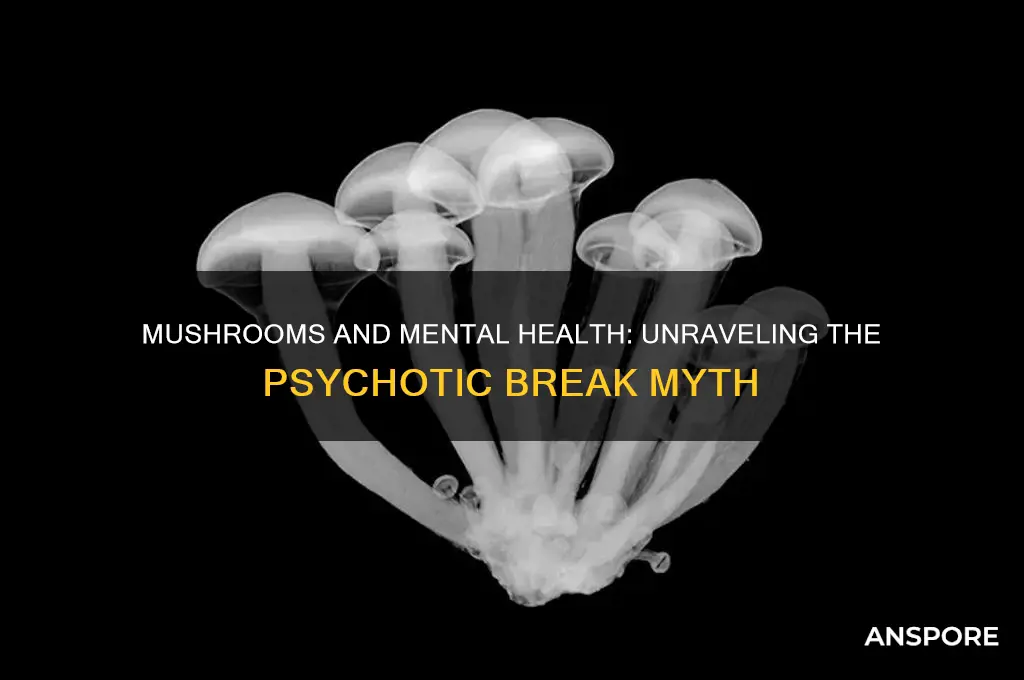
The question of whether mushrooms, particularly those containing psychoactive compounds like psilocybin, can cause a psychotic break is a topic of significant interest and debate in both scientific and public spheres. Psilocybin mushrooms, often referred to as magic mushrooms, have been used for centuries in various cultures for their hallucinogenic effects. While many users report profound, positive experiences, including enhanced creativity and spiritual insights, there is growing concern about the potential risks, especially for individuals predisposed to mental health conditions. Research suggests that psilocybin can induce temporary psychotic-like symptoms, such as hallucinations and paranoia, even in healthy individuals. However, the likelihood of a full-blown psychotic break is generally considered low for most people, though it may be higher in those with a family history of schizophrenia or other psychotic disorders. Understanding the interplay between these substances and mental health is crucial as their use becomes more widespread in both recreational and therapeutic contexts.
| Characteristics | Values |
|---|---|
| Substance | Psilocybin (active compound in psychedelic mushrooms) |
| Psychotic Break Risk | Can trigger or exacerbate psychotic symptoms in susceptible individuals |
| Susceptible Populations | Individuals with personal or family history of mental illness (e.g., schizophrenia, bipolar disorder) |
| Mechanism | Alters serotonin levels and brain activity, potentially disrupting perception and cognition |
| Symptoms | Hallucinations, delusions, paranoia, disorganized thinking, and detachment from reality |
| Duration | Acute effects typically last 4-6 hours, but psychological impact may persist |
| Long-Term Effects | May increase risk of persistent psychosis or hallucinogen persisting perception disorder (HPPD) in vulnerable individuals |
| Prevalence | Rare, but risk increases with high doses, frequent use, or pre-existing mental health conditions |
| Medical Context | Used in controlled therapeutic settings under supervision; not recommended for recreational use in at-risk individuals |
| Prevention | Avoid use if personal or family history of mental illness; use in safe, controlled environments |
| Research Status | Ongoing studies to understand risks and therapeutic potential; limited conclusive data on causation |
Explore related products
What You'll Learn
- Psilocybin's Role in Psychosis: Examines how psilocybin mushrooms may trigger psychotic episodes in susceptible individuals
- Pre-existing Conditions: Explores if mental health disorders increase risk of mushroom-induced psychotic breaks
- Dosage and Effects: Investigates whether high doses of mushrooms correlate with psychotic symptoms
- Long-term Impact: Studies potential lasting psychotic effects after mushroom use in vulnerable users
- Misidentification Risks: Discusses dangers of consuming toxic mushrooms mistaken for psychedelic varieties

Psilocybin's Role in Psychosis: Examines how psilocybin mushrooms may trigger psychotic episodes in susceptible individuals
Psilocybin, the psychoactive compound found in certain mushrooms, has been both celebrated and scrutinized for its profound effects on the mind. While many users report transformative experiences, including enhanced creativity and emotional clarity, the substance is not without risks. For individuals with a predisposition to mental health disorders, particularly schizophrenia or bipolar disorder, psilocybin can act as a catalyst for psychotic episodes. This vulnerability is often linked to genetic factors, pre-existing conditions, or a family history of psychosis. Understanding this risk is crucial, as even a single dose of psilocybin—typically ranging from 10 to 25 milligrams—can trigger symptoms like hallucinations, paranoia, and disorganized thinking in susceptible individuals.
The mechanism behind psilocybin’s potential to induce psychosis lies in its interaction with the brain’s serotonin receptors, particularly the 5-HT2A receptor. This interaction disrupts normal neural pathways, leading to altered perceptions of reality. For most users, these effects are temporary and resolve within 6 to 8 hours. However, in vulnerable populations, the brain may struggle to reintegrate these altered states, resulting in prolonged or permanent psychotic symptoms. Research suggests that individuals under 25, whose brains are still developing, are at higher risk due to increased neural plasticity and susceptibility to external influences.
To mitigate the risk of psilocybin-induced psychosis, several precautions should be taken. First, individuals with a personal or family history of mental illness should avoid psilocybin altogether. Second, those considering its use should start with the lowest effective dose (10 milligrams) and consume it in a controlled, supportive environment, often referred to as "set and setting." Third, having a sober, trusted companion present can provide grounding and assistance if symptoms of psychosis emerge. Finally, integrating the experience through therapy or journaling can help process the effects and reduce the likelihood of long-term psychological harm.
Comparatively, while substances like LSD and DMT also carry risks of psychosis, psilocybin’s effects are often considered more predictable and manageable due to its shorter duration and lower potency. However, this does not negate its potential dangers. Unlike recreational drugs, psilocybin is increasingly being studied for therapeutic use in controlled settings, such as treating depression or PTSD. These clinical trials emphasize rigorous screening to exclude individuals at risk of psychosis, highlighting the importance of medical oversight when using this substance.
In conclusion, while psilocybin holds promise as a therapeutic tool, its ability to trigger psychotic episodes in susceptible individuals cannot be overlooked. Awareness of personal risk factors, adherence to safe dosing practices, and a cautious approach are essential for minimizing harm. As research continues to explore psilocybin’s potential, balancing its benefits against its risks remains a critical consideration for both users and healthcare providers.
Can Puppies Safely Eat Wild Mushrooms? Risks and Precautions
You may want to see also

Pre-existing Conditions: Explores if mental health disorders increase risk of mushroom-induced psychotic breaks
Psychoactive mushrooms, particularly those containing psilocybin, have been both revered and feared for their ability to alter perception and mood. While many users report profound, positive experiences, others face distressing episodes, including psychotic breaks. The question arises: do pre-existing mental health disorders heighten this risk? Research suggests a nuanced answer, emphasizing the interplay between individual vulnerability and substance interaction.
Consider schizophrenia, a condition marked by distorted thinking and perception. Studies indicate that individuals with a family history of schizophrenia or those already diagnosed are more susceptible to mushroom-induced psychosis. Psilocybin’s mechanism—activating serotonin receptors in the brain—can exacerbate underlying imbalances, potentially triggering acute episodes. For instance, a 2019 case study published in *The Journal of Clinical Psychiatry* detailed a 22-year-old with undiagnosed schizophrenia who experienced persistent hallucinations after a single high dose (5 grams) of psilocybin mushrooms. This highlights the importance of screening for familial or personal psychiatric histories before use.
Anxiety and depression present a different scenario. While low to moderate doses (1–2 grams) of psilocybin have shown therapeutic potential in controlled settings, individuals with severe, untreated anxiety or depression may react unpredictably. The substance’s ability to amplify emotions can lead to overwhelming fear or despair, mimicking a psychotic break. A 2021 study in *JAMA Psychiatry* found that 15% of participants with treatment-resistant depression experienced transient paranoia during psilocybin therapy, though these effects resolved within 24 hours. This underscores the need for professional supervision and tailored dosing protocols.
Bipolar disorder introduces another layer of risk. Psilocybin’s mood-altering properties can destabilize individuals in manic or hypomanic states, potentially prolonging or intensifying episodes. A longitudinal study in *Molecular Psychiatry* (2020) noted that bipolar patients who used psychoactive mushrooms were twice as likely to report psychotic symptoms compared to those without the disorder. For this population, even microdosing (0.1–0.5 grams) may disrupt emotional regulation, making abstinence a safer recommendation.
Practical precautions are essential for anyone with a mental health disorder considering mushroom use. First, consult a psychiatrist or psychologist to assess risk factors. Second, avoid self-medication; therapeutic use should occur under expert guidance. Third, start with minimal doses in a controlled environment, and prioritize strains with lower psilocybin content if experimentation is unavoidable. Finally, maintain a support system to monitor for early signs of distress. While mushrooms hold transformative potential, their interaction with pre-existing conditions demands caution and informed decision-making.
Mushroom Compost Manure Mix: Effective Potting Soil Alternative?
You may want to see also

Dosage and Effects: Investigates whether high doses of mushrooms correlate with psychotic symptoms
Psychoactive mushrooms, particularly those containing psilocybin, have been both revered and feared for their profound effects on the mind. While low to moderate doses (0.5–2 grams) often induce euphoria, heightened sensory perception, and introspection, high doses (3 grams or more) can push users into uncharted psychological territory. At these levels, the line between a transformative experience and a psychotic episode blurs. Users report symptoms like paranoia, disconnection from reality, and persistent hallucinations—effects that mirror acute psychosis. This raises a critical question: does dosage alone predict the risk of a psychotic break, or are other factors at play?
Consider the role of set and setting—a user’s mindset and environment—in modulating the effects of high doses. A 2021 study published in *Psychopharmacology* found that individuals with a personal or family history of mental illness were significantly more likely to experience psychotic symptoms after consuming large amounts of psilocybin. For example, a 25-year-old with no psychiatric history might navigate a 4-gram dose with intense but manageable effects, while someone predisposed to schizophrenia could spiral into a full-blown psychotic episode. This suggests that dosage is not the sole determinant; vulnerability matters.
Practical guidance for harm reduction is essential when discussing high doses. If you’re experimenting with mushrooms, start with a threshold dose (0.5–1 gram) to gauge sensitivity. Gradually increase by 0.5-gram increments in controlled settings, ensuring a trusted sober companion is present. Avoid high doses if you’re under 25 (when the brain is still developing) or have a history of mental health issues. Should psychotic symptoms emerge—such as persistent delusions or inability to distinguish reality—seek medical attention immediately. Antipsychotic medications like benzodiazepines can mitigate acute distress, but prevention remains the best strategy.
Comparatively, the relationship between dosage and psychotic symptoms in mushrooms contrasts with substances like LSD, where even microdoses can trigger adverse reactions in susceptible individuals. Psilocybin’s effects are dose-dependent but context-sensitive, making it a double-edged tool for exploration. While high doses can unlock profound insights, they also carry the risk of psychological trauma. For instance, a 30-year-old artist described a 5-gram experience as both enlightening and terrifying, emerging with temporary but distressing symptoms of depersonalization. Such anecdotes underscore the importance of respecting potency and personal limits.
In conclusion, high doses of mushrooms do correlate with an increased risk of psychotic symptoms, but dosage alone is insufficient to predict outcomes. Factors like genetic predisposition, mental health history, and environmental context play pivotal roles. Treat high-dose experiences with caution, prioritizing safety and self-awareness. As research into psychedelics expands, understanding these nuances will be key to harnessing their potential while minimizing harm.
How to Safely Remove Mushrooms from Your Lawn: Tips and Tricks
You may want to see also
Explore related products

Long-term Impact: Studies potential lasting psychotic effects after mushroom use in vulnerable users
Psychotic episodes triggered by psychedelic mushrooms often fade within hours, but emerging research suggests a subset of users may face lingering consequences. Studies focusing on individuals with pre-existing mental health vulnerabilities, such as a family history of schizophrenia or bipolar disorder, have identified a concerning pattern. Even after the acute effects wear off, some users report persistent symptoms like paranoia, disorganized thinking, or auditory hallucinations. These cases, though relatively rare, highlight the need for a nuanced understanding of psilocybin's long-term impact on susceptible populations.
While the majority of mushroom users experience temporary altered states without lasting harm, the potential for prolonged psychosis in vulnerable individuals cannot be ignored.
Consider the case of a 22-year-old with a family history of schizophrenia who, after a single high-dose mushroom experience (estimated at 3.5 grams of dried psilocybin mushrooms), developed persistent delusions requiring antipsychotic medication. This example, though anecdotal, aligns with findings from a 2019 study published in the *Journal of Psychopharmacology*. The study tracked 20 individuals with a predisposition to psychosis who had used psychedelics, including mushrooms. 30% reported experiencing psychotic symptoms lasting beyond the initial trip, with an average duration of 6 months. These findings underscore the importance of screening for mental health risk factors before considering psychedelic use.
"Just because something is natural doesn't mean it's risk-free," warns Dr. Emily Carter, a psychiatrist specializing in substance use disorders. "We need to move beyond the 'magic mushroom' narrative and acknowledge the potential for harm, especially in those with a genetic predisposition to psychosis."
Long-term studies are crucial to fully understanding the relationship between mushroom use and persistent psychosis. Current research suggests that factors like dosage, frequency of use, and individual susceptibility play a significant role. While microdosing (typically 0.1-0.3 grams) is often touted for its potential therapeutic benefits, its long-term effects on vulnerable populations remain largely unexplored. Larger, controlled studies are needed to determine safe dosage ranges and identify individuals at highest risk for adverse outcomes.
Until more definitive data is available, a cautious approach is warranted. Individuals with a personal or family history of psychotic disorders should avoid psychedelic mushrooms altogether. For those without such risk factors, responsible use dictates starting with very low doses in a safe and supportive environment, with a trusted individual present.
Freezing Fresh Mushrooms: A Guide to Preserving and Reusing Later
You may want to see also

Misidentification Risks: Discusses dangers of consuming toxic mushrooms mistaken for psychedelic varieties
The allure of psychedelic mushrooms has led many to forage in the wild, but this practice carries a grave risk: misidentifying toxic species. Amanita ocreata, for instance, closely resembles the sought-after Psilocybe species but contains amatoxins, which can cause liver failure within 24–48 hours. A single misidentified mushroom can be fatal, making accurate identification critical. Unlike psychedelics, whose effects are immediate, toxic mushrooms may delay symptoms, lulling foragers into a false sense of security. This discrepancy highlights the danger of assuming all mushrooms with similar appearances are safe.
To mitigate misidentification risks, follow a systematic approach. First, consult a field guide specific to your region, as mushroom species vary widely by geography. Second, learn the key characteristics of both psychedelic and toxic varieties, such as spore color, gill structure, and bruising reactions. For example, Psilocybe mushrooms often bruise blue when handled, while Amanita species typically have a bulbous base and white spores. Third, cross-reference findings with multiple sources or consult an expert mycologist. Never rely on folklore or single visual cues, as even experienced foragers can make errors.
The consequences of misidentification extend beyond physical harm. Consuming toxic mushrooms can lead to severe psychotic episodes, mimicking the effects of a psychedelic overdose but without the therapeutic potential. Amatoxin poisoning, for instance, can cause delirium, seizures, and confusion, often mistaken for a "bad trip." This confusion delays proper medical treatment, increasing the risk of organ failure. Unlike psychedelics, which are generally non-toxic in moderate doses (e.g., 1–3 grams of Psilocybe cubensis), toxic mushrooms have no safe threshold—even a small bite can be lethal.
Practical precautions are essential for safe foraging. Always carry a knife and basket to collect specimens without damaging them, preserving key identification features. Avoid picking mushrooms near polluted areas, as toxins can accumulate in their tissues. If in doubt, discard the find—the risk is never worth the reward. For those seeking psychedelic experiences, purchasing from reputable sources or growing kits is far safer than wild harvesting. Remember, the goal is not just to avoid toxicity but to ensure a responsible and informed approach to mushroom use.
Shiitake Mushrooms and Blood Pressure: Uncovering the Surprising Connection
You may want to see also
Frequently asked questions
Yes, certain types of mushrooms, particularly those containing psychoactive compounds like psilocybin, can trigger a psychotic break in individuals predisposed to mental health conditions or in high doses.
Individuals with a personal or family history of mental health disorders, such as schizophrenia or bipolar disorder, are at higher risk. First-time users, those consuming large doses, or people in stressful environments are also more vulnerable.
Psychotic symptoms from mushrooms are usually temporary, lasting a few hours to a day. However, in rare cases, they can persist for days or weeks, especially in individuals with underlying mental health issues.
While rare, mushrooms can potentially trigger permanent psychosis in individuals with a genetic predisposition or severe underlying mental health conditions. Most cases resolve without long-term effects.