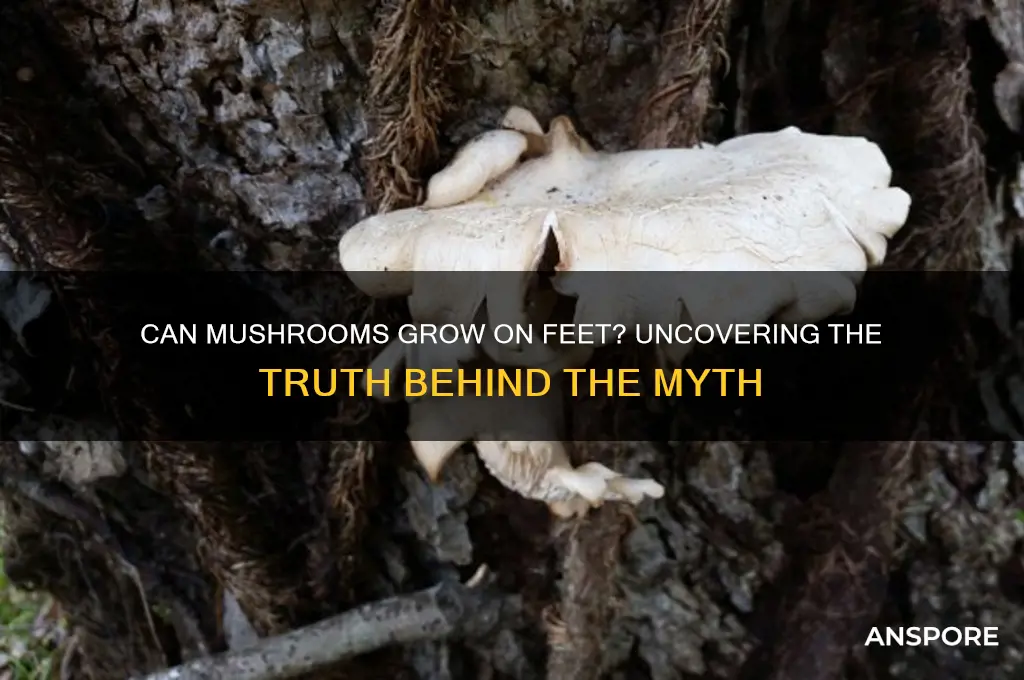
The idea of mushrooms growing on feet may sound like something out of a science fiction novel, but it’s a question rooted in both curiosity and concern. While mushrooms typically thrive in damp, organic environments like soil or decaying wood, the human foot can sometimes create conditions conducive to fungal growth, such as prolonged moisture from sweat or poor hygiene. However, true mushrooms (basidiomycetes) require specific nutrients and conditions not typically found on human skin. What people often mistake for mushrooms on feet are actually fungal infections like athlete’s foot or ringworm, which manifest as rashes, blisters, or discolored patches. Understanding the difference between these infections and actual mushroom growth is essential for proper treatment and peace of mind.
| Characteristics | Values |
|---|---|
| Can mushrooms grow on feet? | No, mushrooms cannot grow on human feet under normal circumstances. |
| Reason | Mushrooms require specific conditions (moisture, organic matter, darkness) that human skin does not provide. |
| Possible Confusion | Skin conditions like dermatophyte infections (e.g., ringworm) or onychomycosis (nail fungus) may resemble mushrooms but are not actual fungi. |
| Myth or Reality | Myth. While fungi can infect skin or nails, mushrooms (fruiting bodies of fungi) do not grow on human feet. |
| Prevention | Maintain foot hygiene, keep feet dry, and avoid walking barefoot in damp areas to prevent fungal infections. |
| Medical Advice | Consult a dermatologist if you suspect a fungal infection, not a mushroom growth. |
Explore related products
What You'll Learn
- Causes of Fungal Infections - Damp, warm environments encourage fungal growth on skin
- Symptoms of Foot Fungi - Itching, redness, peeling skin, and blisters indicate infection
- Prevention Tips - Keep feet dry, wear breathable shoes, and avoid walking barefoot in public areas
- Treatment Options - Antifungal creams, powders, and oral medications effectively treat foot fungi
- When to See a Doctor - Persistent or severe infections require professional medical evaluation and treatment?

Causes of Fungal Infections - Damp, warm environments encourage fungal growth on skin
Fungal infections thrive in environments that mimic their natural habitats—damp, warm, and often dark spaces. Your feet, encased in shoes for hours, become prime real estate for fungi like *Trichophyton*, the culprit behind athlete’s foot. Sweat accumulates, moisture lingers, and the warmth of your skin creates an ideal breeding ground. This isn’t just about discomfort; untreated infections can spread to nails, hands, or even other people. Understanding this environment is the first step in prevention.
Consider the mechanics: Fungi are opportunistic organisms that require specific conditions to colonize. When feet remain damp—from sweaty socks, wet shoes, or humid climates—the skin’s protective barrier weakens. Warmth accelerates fungal metabolism, allowing spores to germinate and multiply rapidly. For instance, wearing tight, non-breathable footwear traps heat and moisture, doubling the risk of infection. Even public spaces like locker rooms or shared showers can introduce fungal spores to vulnerable feet.
Prevention hinges on disrupting this environment. Start with footwear choices: opt for breathable materials like leather or mesh, and alternate shoes daily to allow them to dry completely. After showers or workouts, thoroughly dry feet—especially between toes—using a clean towel or hairdryer on low heat. For those prone to sweating, antiperspirant foot sprays or powders containing aluminum chloride (6%–25% strength) can reduce moisture. Change socks daily, choosing moisture-wicking fabrics like merino wool or synthetic blends.
If infection strikes, early intervention is key. Over-the-counter antifungal creams (e.g., clotrimazole or terbinafine) applied twice daily for 4–6 weeks are typically effective. For stubborn cases, oral medications like terbinafine (250 mg/day for adults) may be prescribed, though these require monitoring for liver function. Pair treatment with environmental adjustments: disinfect shoes with antifungal sprays, avoid walking barefoot in communal areas, and launder socks and towels in hot water (60°C/140°F) to kill spores.
The takeaway is clear: fungal infections aren’t inevitable. By controlling moisture and warmth, you deprive fungi of their lifeline. Small, consistent habits—like drying feet thoroughly and choosing the right footwear—can prevent infections more effectively than reactive treatments. Think of it as environmental management for your feet, where you’re the architect of a space fungi can’t colonize.
Chanterelle Mushrooms in Fettuccine Alfredo: A Gourmet Twist?
You may want to see also

Symptoms of Foot Fungi - Itching, redness, peeling skin, and blisters indicate infection
Foot fungi, often referred to as athlete’s foot (tinea pedis), thrives in warm, moist environments like sweaty shoes or damp locker rooms. The first sign of infection is usually itching, particularly between the toes, where fungi find ideal conditions to flourish. This persistent discomfort often escalates as the fungus spreads, making early detection crucial. Ignoring this symptom can lead to more severe issues, as the fungus disrupts the skin’s protective barrier, paving the way for secondary bacterial infections.
Redness is another telltale symptom, often accompanied by a burning sensation. This inflammation occurs as the body’s immune system responds to the fungal invasion. In mild cases, the redness may be localized, but untreated infections can cause it to spread across the foot. For individuals with diabetes or compromised immune systems, this symptom warrants immediate attention, as they are at higher risk for complications like cellulitis.
Peeling skin is a direct result of the fungus breaking down the skin’s outer layer, leading to flakiness or scaling. This symptom is most noticeable on the soles and sides of the feet, where friction from walking exacerbates the shedding. Over-the-counter antifungal creams containing clotrimazole or terbinafine (1% strength) can be applied twice daily for 4–6 weeks to combat this. However, if peeling persists or worsens, a healthcare provider may prescribe oral medications like terbinafine (250 mg daily) for more aggressive treatment.
Blisters are a more advanced symptom, indicating a severe fungal infection or a secondary bacterial issue. These fluid-filled pockets can rupture, causing pain and increasing the risk of spreading the infection. To manage blisters, keep the area clean and dry, apply a topical antifungal with an antiseptic like povidone-iodine, and avoid popping them. For recurrent or painful blisters, consult a dermatologist, as they may recommend a combination of oral antifungals and topical steroids to reduce inflammation.
Preventive measures are key to avoiding foot fungi. Wear moisture-wicking socks, rotate shoes to allow them to dry completely, and use antifungal powders in footwear. After public showers or pool areas, thoroughly dry feet, especially between toes, and consider wearing flip-flops to avoid direct contact with contaminated surfaces. By recognizing these symptoms early and taking proactive steps, you can halt the infection’s progression and maintain foot health.
Freezing Cremini Mushrooms: A Complete Guide to Preserve Freshness
You may want to see also

Prevention Tips - Keep feet dry, wear breathable shoes, and avoid walking barefoot in public areas
Mushrooms thrive in damp, dark environments, and while they typically grow in soil or on decaying matter, certain fungal infections can mimic their appearance on human skin, particularly on feet. Athlete’s foot, caused by the fungus *Tinea pedis*, often presents as red, itchy patches or blisters, resembling the early stages of a mushroom colony. Preventing such fungal growth starts with controlling moisture—the lifeblood of fungi.
Step 1: Keep Feet Dry
Moisture is the enemy. Fungi flourish in wet conditions, so drying feet thoroughly after showers, swimming, or sweating is critical. Pay special attention to the spaces between toes, where moisture lingers. For those prone to sweating, use antifungal foot powder daily, focusing on areas like the soles and between toes. Change socks mid-day if necessary, and opt for moisture-wicking materials like merino wool or synthetic blends designed for athletes.
Step 2: Wear Breathable Shoes
Non-breathable footwear traps sweat, creating a greenhouse effect for fungi. Choose shoes made from natural materials like leather or canvas, which allow air circulation. Avoid synthetic materials like rubber or plastic, especially for prolonged wear. Rotate shoes daily to let them dry out completely between uses. For those in humid climates or with active lifestyles, consider investing in shoes with antimicrobial linings or mesh panels for enhanced ventilation.
Step 3: Avoid Walking Barefoot in Public Areas
Public spaces like pools, gyms, and locker rooms are breeding grounds for fungi. Walking barefoot in these areas increases the risk of contracting infections like athlete’s foot or nail fungus. Always wear flip-flops or water shoes in communal showers or pool decks. For added protection, apply a thin layer of antifungal cream or powder to feet before entering such environments, particularly if you have cuts or cracks in the skin where fungi can easily enter.
Cautions and Practical Tips
While prevention is key, over-drying feet can lead to cracks, which fungi can exploit. Balance dryness with hydration by using a non-greasy foot lotion at night, avoiding the spaces between toes. For those with diabetes or compromised immune systems, consult a healthcare provider for personalized prevention strategies, as fungal infections can escalate quickly. Finally, inspect feet regularly for early signs of infection—catching it early can prevent the need for aggressive treatments like oral antifungals.
By integrating these habits into daily routines, you create an environment inhospitable to fungal growth, ensuring your feet remain healthy and mushroom-free.
Portobello vs. King Oyster: Can You Substitute One for the Other?
You may want to see also
Explore related products

Treatment Options - Antifungal creams, powders, and oral medications effectively treat foot fungi
Mushrooms don’t grow on feet, but fungi certainly can, and they’re far less charming than their forest counterparts. Athlete’s foot, toenail fungus, and other fungal infections thrive in warm, damp environments like shoes and socks. Fortunately, antifungal treatments are both effective and accessible, ranging from topical creams to oral medications. The key is early intervention—left untreated, these infections can spread and become more difficult to eradicate.
Topical Treatments: Your First Line of Defense
Antifungal creams, lotions, and powders are typically the first step in treating foot fungi. Active ingredients like clotrimazole, miconazole, and terbinafine work by disrupting the fungal cell membrane, halting growth and reproduction. Apply these products twice daily to clean, dry skin, ensuring coverage of the entire affected area and surrounding skin. Powders, such as tolnaftate, are particularly useful for preventing recurrence by keeping feet dry and inhospitable to fungi. For best results, continue treatment for at least two weeks after symptoms disappear to ensure the infection is fully eradicated.
Oral Medications: When Topicals Aren’t Enough
For severe or persistent infections, oral antifungal medications like terbinafine or itraconazole may be prescribed. These systemic treatments target the fungus from within, making them effective for stubborn cases like toenail fungus. However, they come with considerations: oral antifungals can interact with other medications and may require liver function monitoring. Dosage varies—terbinafine is often taken daily for 6–12 weeks, while itraconazole may be prescribed in pulses (e.g., one week per month for several months). Always follow your healthcare provider’s instructions and complete the full course, even if symptoms improve quickly.
Practical Tips for Maximizing Treatment Efficacy
Pairing antifungal treatments with good foot hygiene amplifies their effectiveness. Keep feet clean and dry, changing socks daily and alternating shoes to allow them to air out. Trim toenails straight across to prevent ingrown nails, which can harbor fungus. For added protection, sprinkle antifungal powder in shoes and avoid walking barefoot in communal areas like locker rooms or pools. If you’re prone to fungal infections, consider using a foot file to remove dead skin, as fungi thrive on keratin-rich environments.
When to Seek Professional Help
While over-the-counter treatments work for most cases, persistent or worsening infections warrant a visit to a dermatologist or podiatrist. Signs of complications include severe pain, pus, or spreading redness, which may indicate a secondary bacterial infection. Professionals can also provide advanced treatments like laser therapy or prescribe stronger medications tailored to your specific condition. Remember, foot fungi may not be as picturesque as mushrooms, but with the right approach, they’re far easier to eliminate.
Mushrooms for Bearded Dragons: Safe or Harmful? Expert Advice
You may want to see also

When to See a Doctor - Persistent or severe infections require professional medical evaluation and treatment
While mushrooms growing on feet might sound like a bizarre concept, it’s a real concern tied to fungal infections. Persistent or severe cases, often mistaken for harmless rashes, can signal deeper issues like compromised immunity or untreated tinea pedis (athlete’s foot). If over-the-counter antifungals (e.g., clotrimazole 1% cream applied twice daily for 4–6 weeks) fail to resolve symptoms, or if redness, swelling, and pus accompany the infection, professional intervention is critical. Fungal organisms thrive in damp, warm environments, and feet, often confined in shoes, provide ideal conditions. Ignoring these signs risks systemic spread, particularly in diabetics or the immunocompromised.
Analyzing the progression of foot fungus reveals why timely medical attention matters. Mild cases may present as itching or scaling, but severe infections can lead to cracked skin, blisters, or even fungal nails. If symptoms persist beyond two weeks despite consistent treatment, consult a dermatologist. They may prescribe oral antifungals like terbinafine (250 mg daily for 6–12 weeks) or perform a potassium hydroxide (KOH) test to confirm the fungal type. Delaying care increases the risk of secondary bacterial infections, which can escalate into cellulitis, requiring antibiotics like cephalexin (500 mg every 6 hours for 7–14 days).
Persuasively, consider the long-term consequences of neglecting persistent foot fungus. Chronic infections can lead to permanent nail damage, recurrent outbreaks, or even sepsis in extreme cases. For those over 60 or with conditions like diabetes, HIV, or psoriasis, the stakes are higher. Regular foot inspections, keeping feet dry, and avoiding shared footwear are preventive measures, but they’re no substitute for professional care when infections worsen. A podiatrist or dermatologist can tailor treatment, ensuring the fungus is eradicated before it becomes a recurring nightmare.
Comparatively, while home remedies like tea tree oil or vinegar soaks may offer temporary relief, they lack the potency of prescription treatments. For instance, a study in the *Journal of Clinical and Aesthetic Dermatology* found that 5% tea tree oil was only 34% effective against tinea pedis compared to 80% efficacy with terbinafine. Relying solely on natural remedies for severe cases is akin to using a bandage on a bullet wound. When symptoms like fever, intense pain, or rapid spreading occur, head to the emergency room—these could indicate a systemic infection requiring intravenous antifungals like amphotericin B.
Descriptively, imagine a scenario where a persistent foot fungus transforms from a minor nuisance to a debilitating condition. The skin cracks, oozes, and bleeds, making walking agonizing. Shoes become instruments of torture, and the infection’s odor is socially isolating. This isn’t mere discomfort—it’s a quality-of-life crisis. A doctor’s visit could have prevented this with early diagnosis and targeted therapy. Practical tips include changing socks daily, using antifungal powders in shoes, and avoiding walking barefoot in communal areas. But when home efforts fail, professional care isn’t optional—it’s essential.
Freezing Dehydrated Mushrooms: A Guide to Preservation and Storage
You may want to see also
Frequently asked questions
While rare, certain fungi can infect the skin on feet, leading to conditions like athlete’s foot, but true mushrooms do not grow on human feet.
Fungal infections like athlete’s foot or toenail fungus are caused by dermatophytes, which thrive in warm, moist environments, but they do not form mushroom-like structures.
No, mushrooms do not target human feet. Fungal infections on feet are caused by common dermatophytes, not mushroom species.
Walking barefoot in damp areas can increase the risk of fungal infections, but mushrooms will not grow on feet; only fungal spores may cause skin issues.
Keep feet clean and dry, wear breathable footwear, avoid walking barefoot in public areas, and use antifungal powders or sprays to prevent infections.