Psychedelic mushrooms, containing the active compound psilocybin, have garnered significant attention in recent years as a potential treatment for depression, particularly for individuals who have not responded to traditional therapies. Research suggests that psilocybin may alleviate symptoms of depression by promoting neuroplasticity, resetting abnormal brain activity patterns, and fostering profound emotional and psychological insights. Clinical trials have shown promising results, with many participants reporting sustained improvements in mood and well-being after just one or two supervised sessions. However, the use of psychedelic mushrooms for depression remains highly regulated and is typically conducted in controlled, therapeutic settings due to their potent psychoactive effects and potential risks. As the scientific community continues to explore this novel approach, the question of whether psychedelic mushrooms are a viable and safe treatment for depression remains a topic of both hope and cautious optimism.
| Characteristics | Values |
|---|---|
| Mechanism of Action | Psilocybin (active compound) interacts with serotonin receptors in the brain, particularly the 5-HT2A receptor, leading to altered brain connectivity and neuroplasticity. |
| Clinical Trials | Recent studies (e.g., Johns Hopkins, Imperial College London) show significant reduction in depression symptoms, often after just one or two doses, with effects lasting weeks to months. |
| Efficacy | High efficacy in treatment-resistant depression (TRD), with remission rates of 50-70% in controlled trials. |
| Duration of Effects | Acute effects last 4-6 hours, but therapeutic benefits can persist for weeks or months after a single dose. |
| Safety Profile | Generally safe when administered in controlled settings; rare adverse effects include transient anxiety, confusion, or mild increases in blood pressure/heart rate. |
| Legal Status | Illegal in most countries, but decriminalized or legalized for medical/therapeutic use in some regions (e.g., Oregon, Canada, Australia). |
| Psychological Support | Requires supervised administration with psychological support before, during, and after sessions for optimal outcomes. |
| Long-term Effects | Limited data on long-term effects, but no evidence of addiction or cognitive impairment in therapeutic use. |
| Comparative Effectiveness | More rapid and sustained effects compared to traditional antidepressants, which often take weeks to work and may have side effects. |
| Patient Population | Most effective for treatment-resistant depression, end-of-life anxiety, and major depressive disorder (MDD). |
| Regulatory Approval | Not yet FDA-approved, but designated as a "breakthrough therapy" for depression and PTSD, accelerating research and potential approval. |
| Public Perception | Growing acceptance due to promising research, though stigma and legal barriers remain significant challenges. |
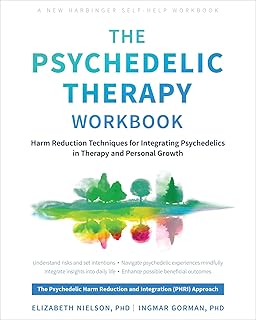
Explore related products
What You'll Learn
- Mechanism of Action: How psilocybin affects brain chemistry to alleviate depressive symptoms
- Clinical Trial Results: Evidence from studies on psychedelic mushrooms for depression treatment
- Potential Risks: Side effects and dangers associated with using mushrooms for mental health
- Legal and Ethical Issues: Current laws and moral debates surrounding psychedelic therapy
- Long-Term Effects: Sustained benefits or drawbacks of mushroom use for depression

Mechanism of Action: How psilocybin affects brain chemistry to alleviate depressive symptoms
Psilocybin, the active compound in psychedelic mushrooms, exerts its antidepressant effects by fundamentally altering brain chemistry and connectivity. Unlike traditional antidepressants, which primarily target serotonin reuptake, psilocybin acts as a serotonin 2A receptor agonist. This activation triggers a cascade of neurochemical changes, including increased glutamate release and brain-derived neurotrophic factor (BDNF) production. BDNF promotes neuronal growth and plasticity, potentially reversing the atrophy often observed in depressed brains. A single dose of 20–30 mg psilocybin, administered in a controlled setting, can induce these changes, with effects lasting weeks to months.
Consider the brain as a city grid: depression often resembles traffic jams and blocked routes, with rigid thought patterns and emotional stagnation. Psilocybin acts like a city planner, temporarily dismantling old pathways and fostering new connections. Functional MRI studies show that it reduces activity in the default mode network (DMN), a brain region hyperactive in depression, linked to rumination and self-criticism. Simultaneously, it increases connectivity between previously isolated brain areas, enabling novel perspectives and emotional processing. This "reset" effect is akin to defragmenting a computer hard drive, optimizing function and reducing depressive symptoms.
However, the mechanism isn’t without nuance. The intensity of the psychedelic experience, often referred to as the "trip," correlates with therapeutic outcomes. A 2016 study published in *Scientific Reports* found that participants who reported more profound mystical experiences during psilocybin sessions showed greater reductions in depression scores. This suggests that the subjective experience, not just the neurochemical changes, plays a critical role. For this reason, clinical trials emphasize psychological preparation and supportive therapy before and after dosing, ensuring patients can integrate the experience constructively.
Practical considerations are essential for safety and efficacy. Psilocybin therapy is not a DIY solution; it requires medical supervision due to potential risks like anxiety or psychosis, especially in individuals with a history of mental health disorders. Dosage precision is critical—microdosing (0.1–0.5 mg) lacks sufficient evidence for depression, while macrodoses (20–30 mg) are reserved for clinical settings. Patients should avoid self-medication, as improper use can exacerbate symptoms. Instead, seek out clinical trials or jurisdictions where psilocybin therapy is legally accessible, such as Oregon’s regulated programs.
In summary, psilocybin’s antidepressant mechanism hinges on its ability to rewire brain networks, promote neuroplasticity, and facilitate profound emotional experiences. While promising, its use demands caution, precision, and professional guidance. As research advances, this unique approach could redefine depression treatment, offering hope to those resistant to conventional therapies.
Exploring Tasty Mushroom Alternatives: Creative Substitutes for Every Recipe
You may want to see also

Clinical Trial Results: Evidence from studies on psychedelic mushrooms for depression treatment
Recent clinical trials have shed light on the potential of psychedelic mushrooms, specifically psilocybin, as a treatment for depression. A landmark study published in *JAMA Psychiatry* (2021) found that a single 25-milligram dose of psilocybin, administered in a controlled therapeutic setting, led to significant reductions in depression symptoms for up to 12 weeks in 75% of participants. These individuals, who had treatment-resistant depression, showed rapid and sustained improvement, outperforming traditional antidepressants in terms of speed and efficacy. The study underscores the importance of set and setting—participants received psychological support before, during, and after the session, highlighting the need for a structured environment to maximize benefits.
Another pivotal trial, conducted by Imperial College London, compared psilocybin therapy to conventional antidepressants like escitalopram. Over a six-week period, participants receiving two doses of 25 milligrams of psilocybin, spaced three weeks apart, reported greater reductions in depressive symptoms compared to those on daily escitalopram. Notably, the psilocybin group also experienced fewer side effects, such as emotional numbing, which are commonly associated with SSRIs. This comparative analysis suggests that psychedelic mushrooms could offer a more holistic and immediate solution for depression, particularly for those who have not responded to standard treatments.
However, not all trials have yielded uniformly positive results. A 2022 study in *Nature Medicine* found that while 60% of participants experienced significant symptom relief after a 20-milligram dose of psilocybin, 20% reported transient anxiety or confusion during the session. These adverse effects, though short-lived, emphasize the need for careful patient selection and monitoring. Researchers recommend excluding individuals with a history of psychosis or severe anxiety disorders, as they may be more susceptible to negative reactions. Additionally, the therapeutic environment must be meticulously designed to ensure safety and comfort.
Practical implementation of psilocybin therapy requires strict protocols. Dosage is critical—studies typically use 20 to 25 milligrams, administered orally in a capsule. Sessions last 6 to 8 hours, with two therapists present to guide the experience. Patients are advised to avoid food for 6 hours beforehand and to refrain from alcohol or other substances for 24 hours prior. Post-session integration, involving follow-up therapy to process the experience, is essential for long-term benefits. While not yet widely available, these trials provide a roadmap for future clinical practice, offering hope for a paradigm shift in depression treatment.
In conclusion, clinical trial results demonstrate that psychedelic mushrooms, when used in controlled settings, can be a powerful tool for treating depression. The evidence is compelling but not without caveats. As research progresses, the focus must remain on safety, standardization, and accessibility to ensure this innovative treatment reaches those who need it most. For now, psilocybin therapy stands as a promising alternative for individuals who have exhausted other options, offering a glimpse into a new era of mental health care.
Mushrooms in Compost: Benefits, Uses, and Eco-Friendly Gardening Tips
You may want to see also

Potential Risks: Side effects and dangers associated with using mushrooms for mental health
While psychedelic mushrooms have shown promise in treating depression, their use is not without risks. One of the most immediate concerns is the unpredictability of the experience. Psilocybin, the active compound in these mushrooms, can induce intense hallucinations, altered perceptions of time, and profound emotional shifts. For individuals with a history of psychosis or schizophrenia, these effects can exacerbate symptoms, potentially leading to long-term psychological distress. Even in healthy individuals, a "bad trip" can occur, characterized by overwhelming anxiety, paranoia, or fear, which may persist beyond the acute experience and contribute to lasting emotional trauma.
Dosage plays a critical role in managing these risks. A typical therapeutic dose ranges from 0.2 to 0.4 grams of dried mushrooms per kilogram of body weight, but even small variations can lead to vastly different outcomes. Overconsumption can result in severe disorientation, panic attacks, or even psychotic episodes. Without proper medical supervision, users may inadvertently ingest harmful amounts, particularly if they are unfamiliar with the potency of the mushrooms they are consuming. This lack of standardization is a significant danger, as it increases the likelihood of adverse reactions.
Another often-overlooked risk is the potential for physical harm during a psychedelic experience. Users may lose touch with reality, leading to accidents or self-injury. For example, someone under the influence might attempt to walk through a window, believing it to be a portal, or neglect basic safety precautions. This is particularly concerning for individuals using mushrooms alone or in unsupportive environments. Additionally, psilocybin can cause increased heart rate and blood pressure, posing risks for those with cardiovascular conditions or hypertension.
Long-term effects are still not fully understood, but there are concerns about the impact of repeated use on brain function. While studies suggest that occasional use may not lead to addiction, frequent consumption could potentially disrupt neural pathways, particularly in younger individuals whose brains are still developing. Adolescents and young adults under 25 are especially vulnerable, as their prefrontal cortex—responsible for decision-making and emotional regulation—is not yet fully mature. This age group should exercise extreme caution, as the risks may outweigh any potential benefits.
Finally, the legal and social consequences of using psychedelic mushrooms cannot be ignored. In most countries, psilocybin is classified as a Schedule I controlled substance, making its possession or distribution illegal. Arrests, fines, and criminal records can have lasting impacts on employment, education, and personal relationships. Even in regions where decriminalization efforts are underway, the lack of regulatory oversight means users must navigate these risks independently. For those considering mushrooms as a treatment for depression, consulting with a healthcare professional and exploring legal, supervised options is essential to minimize harm.
Mushrooms and Fiber: Unlocking Their Digestive Health Benefits
You may want to see also
Explore related products

Legal and Ethical Issues: Current laws and moral debates surrounding psychedelic therapy
Psychedelic mushrooms, primarily containing psilocybin, have shown promise in treating depression, but their legal and ethical landscape remains complex. In most countries, including the United States, psilocybin is classified as a Schedule I substance, deemed to have no accepted medical use and a high potential for abuse. This classification severely restricts research and clinical application, despite growing evidence of its therapeutic benefits. For instance, studies like those conducted by Johns Hopkins University have demonstrated that controlled doses of psilocybin (typically 20–30 mg) can produce significant and lasting reductions in depressive symptoms, often after just one or two sessions. However, the legal framework often lags behind scientific progress, leaving patients and practitioners in a regulatory gray area.
Ethically, the use of psychedelic therapy raises questions about consent, safety, and accessibility. Patients must be fully informed of the potential risks, such as psychological distress or re-emergence of trauma, which requires rigorous screening and preparation. For example, individuals with a personal or family history of psychosis are generally excluded from trials due to heightened risks. Additionally, the cost and availability of treatment pose ethical dilemmas. Clinical trials and therapy sessions can be prohibitively expensive, limiting access to those with financial means. This disparity raises concerns about equity, as marginalized populations, who often bear a disproportionate burden of mental health issues, may be left behind.
The moral debate also extends to the role of therapists and facilitators. Unlike traditional pharmaceuticals, psychedelic therapy relies heavily on the therapeutic relationship and setting. Practitioners must be trained to create a safe, supportive environment and guide patients through potentially intense experiences. This demands a high level of skill and ethical responsibility, as misuse or negligence could lead to harm. For instance, improper dosing or inadequate preparation can result in adverse reactions, undermining the therapy’s potential benefits. Standardizing these practices while respecting the unique nature of psychedelic experiences remains a challenge.
Comparatively, countries like Canada and the Netherlands have adopted more progressive approaches, allowing limited access to psilocybin therapy under compassionate use or right-to-try frameworks. These examples highlight the need for flexible legal systems that balance safety with innovation. In the U.S., cities like Denver and Oregon have decriminalized psilocybin or legalized its therapeutic use, signaling a shift in public and political attitudes. However, federal law remains a significant barrier, creating a patchwork of regulations that complicate research and treatment.
Practically, individuals considering psychedelic therapy should prioritize safety and legality. Joining clinical trials, where available, offers a regulated environment with expert oversight. For those in regions where psilocybin remains illegal, advocating for policy change through grassroots movements or supporting research organizations can help drive progress. Ultimately, the legal and ethical issues surrounding psychedelic therapy reflect broader tensions between innovation, regulation, and equity. Addressing these challenges requires collaboration among lawmakers, researchers, and communities to ensure that this promising treatment is accessible, safe, and just.
Mushrooms in Your Yard: Benefits, Myths, and Gardening Tips
You may want to see also

Long-Term Effects: Sustained benefits or drawbacks of mushroom use for depression
The long-term effects of psychedelic mushroom use for depression remain a subject of intense scientific inquiry, with emerging evidence suggesting both sustained benefits and potential drawbacks. Clinical trials have shown that a single high dose of psilocybin (25–30 mg) administered in a controlled therapeutic setting can lead to significant reductions in depressive symptoms for up to 12 months in some individuals. These effects are often accompanied by reports of increased emotional openness, improved relationships, and a heightened sense of purpose. However, the durability of these benefits varies widely, with approximately 30–50% of participants experiencing a relapse into depressive episodes within the first year post-treatment.
One of the most compelling aspects of psilocybin therapy is its ability to "reset" dysfunctional brain patterns associated with depression. Neuroimaging studies have demonstrated that psilocybin reduces activity in the default mode network (DMN), a brain network linked to rumination and self-critical thoughts. This "reset" effect can persist for months, offering a unique advantage over traditional antidepressants, which often require daily use and may lose efficacy over time. However, this neuroplasticity also raises concerns about long-term changes in brain function, particularly in individuals with pre-existing mental health conditions or those who use mushrooms outside of a controlled setting.
Despite the promise, long-term drawbacks cannot be overlooked. Repeated use of psychedelic mushrooms, especially at high doses or without therapeutic guidance, may lead to psychological distress, including anxiety, paranoia, or persistent perceptual changes. A small subset of users (approximately 1–2%) report experiencing "flashbacks" or hallucinogen persisting perception disorder (HPPD), where visual disturbances or emotional instability persist long after the drug has left the system. Additionally, the lack of standardized dosing and the variability in individual responses make it difficult to predict who will benefit and who may be at risk for adverse effects.
For those considering psilocybin as a treatment for depression, practical steps can mitigate risks. First, ensure treatment is administered in a clinical trial or by a trained professional, as the therapeutic setting plays a critical role in outcomes. Second, start with a low dose (e.g., 10–15 mg) to gauge sensitivity and minimize the risk of overwhelming experiences. Third, integrate the experience with ongoing psychotherapy to process insights and sustain behavioral changes. Finally, avoid self-medication, as unsupervised use increases the likelihood of adverse effects and reduces the potential for long-term benefits.
In conclusion, while psychedelic mushrooms show remarkable potential for treating depression, their long-term effects are a double-edged sword. Sustained benefits in mood, cognition, and quality of life are possible, but they are not guaranteed and must be balanced against the risks of psychological harm. As research progresses, a nuanced understanding of who stands to benefit most—and under what conditions—will be critical to maximizing the therapeutic potential of these powerful substances.
Ryze Mushroom Coffee: A Healthy Choice for Type 2 Diabetics?
You may want to see also
Frequently asked questions
While research is promising, psychedelic mushrooms (containing psilocybin) are not yet a fully proven or widely accepted treatment for depression. Clinical trials show potential benefits, but more research is needed for FDA approval.
Psilocybin in mushrooms is believed to reset brain circuits associated with depression by promoting neuroplasticity and altering serotonin receptors, leading to improved mood and reduced symptoms.
When used in controlled, therapeutic settings with professional guidance, psychedelic mushrooms are generally considered safe. However, they can cause psychological distress or worsen mental health in unsupervised use.
No, psychedelic mushrooms are not suitable for everyone. Individuals with a history of psychosis, severe mental health conditions, or certain medical issues should avoid them due to potential risks.
Psilocybin mushrooms remain illegal in most countries, though some regions (e.g., Oregon, Colorado) have decriminalized or approved them for therapeutic use under strict regulations. Always check local laws.