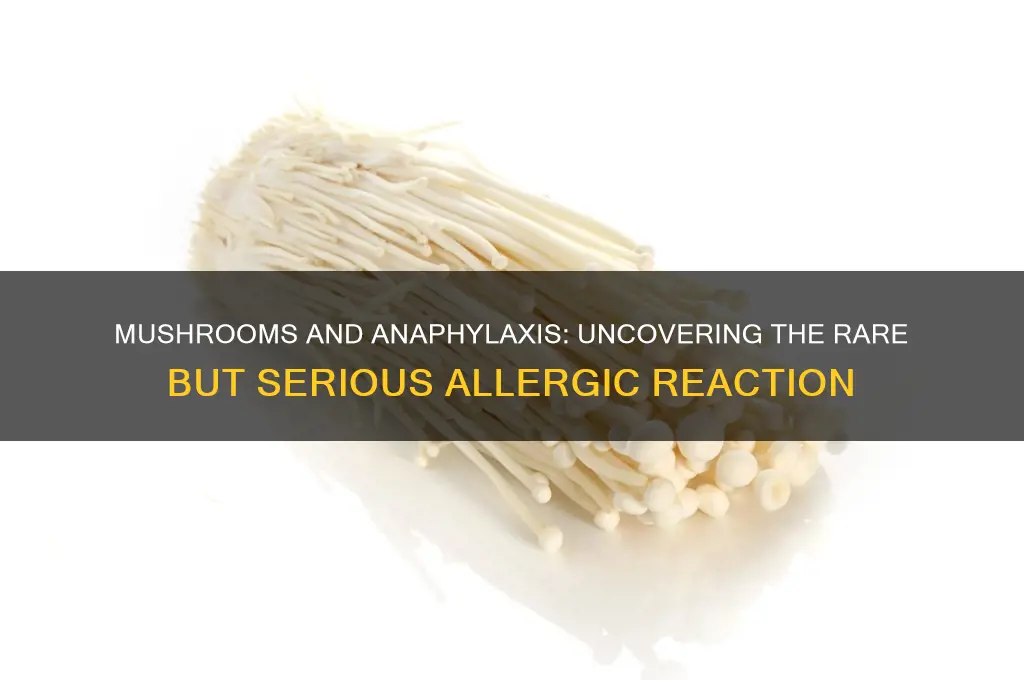
Mushrooms, while generally considered safe for consumption, have been rarely associated with severe allergic reactions, including anaphylaxis. Although such cases are uncommon, certain individuals may exhibit hypersensitivity to specific mushroom proteins or compounds, leading to potentially life-threatening symptoms. Anaphylaxis from mushrooms can manifest as rapid onset of symptoms such as difficulty breathing, swelling, hives, and a drop in blood pressure. These reactions are typically triggered by either ingestion or, in some cases, exposure to mushroom spores. Given the rarity of such incidents, it is crucial for individuals with known allergies or sensitivities to exercise caution and seek medical advice if they experience any adverse reactions after consuming or handling mushrooms.
| Characteristics | Values |
|---|---|
| Can mushrooms cause anaphylaxis? | Yes, although rare, mushrooms can cause anaphylaxis in susceptible individuals. |
| Common mushroom species associated with anaphylaxis | Shiitake, oyster, and other edible mushrooms; cases also reported with wild mushrooms. |
| Mechanism of reaction | IgE-mediated immune response to mushroom proteins or allergens. |
| Symptoms of mushroom-induced anaphylaxis | Rapid onset of hives, itching, swelling, difficulty breathing, dizziness, and potentially life-threatening shock. |
| Prevalence | Rare; more common in individuals with known mushroom allergies or sensitivities. |
| Risk factors | History of mushroom allergy, atopic conditions (e.g., asthma, eczema), or cross-reactivity with other allergens. |
| Diagnosis | Clinical history, skin prick tests, specific IgE blood tests, or oral food challenges under medical supervision. |
| Treatment | Immediate administration of epinephrine (adrenaline), antihistamines, and corticosteroids; emergency medical attention required. |
| Prevention | Avoidance of mushrooms for known allergic individuals; careful identification of wild mushrooms to prevent accidental ingestion. |
| Cross-reactivity | Possible cross-reactivity with other fungi or mold allergens in some cases. |
| Research status | Limited studies; most evidence is from case reports and small clinical studies. |
Explore related products
What You'll Learn
- Common Mushroom Allergens: Proteins in mushrooms like Agaricus bisporus can trigger allergic reactions in sensitive individuals
- Symptoms of Anaphylaxis: Rapid onset of hives, swelling, difficulty breathing, and low blood pressure after mushroom exposure
- Cross-Reactivity Risks: Allergies to molds or other fungi may increase the likelihood of mushroom-induced anaphylaxis
- Diagnosis Methods: Skin prick tests and IgE blood tests help identify mushroom allergies linked to anaphylaxis
- Prevention Strategies: Avoiding mushrooms, carrying epinephrine, and reading food labels to prevent severe reactions

Common Mushroom Allergens: Proteins in mushrooms like Agaricus bisporus can trigger allergic reactions in sensitive individuals
Mushroom allergies, though less common than reactions to nuts or shellfish, can be severe, with proteins in species like *Agaricus bisporus* (the common button mushroom) acting as potent allergens. These proteins, such as hydrophobins and lectins, are recognized by the immune system of sensitive individuals, triggering reactions that range from mild itching to life-threatening anaphylaxis. Unlike many food allergens, mushroom proteins are heat-stable, meaning cooking does not denature them, leaving allergic individuals vulnerable even to well-prepared dishes.
Identifying a mushroom allergy requires vigilance, as symptoms can manifest within minutes to hours of ingestion. Common signs include hives, swelling, abdominal pain, and respiratory distress. Anaphylaxis, though rare, is characterized by rapid onset of symptoms like throat swelling, difficulty breathing, and a sudden drop in blood pressure. Immediate administration of epinephrine via an auto-injector (e.g., EpiPen) is critical in such cases, followed by urgent medical attention. Individuals with known allergies should carry two doses of epinephrine, as delayed or repeated reactions can occur.
For those suspecting a mushroom allergy, an allergist can perform skin prick tests or blood tests (e.g., IgE antibody tests) to confirm sensitivity. Cross-reactivity with other fungi, such as molds or yeast, is possible, complicating diagnosis. Elimination diets, under medical supervision, can help identify triggers, but strict avoidance of mushrooms and products containing mushroom derivatives (e.g., soups, sauces, or supplements) is the primary management strategy. Reading food labels carefully is essential, as mushrooms may be listed under terms like "natural flavors" or "umami enhancers."
Prevention is key for at-risk individuals, particularly in social or dining-out scenarios. Communicating allergies clearly to chefs or hosts reduces contamination risks, and carrying a chef card in multiple languages can be invaluable when traveling. For children, educating caregivers and school staff about allergy management is crucial, as accidental exposure is more likely in group settings. While mushroom allergies are rare, their potential severity underscores the need for preparedness and awareness in sensitive populations.
Slimy Mushrooms: Safe to Rinse or Toss? Quick Tips
You may want to see also

Symptoms of Anaphylaxis: Rapid onset of hives, swelling, difficulty breathing, and low blood pressure after mushroom exposure
Mushroom exposure, though rare, can trigger anaphylaxis, a severe and potentially life-threatening allergic reaction. The symptoms of anaphylaxis following mushroom ingestion or contact manifest rapidly, often within minutes to an hour. The first noticeable signs typically include hives, which appear as raised, itchy welts on the skin. These hives are the body’s immediate response to an allergen, signaling the release of histamines and other inflammatory substances. Simultaneously, swelling may occur, particularly around the face, lips, throat, or extremities, due to fluid accumulation in the tissues. This swelling can be alarming, especially when it affects the throat, as it may lead to difficulty breathing, a hallmark symptom of anaphylaxis. As the reaction progresses, low blood pressure (hypotension) can develop, causing dizziness, fainting, or a rapid, weak pulse. This combination of symptoms requires immediate medical attention, as anaphylaxis can escalate quickly and become fatal if untreated.
For individuals who suspect mushroom-induced anaphylaxis, recognizing these symptoms early is critical. Hives and swelling are often the first indicators, but they can be mistaken for milder allergic reactions. The key differentiator is the rapid onset and severity of symptoms. Difficulty breathing, for instance, may present as wheezing, shortness of breath, or a tight feeling in the chest. Low blood pressure can manifest as confusion, pale skin, or loss of consciousness. If any of these symptoms occur after mushroom exposure—whether through ingestion, inhalation, or skin contact—emergency medical intervention is essential. Epinephrine (adrenaline) administered via an auto-injector (e.g., EpiPen) is the first-line treatment and should be used immediately while awaiting professional help.
Comparatively, mushroom-induced anaphylaxis is less common than reactions to foods like peanuts or shellfish, but its severity is no less critical. Unlike mild allergic reactions, which may resolve with antihistamines, anaphylaxis demands urgent action. For those with known mushroom allergies, avoidance is the best prevention. However, accidental exposure can occur, particularly in culinary settings or outdoor activities. Practical tips include thoroughly identifying mushrooms before consumption, avoiding wild mushrooms unless verified by an expert, and informing others of your allergy. Wearing gloves when handling mushrooms can reduce the risk of skin contact, and ensuring proper ventilation can minimize inhalation risks.
Instructively, if you or someone you know experiences symptoms of anaphylaxis after mushroom exposure, follow these steps: 1) Administer epinephrine immediately if available. 2) Call emergency services or proceed to the nearest hospital. 3) Lay the person flat (or on their side if vomiting) to maintain blood flow. 4) Remove any tight clothing or jewelry that could restrict breathing. 5) Monitor breathing and vital signs until help arrives. It’s crucial not to delay treatment, even if symptoms seem to improve temporarily, as biphasic reactions (a recurrence of symptoms hours later) can occur.
Descriptively, the body’s response to mushroom allergens in anaphylaxis is a dramatic cascade of events. Histamine release causes blood vessels to dilate, leading to hives and swelling, while also triggering bronchial constriction, which impairs breathing. Simultaneously, the immune system’s overreaction causes blood vessels to leak fluid, resulting in low blood pressure and reduced organ perfusion. This systemic reaction underscores why anaphylaxis is a medical emergency. For those at risk, carrying an epinephrine auto-injector and wearing a medical alert bracelet are essential precautions. Awareness and preparedness can save lives, turning a potentially fatal encounter into a manageable incident.
Puffball Mushrooms and Psychoactivity: Separating Fact from Fiction
You may want to see also

Cross-Reactivity Risks: Allergies to molds or other fungi may increase the likelihood of mushroom-induced anaphylaxis
Mushroom allergies, though rare, can trigger severe reactions, including anaphylaxis. For individuals with pre-existing allergies to molds or other fungi, the risk escalates due to cross-reactivity. This phenomenon occurs when the immune system mistakes proteins in mushrooms for those in molds, launching an aggressive response. Understanding this link is crucial for those with fungal allergies, as it highlights the need for caution when consuming mushrooms or even handling them in environments where fungal spores are prevalent.
Cross-reactivity stems from shared allergenic proteins, such as beta-glucans and chitin, found in both fungi and mushrooms. Studies show that individuals allergic to *Aspergillus* or *Penicillium* molds, for instance, may experience symptoms like hives, swelling, or difficulty breathing after mushroom exposure. While not all fungal allergy sufferers will react to mushrooms, the potential for anaphylaxis is higher in this group. Immediate medical attention is essential if symptoms like throat tightness, rapid heartbeat, or dizziness occur, as epinephrine may be required to halt the reaction.
Practical precautions can mitigate risk. Individuals with known fungal allergies should avoid wild mushrooms, as they are more likely to harbor mold contaminants. Cultivated varieties, grown in controlled environments, are safer but not risk-free. Cooking mushrooms thoroughly can denature some allergens, but this does not eliminate all risks. Reading food labels carefully is also vital, as mushrooms may be hidden in sauces, soups, or supplements. For those with severe fungal allergies, carrying an epinephrine auto-injector is a proactive step, especially when dining out or in unfamiliar settings.
Children and adults with asthma or atopic dermatitis are particularly vulnerable, as fungal allergies often coexist with these conditions. Parents should monitor for signs of mushroom sensitivity, such as itching or gastrointestinal distress, after exposure. Allergy testing, including skin prick tests or specific IgE blood tests, can confirm sensitivities and guide dietary choices. Consulting an allergist is recommended for personalized advice, especially before introducing mushrooms into the diet of someone with a fungal allergy history.
In summary, cross-reactivity between fungal and mushroom allergies poses a tangible anaphylaxis risk for susceptible individuals. Awareness, avoidance strategies, and preparedness are key to managing this risk. By recognizing the connection between mold and mushroom allergies, those affected can take informed steps to protect their health, ensuring that a meal or environmental exposure doesn’t turn into a medical emergency.
Can You Eat Mushroom Stems? A Guide to Edible Parts
You may want to see also
Explore related products

Diagnosis Methods: Skin prick tests and IgE blood tests help identify mushroom allergies linked to anaphylaxis
Mushroom allergies, though rare, can trigger severe reactions, including anaphylaxis. Identifying these allergies early is crucial for prevention and management. Two primary diagnostic tools—skin prick tests and IgE blood tests—offer reliable methods to detect mushroom-specific allergies linked to anaphylaxis. These tests are particularly valuable for individuals with a history of adverse reactions to mushrooms, whether consumed or inhaled as spores.
Skin prick tests are a straightforward, minimally invasive method to assess mushroom allergies. During the test, a small amount of mushroom extract is applied to the skin, typically on the forearm or back, and the skin is gently pricked to allow the allergen to penetrate. A positive reaction, indicated by swelling, redness, or itching at the test site, suggests the presence of mushroom-specific IgE antibodies. This test is often performed in a controlled clinical setting and provides rapid results, usually within 15–20 minutes. It is suitable for adults and children alike, though caution is advised for those with severe eczema or other skin conditions that might interfere with results.
IgE blood tests, also known as specific IgE tests or RAST (Radioallergosorbent Test), measure the level of IgE antibodies in the blood that are specific to mushroom allergens. Unlike skin prick tests, this method does not require direct exposure to the allergen, making it a safer option for individuals at high risk of severe reactions. A blood sample is drawn and analyzed in a laboratory, with results typically available within a few days. Normal IgE levels vary by age, but elevated levels of mushroom-specific IgE strongly indicate an allergy. For example, a class 3 or higher result (on a scale of 1–6) often correlates with a high likelihood of clinical allergy.
While both tests are effective, their choice depends on patient factors and clinical context. Skin prick tests are preferred for their speed and cost-effectiveness, but IgE blood tests are ideal for those with skin conditions or a history of severe reactions. Combining both methods can enhance diagnostic accuracy, especially in complex cases. For instance, a positive skin prick test followed by confirmation via IgE blood test provides robust evidence of a mushroom allergy.
Practical tips for patients include avoiding antihistamines for 3–7 days before skin prick testing, as they can suppress reactions. For IgE blood tests, no specific preparation is required, though fasting is typically unnecessary. Regardless of the method, consulting an allergist is essential for interpreting results and developing a personalized management plan. Early diagnosis not only prevents life-threatening anaphylaxis but also empowers individuals to make informed dietary and environmental choices.
Can King Stropharia Mushrooms Neutralize Sodium Chloride? Exploring the Science
You may want to see also

Prevention Strategies: Avoiding mushrooms, carrying epinephrine, and reading food labels to prevent severe reactions
Mushroom allergies, though rare, can trigger severe reactions, including anaphylaxis. For those affected, prevention is paramount. The cornerstone of this strategy is complete avoidance of mushrooms, both in their whole form and as hidden ingredients in processed foods. This requires vigilance, as mushrooms can lurk in unexpected places—soups, sauces, stuffings, and even dietary supplements. Cross-contamination is another risk, especially in restaurants or shared kitchens, where utensils or surfaces may have come into contact with mushrooms.
Carrying epinephrine auto-injectors is non-negotiable for individuals with a known mushroom allergy. Anaphylaxis can escalate rapidly, and epinephrine is the only effective treatment to reverse symptoms like throat swelling, severe hives, or difficulty breathing. Adults and children over 30 kg typically use a 0.3 mg dose, while those under 30 kg require a 0.15 mg dose. Ensure the auto-injector is accessible at all times, not buried in a bag or left in a car. Regularly check the expiration date and replace it as needed, as expired epinephrine may be less effective.
Reading food labels is a critical skill for mushroom-allergic individuals. Look for explicit mentions of mushrooms, but also be wary of vague terms like "natural flavors," "vegetable broth," or "umami seasoning," which may contain mushroom derivatives. In countries like the U.S., mushrooms are not among the top allergens requiring mandatory labeling, so manufacturers may not highlight their presence. When dining out, ask detailed questions about ingredients and preparation methods, and consider carrying a chef card explaining your allergy in multiple languages if traveling.
Combining these strategies creates a robust defense against mushroom-induced anaphylaxis. Avoidance minimizes exposure, epinephrine provides a lifeline in emergencies, and label literacy empowers informed choices. For parents of allergic children, educate caregivers, teachers, and peers about the risks and ensure they know how to use an auto-injector. While living with a mushroom allergy demands constant awareness, these measures can help individuals lead safe, unrestricted lives.
Exploring Potassium Hydroxide's Reaction with Dried Mushrooms: A Chemical Analysis
You may want to see also
Frequently asked questions
Yes, mushrooms can cause anaphylaxis in rare cases, particularly in individuals who are allergic to specific mushroom proteins or components.
Symptoms include difficulty breathing, swelling of the face or throat, hives, rapid heartbeat, dizziness, and in severe cases, loss of consciousness.
Individuals with a known allergy to mushrooms or those with a history of severe allergic reactions to fungi are at higher risk. Always consult a doctor if you suspect an allergy.