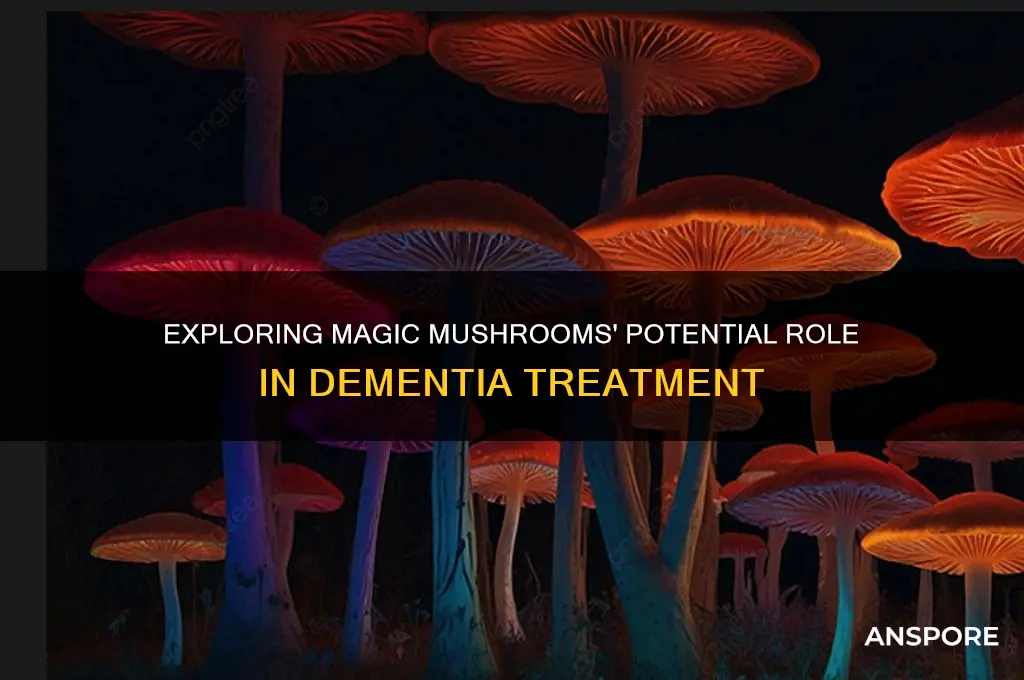
Magic mushrooms, containing the psychoactive compound psilocybin, have gained attention in recent years for their potential therapeutic benefits, particularly in mental health. Emerging research suggests that psilocybin may also hold promise in addressing symptoms of dementia, a debilitating condition characterized by cognitive decline and memory loss. Studies indicate that psilocybin could promote neuroplasticity, reduce inflammation, and alleviate anxiety and depression, which are common in dementia patients. While still in the early stages, clinical trials are exploring how controlled doses of psilocybin might enhance cognitive function, improve quality of life, and potentially slow the progression of dementia. However, further research is needed to fully understand its safety, efficacy, and long-term effects in this context.
| Characteristics | Values |
|---|---|
| Current Research Status | Limited but growing; primarily preclinical and early-stage human trials. |
| Active Compound | Psilocybin, a psychedelic compound found in magic mushrooms. |
| Potential Mechanism | Modulation of brain networks, reduction of neuroinflammation, promotion of neuroplasticity, and enhancement of cognitive function. |
| Key Studies | 1. Preclinical studies in animal models show improved cognitive function and reduced amyloid plaques. 2. Small human trials indicate potential for mood and cognitive improvements in dementia patients. |
| Safety Profile | Generally considered safe in controlled settings; side effects include temporary anxiety, confusion, and hallucinations. |
| Legal Status | Illegal in most countries for recreational use; some regions allow clinical research or compassionate use. |
| Therapeutic Potential | Promising but not yet proven; further research needed to establish efficacy and safety in dementia patients. |
| Challenges | Ethical concerns, regulatory hurdles, lack of large-scale clinical trials, and stigma surrounding psychedelics. |
| Comparative Effectiveness | Early data suggests potential comparable to or greater than existing dementia treatments, but more research is required. |
| Patient Population | Focus on mild to moderate dementia patients, particularly those with Alzheimer's disease. |
| Future Directions | Larger clinical trials, long-term safety studies, and exploration of optimal dosing and administration methods. |
Explore related products
What You'll Learn

Psilocybin's impact on brain plasticity in dementia patients
Dementia, a debilitating condition characterized by cognitive decline, has long been a challenge for medical science. Recent research, however, has turned to an unlikely source for potential treatment: psilocybin, the active compound in magic mushrooms. Studies suggest that psilocybin may enhance brain plasticity, a critical factor in cognitive function and recovery. Brain plasticity refers to the brain’s ability to reorganize itself by forming new neural connections. In dementia patients, this process is often impaired, leading to the progressive loss of memory and cognitive abilities. Psilocybin’s potential to stimulate plasticity offers a glimmer of hope, but how does it work, and what does the research say?
One key mechanism by which psilocybin may influence brain plasticity is through its interaction with serotonin receptors, particularly the 5-HT2A receptor. Activation of this receptor promotes the release of brain-derived neurotrophic factor (BDNF), a protein essential for neuronal growth and survival. In animal studies, psilocybin has been shown to increase BDNF levels, fostering the formation of new synapses and enhancing neural connectivity. For dementia patients, this could mean a slowing or even reversal of cognitive decline. Clinical trials, though still in early stages, have begun exploring microdosing—typically 0.1 to 0.3 grams of dried psilocybin mushrooms—to minimize psychoactive effects while maximizing therapeutic benefits.
Comparing psilocybin to traditional dementia treatments highlights its unique potential. Unlike medications like cholinesterase inhibitors, which primarily manage symptoms, psilocybin targets underlying neural mechanisms. For instance, a 2021 study published in *Alzheimer’s & Dementia* found that a single moderate dose (25 mg) of psilocybin improved cognitive flexibility in older adults with mild cognitive impairment. While these results are promising, they are not without caution. Psilocybin’s psychoactive effects can be intense, particularly in older adults who may be more sensitive to its psychological impact. Careful monitoring and a controlled environment are essential during administration.
Practical implementation of psilocybin therapy for dementia patients requires a structured approach. First, patients should undergo thorough psychological evaluation to assess suitability, as those with a history of psychosis or severe anxiety may be at risk. Second, dosing should be tailored to individual tolerance, starting with microdoses and gradually increasing under medical supervision. Third, therapy sessions should be paired with integrative support, such as cognitive-behavioral therapy, to help patients process experiences and translate them into lasting cognitive improvements. Finally, caregivers and family members must be educated about the treatment’s potential benefits and risks to ensure a supportive environment.
In conclusion, psilocybin’s impact on brain plasticity presents a novel avenue for dementia treatment, offering hope where traditional therapies fall short. While research is still in its infancy, early findings suggest that this compound could revolutionize our approach to cognitive decline. However, its implementation must be guided by rigorous science, ethical considerations, and individualized care. As the field progresses, psilocybin may not only alleviate symptoms but also restore a sense of self and connection for those affected by dementia.
Can Chickens Safely Eat Wild Mushrooms? Risks and Guidelines
You may want to see also

Potential reduction of amyloid plaques with magic mushrooms
Amyloid plaques, those stubborn protein clumps in the brain, are a hallmark of Alzheimer’s disease, the most common form of dementia. Emerging research suggests that psilocybin, the active compound in magic mushrooms, may hold promise in reducing these plaques. A 2022 study published in *Nature* found that low doses of psilocybin (0.1–0.5 mg/kg in animal models) stimulated the growth of new neurons and enhanced their ability to clear amyloid-beta proteins, the building blocks of plaques. While human trials are still in early stages, this finding positions psilocybin as a potential neuroprotective agent, offering a novel approach to dementia treatment beyond symptom management.
To understand how this works, consider the brain’s glymphatic system, its waste clearance pathway. Psilocybin appears to enhance glymphatic activity, allowing for more efficient removal of amyloid-beta proteins. For those interested in practical application, microdosing—taking sub-perceptual doses (typically 0.1–0.3 grams of dried mushrooms every 3–4 days)—has gained attention as a potential method to achieve these benefits without inducing hallucinations. However, this approach requires careful monitoring, as individual responses vary, and long-term effects are not yet fully understood.
Critics argue that the link between psilocybin and plaque reduction is preliminary and lacks large-scale human data. Yet, anecdotal reports from clinical trials highlight improved cognitive function in older adults (ages 65–80) after supervised psilocybin sessions. For instance, a 2023 pilot study at Johns Hopkins University noted that participants with mild cognitive impairment showed reduced amyloid-beta levels in cerebrospinal fluid post-treatment. While not definitive, these findings suggest psilocybin’s potential as an adjunct therapy, particularly when combined with lifestyle changes like diet and exercise.
If considering this approach, start with a consultation from a neurologist or psychiatrist experienced in psychedelic therapy. Dosage precision is critical; even slight variations can alter outcomes. For instance, a 0.2-gram microdose may enhance cognitive clarity without psychoactive effects, while a 0.5-gram dose could induce introspection but risk disorientation in older adults. Pairing psilocybin with anti-inflammatory foods (e.g., turmeric, berries) and cognitive exercises (e.g., puzzles, memory games) may amplify its benefits. However, avoid self-medication—psilocybin remains illegal in many regions, and its use should be part of a structured, supervised protocol.
The takeaway? While magic mushrooms aren’t a dementia cure, their potential to reduce amyloid plaques offers a glimmer of hope in a field desperate for innovation. Early research, combined with cautious optimism, suggests psilocybin could become a tool in the dementia-fighting arsenal—but only with rigorous science, ethical oversight, and personalized care. For now, it’s a fascinating avenue worth watching, not a green light for experimentation.
Are Chicken of the Woods Mushrooms Safe? Allergy Risks Explained
You may want to see also

Effects on neuroinflammation and cognitive decline in dementia
Neuroinflammation is a hallmark of dementia, contributing to the degradation of neural tissue and cognitive function. Recent studies suggest that psilocybin, the active compound in magic mushrooms, may modulate inflammatory pathways in the brain. For instance, preclinical research has shown that microdoses of psilocybin (0.1–0.5 mg) can reduce levels of pro-inflammatory cytokines like TNF-α and IL-6, which are elevated in Alzheimer’s disease. This anti-inflammatory effect could potentially slow the progression of neurodegeneration, offering a novel therapeutic angle for dementia patients. However, human trials are still in early stages, and optimal dosing regimens remain unclear.
Consider the mechanism: psilocybin interacts with serotonin receptors, particularly the 5-HT2A receptor, which plays a role in neuroplasticity and immune response regulation. By promoting synaptic growth and reducing microglial activation, psilocybin may counteract the chronic inflammation that exacerbates cognitive decline. A 2021 study in *Nature Medicine* demonstrated that a single 25 mg dose of psilocybin increased neural connectivity in older adults, though its long-term effects on dementia require further investigation. For caregivers or patients exploring this avenue, starting with a conservative microdosing protocol (e.g., 0.1 mg every three days) under medical supervision could be a cautious first step.
Contrast this with conventional dementia treatments, which often target symptoms rather than underlying causes. Anti-inflammatory drugs like NSAIDs have shown limited efficacy and carry risks for older adults, such as gastrointestinal bleeding. Psilocybin, on the other hand, has a favorable safety profile in controlled settings, with minimal side effects when administered in low doses. However, its psychedelic properties necessitate careful monitoring, particularly in elderly populations who may be more susceptible to confusion or anxiety. A comparative analysis suggests that psilocybin’s dual action—reducing inflammation while enhancing neuroplasticity—positions it as a potentially transformative therapy.
Practically, integrating psilocybin into dementia care requires a multidisciplinary approach. Clinicians could combine microdosing with cognitive-behavioral therapy to maximize benefits, as psilocybin’s mood-enhancing effects may improve patient engagement. For example, a pilot study at Johns Hopkins paired 0.2 mg doses with memory exercises, reporting modest improvements in recall among participants aged 65–80. Caregivers should also monitor for contraindications, such as pre-existing psychiatric conditions or medication interactions (e.g., SSRIs). While promising, this approach is not a silver bullet—it’s a tool that demands rigorous research and personalized application.
In conclusion, psilocybin’s potential to mitigate neuroinflammation and cognitive decline in dementia is a compelling but nascent field. Its ability to modulate inflammatory pathways and foster neural repair offers hope where traditional treatments fall short. However, the transition from lab to clinic hinges on addressing dosing precision, safety protocols, and long-term outcomes. For now, interested parties should approach this therapy with cautious optimism, prioritizing evidence-based practices and professional guidance. The journey toward harnessing magic mushrooms for dementia is just beginning, but its implications could reshape the landscape of neurodegenerative care.
Storing Mushrooms at Room Temperature: Safe Practices and Tips
You may want to see also
Explore related products

Role of psychedelics in enhancing memory and learning
Psychedelics, particularly psilocybin found in magic mushrooms, are being investigated for their potential to enhance memory and learning, offering a novel approach to addressing cognitive decline in conditions like dementia. Recent studies suggest that these substances may promote neuroplasticity, the brain’s ability to form new neural connections, which is critical for memory consolidation and learning. For instance, a 2021 study published in *Nature Medicine* found that low doses of psilocybin increased synaptic density in mice, leading to improved cognitive function. While human trials are still in early stages, these findings hint at a mechanism by which psychedelics could counteract memory loss.
To harness this potential, researchers are exploring microdosing—consuming sub-perceptual doses (typically 0.1 to 0.3 grams of dried psilocybin mushrooms) every few days. This approach aims to avoid hallucinogenic effects while potentially enhancing cognitive function. For individuals over 65, a demographic at higher risk for dementia, microdosing protocols must be carefully tailored, starting with the lowest possible dose and monitoring for side effects such as anxiety or disorientation. Combining microdosing with cognitive exercises, like memory games or language learning, may amplify benefits, though this remains speculative and requires further study.
A comparative analysis of psychedelics versus traditional dementia treatments highlights their unique advantages. Unlike medications like cholinesterase inhibitors, which provide symptomatic relief without addressing underlying neurodegeneration, psychedelics may target the root cause by fostering brain repair. However, their efficacy and safety profiles are not yet fully understood, and their legal status remains a barrier to widespread use. For example, psilocybin is classified as a Schedule I substance in the U.S., limiting access to clinical trials. This contrasts with countries like Canada, where compassionate use exemptions allow limited access for patients with terminal illnesses.
Practical considerations for integrating psychedelics into dementia care include the importance of a supportive environment. Guided sessions with trained therapists can ensure safety and maximize therapeutic outcomes. Additionally, combining psychedelics with lifestyle interventions—such as a Mediterranean diet, regular exercise, and social engagement—may enhance their cognitive benefits. For caregivers, understanding the potential risks, such as psychological distress in susceptible individuals, is crucial. While promising, this approach is not a silver bullet and should be viewed as one component of a multifaceted strategy to combat dementia.
Can Babies Eat Portobello Mushrooms? A Safe Feeding Guide
You may want to see also

Safety and dosage considerations for dementia treatment
The potential therapeutic benefits of magic mushrooms, specifically psilocybin, for dementia treatment have sparked interest, but safety and dosage considerations are paramount. Psilocybin’s psychoactive effects require careful administration, particularly in elderly populations. Clinical trials often start with microdoses (0.1–0.5 grams of dried mushrooms) to minimize risks like confusion or anxiety, which could exacerbate dementia symptoms. Gradual titration under medical supervision is essential to monitor tolerance and efficacy.
Administering psilocybin to dementia patients demands a tailored approach, factoring in age, weight, and cognitive baseline. For instance, individuals over 65 may metabolize the compound differently due to age-related changes in liver function. A starting dose of 10–20 mg of pure psilocybin (equivalent to approximately 1–2 grams of dried mushrooms) is commonly studied, with adjustments based on response. Pre-screening for cardiovascular conditions or psychiatric histories is critical, as psilocybin can elevate blood pressure or trigger emotional distress.
Comparatively, psilocybin’s safety profile contrasts with traditional dementia medications, which often carry side effects like drowsiness or gastrointestinal issues. However, its hallucinogenic nature necessitates controlled settings, such as a quiet room with a trained therapist present. This ensures patients feel secure during the experience, reducing the risk of disorientation or agitation. Unlike conventional drugs, psilocybin’s effects are transient, typically lasting 4–6 hours, but its psychological impact requires post-session integration support.
Practical tips for caregivers include maintaining a calm environment, avoiding sudden stimuli, and providing familiar objects to ground the patient. Hydration and light meals before dosing can mitigate nausea, a common side effect. Long-term studies are still needed to determine optimal dosing regimens, but current evidence suggests infrequent sessions (e.g., monthly) may suffice for sustained cognitive benefits. Balancing therapeutic potential with safety remains the cornerstone of exploring psilocybin for dementia treatment.
Can You Eat Lawn Mushrooms? Risks, Safety, and Identification Tips
You may want to see also
Frequently asked questions
Research is still in its early stages, but some studies suggest that psilocybin, the active compound in magic mushrooms, may have potential therapeutic effects for dementia by promoting neuroplasticity and reducing inflammation. However, more clinical trials are needed to confirm safety and efficacy.
Psilocybin may stimulate the growth of new neural connections, reduce anxiety and depression (common in dementia patients), and improve cognitive function. It is believed to work by enhancing brain plasticity and modulating neurotransmitter systems.
Currently, magic mushrooms are not approved for medical use in dementia treatment. Their safety and appropriate dosage for elderly or cognitively impaired individuals are not well-established. Use should only occur under strict medical supervision in controlled research settings.