Mushrooms are often considered a healthy addition to diets due to their low calorie content and rich nutrient profile, but their impact on acid reflux can vary depending on individual tolerance. While mushrooms themselves are not inherently acidic, they can sometimes trigger symptoms in people with gastroesophageal reflux disease (GERD) or sensitive stomachs, particularly if consumed in large quantities or when combined with other trigger foods. Certain varieties, like shiitake or portobello, may be better tolerated than others, and preparation methods—such as grilling or sautéing—can also influence their effect on digestion. For those prone to acid reflux, it’s advisable to monitor how mushrooms affect symptoms and consider portion control or pairing them with alkaline foods to minimize discomfort.
| Characteristics | Values |
|---|---|
| Impact on Acid Reflux | Generally considered neutral or beneficial |
| Acidity Level | Low in acidity, unlikely to trigger reflux |
| Fiber Content | High in fiber, which can aid digestion and reduce reflux symptoms |
| Prebiotic Properties | Contains prebiotics that promote gut health, potentially reducing reflux |
| Fat Content | Low in fat, less likely to relax the lower esophageal sphincter (LES) |
| Common Triggers | Not typically listed as a common trigger for acid reflux |
| Individual Tolerance | Varies; some individuals may still experience discomfort |
| Preparation Methods | Grilled or steamed mushrooms are better than fried, which can increase fat content |
| Portion Size | Large portions may cause discomfort in sensitive individuals |
| Overall Recommendation | Safe for most people with acid reflux when consumed in moderation |
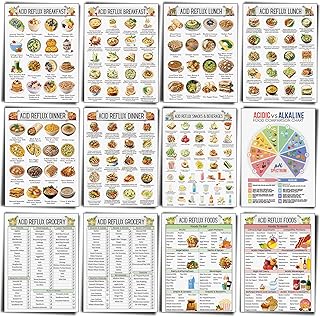
Explore related products
What You'll Learn

Mushroom types and acid reflux impact
Mushrooms, with their diverse varieties and nutritional profiles, can have varying impacts on acid reflux, making it essential to distinguish between types. For instance, Shiitake mushrooms are often recommended for their anti-inflammatory properties, which may help soothe the esophageal lining. However, portobello mushrooms, when cooked with high-fat oils or butter, can exacerbate acid reflux symptoms due to their tendency to relax the lower esophageal sphincter. Understanding these differences allows individuals to make informed choices, ensuring mushrooms complement rather than complicate their diet.
When considering button mushrooms, their mild flavor and low acidity make them a safer option for acid reflux sufferers. They are rich in fiber, which aids digestion, but should be consumed in moderation—a 1-cup serving (about 70g) is ideal. Conversely, cremini mushrooms, though similar in appearance, have a slightly earthier taste and denser texture, which may trigger discomfort in sensitive individuals. Pairing them with alkaline vegetables like spinach or zucchini can help balance their potential acidity.
For those exploring oyster mushrooms, their delicate texture and high protein content make them a nutritious addition to acid reflux-friendly meals. However, their preparation is key: steaming or sautéing with minimal oil is best, as frying can increase fat content and worsen symptoms. Enoki mushrooms, with their crunchy texture, are another low-acid option, but their long, thin strands can sometimes irritate the throat if not chewed thoroughly. Incorporating them into soups or stir-fries can mitigate this risk.
A comparative analysis reveals that reishi mushrooms, often consumed in supplement form (500–1,000 mg daily), may indirectly benefit acid reflux by reducing stress and inflammation, common triggers for symptoms. However, their bitter taste and potential interactions with medications warrant caution. On the other hand, lion’s mane mushrooms, known for their cognitive benefits, are generally well-tolerated but should be avoided in large doses (over 1,000 mg daily) to prevent digestive upset.
In practical terms, individuals with acid reflux should experiment with small portions of different mushroom types to gauge their tolerance. For example, starting with ½ cup of cooked mushrooms per meal and gradually increasing can help identify triggers. Pairing mushrooms with herbs like ginger or turmeric, known for their digestive benefits, can further enhance their compatibility with acid reflux diets. By tailoring mushroom consumption to individual needs, sufferers can enjoy their nutritional benefits without aggravating symptoms.
Are Brown Mushrooms Toxic to Dogs? A Pet Owner's Guide
You may want to see also

Cooking methods to reduce reflux risk
Mushrooms, often celebrated for their umami flavor and nutritional benefits, are generally considered neutral or even beneficial for acid reflux sufferers when prepared mindfully. However, cooking methods can either exacerbate or alleviate symptoms. High-heat techniques like frying or grilling mushrooms in oil can trigger reflux by increasing stomach acidity and relaxing the lower esophageal sphincter. Instead, opt for gentler methods that retain their natural properties while minimizing irritants.
Steaming or boiling mushrooms is an excellent alternative. These methods require minimal added fat and preserve their water-soluble nutrients, such as B vitamins and antioxidants, without introducing reflux triggers. For instance, simmering mushrooms in a low-sodium broth for 10–15 minutes not only enhances their flavor but also creates a soothing, easy-to-digest dish. Pair them with reflux-friendly ingredients like spinach or zucchini for a balanced meal.
Another effective technique is sautéing mushrooms with a small amount of low-acid liquid, such as almond milk or vegetable stock, instead of oil. Use a non-stick pan over medium heat to avoid sticking, and cook until they release their moisture and soften. This method reduces fat content while maintaining their texture and flavor. For added benefit, incorporate herbs like ginger or fennel, which are known to soothe the digestive system.
Roasting mushrooms at a moderate temperature (350°F/175°C) is also reflux-friendly when done correctly. Toss them with a light coating of olive oil or avocado oil spray, spread them on a baking sheet, and roast for 20–25 minutes until tender. Avoid overcrowding the pan, as this can lead to steaming instead of roasting, altering their texture. Serve roasted mushrooms as a side or mix them into whole-grain dishes for a fiber-rich, reflux-safe option.
Lastly, consider incorporating mushrooms into reflux-friendly recipes like soups or stews. Slow-cooking them in a tomato-free vegetable broth with ingredients like carrots, celery, and quinoa creates a nourishing meal that’s gentle on the stomach. Avoid adding garlic or onions, common reflux triggers, and season with mild spices like turmeric or cumin instead. By choosing these cooking methods, you can enjoy mushrooms without aggravating acid reflux symptoms.
Utah's Brown Grass Mushrooms: Are They Harmful to Dogs?
You may want to see also

Portion sizes and symptom severity
Mushrooms, often celebrated for their nutritional benefits, can be a double-edged sword for individuals managing acid reflux. While they are low in fat and rich in fiber, their impact on symptoms varies significantly with portion size. Consuming a small serving, such as ½ cup of cooked mushrooms, is unlikely to trigger discomfort for most people. However, larger portions, like a full cup or more, can increase the risk of symptoms due to their fermentable fiber content, which may relax the lower esophageal sphincter or promote gas production.
Consider this scenario: a 30-year-old with mild acid reflux adds ¼ cup of sautéed mushrooms to their omelet for breakfast. This modest portion is unlikely to cause issues. In contrast, a 50-year-old with chronic GERD who consumes a mushroom-heavy risotto (2+ cups) for dinner may experience heartburn or regurgitation within hours. The key takeaway is that portion control is critical. Limiting mushroom intake to ½ cup per meal, especially when combined with other low-acid foods, can help mitigate risks while allowing you to enjoy their nutritional benefits.
For those experimenting with mushrooms, start with a ¼ cup serving and monitor symptoms over 2–3 hours. If no discomfort arises, gradually increase to ½ cup in subsequent meals. Pairing mushrooms with alkaline foods like spinach or quinoa can further reduce acidity. Avoid high-fat cooking methods, such as frying in butter, as these exacerbate reflux. Instead, opt for steaming, grilling, or sautéing in minimal olive oil.
Age and overall health play a role in tolerance. Younger adults with occasional reflux may handle slightly larger portions than older individuals or those with severe GERD. Pregnant women, who are more prone to acid reflux, should adhere strictly to smaller servings. Always consult a healthcare provider if symptoms persist despite dietary adjustments.
In summary, mushrooms are not inherently bad for acid reflux, but their impact hinges on portion size and preparation. Stick to ½ cup or less per meal, choose low-fat cooking methods, and monitor your body’s response. With mindful consumption, mushrooms can remain a nutritious addition to your diet without aggravating symptoms.
Mushrooms and IBS: Are They a Trigger or Safe to Eat?
You may want to see also
Explore related products

Individual tolerance variations in patients
Mushrooms, often celebrated for their nutritional benefits, can provoke varying responses in individuals with acid reflux, underscoring the importance of understanding personal tolerance levels. While some patients report no adverse effects, others experience heightened symptoms after consumption, suggesting a spectrum of sensitivity. This variability is influenced by factors such as mushroom type, preparation method, and individual digestive health. For instance, shiitake mushrooms, rich in umami flavor, may trigger reflux in sensitive individuals due to their natural glutamate content, while milder varieties like button mushrooms are often better tolerated. Recognizing these nuances is crucial for tailoring dietary choices to manage acid reflux effectively.
Analyzing the role of portion size and frequency reveals further insights into tolerance variations. Consuming large quantities of mushrooms in a single sitting, say 1–2 cups, can overwhelm the digestive system, potentially exacerbating acid reflux symptoms. Conversely, smaller portions, such as ½ cup, integrated into a balanced meal, may be well-tolerated by some. Age and overall health also play a role; older adults or those with pre-existing gastrointestinal conditions may exhibit lower tolerance levels. A practical approach is to start with minimal servings and gradually increase while monitoring symptoms, allowing individuals to identify their threshold without unnecessary discomfort.
Persuasive evidence suggests that preparation methods can significantly impact mushroom tolerance in acid reflux patients. Raw mushrooms, for example, contain chitin, a fibrous substance that can be difficult to digest, potentially triggering reflux. Cooking mushrooms, however, breaks down chitin, making them easier on the stomach. Sautéing or steaming mushrooms instead of frying them reduces the addition of fats that can relax the lower esophageal sphincter, a common reflux trigger. Adopting such cooking techniques can make mushrooms a more viable option for those with sensitive digestive systems, bridging the gap between avoidance and enjoyment.
Comparing individual responses to mushrooms highlights the need for personalized dietary strategies in managing acid reflux. While one person might tolerate mushrooms in soups or stir-fries, another may find them problematic even in small amounts. Keeping a food diary can be an effective tool for tracking symptoms and identifying patterns. For instance, noting whether symptoms occur after consuming mushrooms in a specific dish or at a particular time of day can provide valuable clues. This data-driven approach empowers individuals to make informed decisions, ensuring that dietary choices align with their unique tolerance levels.
Descriptive accounts from patients further illustrate the complexity of mushroom tolerance in acid reflux management. Some individuals report that pairing mushrooms with alkaline foods, such as spinach or broccoli, helps mitigate potential reflux. Others find that avoiding mushrooms during evening meals reduces nighttime symptoms. These anecdotal strategies, while not universally applicable, offer practical insights into managing tolerance variations. By experimenting with timing, combinations, and portion sizes, individuals can navigate their dietary preferences while minimizing acid reflux discomfort, turning mushrooms from a potential trigger into a manageable, nutrient-rich addition to their meals.
Are Burnt Mushrooms Harmful? Health Risks and Safe Cooking Tips
You may want to see also

Mushroom alternatives for reflux sufferers
Mushrooms, while nutrient-dense, can trigger acid reflux in some individuals due to their high histamine and fermentable oligosaccharide content. For reflux sufferers seeking umami depth or meaty texture without discomfort, several alternatives offer culinary versatility and digestive peace. Here’s a practical guide to substituting mushrooms effectively.
Step 1: Choose Low-FODMAP Vegetables for Texture
Zucchini, eggplant, and hearts of palm mimic mushrooms’ chewiness when sliced or roasted. For example, marinate zucchini rounds in tamari (a low-histamine soy sauce alternative) and balsamic vinegar, then bake at 400°F for 20 minutes. These options are gentle on the gut, as they fall within the low-FODMAP diet framework recommended for reflux and IBS management. Avoid large portions, as even low-FODMAP foods can provoke symptoms when overeaten.
Step 2: Leverage Umami-Rich, Reflux-Friendly Ingredients
Kombu seaweed, roasted red peppers, and nutritional yeast provide mushroom-like savoriness without histamine or fermentable fibers. Add a 2-inch strip of kombu to soups or broths during cooking to enhance flavor, then remove before serving. Nutritional yeast, sprinkled in 1–2 tablespoon increments, works well in sauces or as a popcorn topping. These alternatives are particularly beneficial for vegans or those reducing meat intake.
Step 3: Experiment with Protein Substitutes
For dishes requiring a meaty substitute, opt for tempeh made from soybeans (lower in FODMAPs than chickpea-based options) or seitan, provided gluten is tolerated. Pan-fry tempeh cubes in avocado oil (high smoke point, reflux-friendly) with garlic-infused oil (safer than raw garlic) for a mushroom-like bite. Note: Introduce new proteins gradually, as some individuals may react to their natural compounds.
Cautionary Notes and Final Tips
While these alternatives are generally safer, individual tolerance varies. Track symptoms using a food diary to identify personal triggers. Pair alternatives with alkaline foods like spinach or ginger tea to further soothe the esophagus. For children or elderly individuals, prioritize softer textures (e.g., blended roasted peppers) to minimize swallowing discomfort. Always consult a dietitian when making significant dietary changes, especially for chronic conditions.
By strategically substituting mushrooms with these alternatives, reflux sufferers can reclaim culinary enjoyment without compromising digestive health. Experimentation and mindful portioning are key to finding what works best for your body.
Spotting Spoiled Mushrooms: Signs Your Fungi Have Gone Bad
You may want to see also
Frequently asked questions
Mushrooms are generally considered safe for acid reflux sufferers, as they are low in fat and acidity. However, individual tolerance varies, so monitor how your body reacts.
While mushrooms are unlikely to trigger acid reflux, certain preparations (e.g., fried or heavily seasoned) may worsen symptoms. Stick to plain, cooked mushrooms for best results.
Most common mushrooms (button, cremini, shiitake) are safe, but some people may react to wild or exotic varieties. Start with small portions to test tolerance.
Mushrooms are not typically a trigger for GERD, but if you notice discomfort after eating them, consider reducing portion sizes or avoiding them altogether. Consult a doctor if symptoms persist.