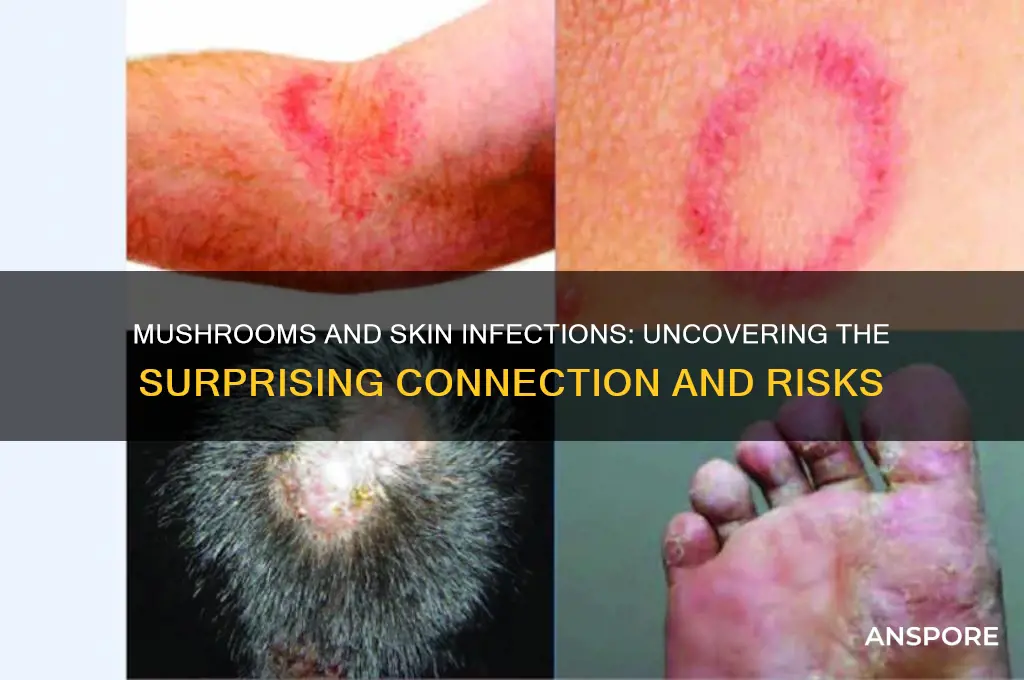
Mushrooms, while often celebrated for their culinary and medicinal benefits, can occasionally be associated with skin infections, though such cases are relatively rare. Certain species of fungi, including some mushrooms, can cause dermatological issues if they come into direct contact with the skin or if an individual is allergic or sensitive to fungal spores. Conditions like tinea (ringworm) or fungal dermatitis may arise from prolonged exposure to mold or mushroom spores, particularly in damp environments. Additionally, handling wild mushrooms without proper protection can lead to irritation or infection, especially if the skin is compromised. Understanding the potential risks and practicing caution when handling mushrooms or being in fungal-rich environments can help prevent such skin issues.
| Characteristics | Values |
|---|---|
| Can mushrooms cause skin infections? | Yes, certain mushrooms can cause skin infections, though it is relatively rare. |
| Types of mushrooms involved | Primarily dermatophytes (e.g., Trichophyton species) and some wild mushrooms like Amanita or Clitocybe species. |
| Mechanism of infection | Direct contact with fungal spores or mycelium can lead to dermatophytosis (ringworm) or allergic reactions. |
| Common symptoms | Itching, redness, rashes, blisters, or dermatitis at the site of contact. |
| Risk factors | Handling wild mushrooms, occupational exposure (e.g., farmers, gardeners), or weakened immune systems. |
| Prevention | Wearing gloves when handling mushrooms, proper hygiene, and avoiding contact with unknown fungi. |
| Treatment | Topical antifungal creams, oral antifungals, or corticosteroids for severe cases. |
| Prevalence | Rare compared to other fungal infections like athlete's foot or jock itch. |
| Misconception | Not all mushrooms cause skin infections; only specific species are implicated. |
| Research status | Limited studies, but cases are documented in medical literature. |
Explore related products
What You'll Learn

Types of Mushroom-Related Skin Infections
Mushroom-related skin infections, though rare, can occur through direct contact with certain fungi or their spores. One well-documented type is dermatophytosis caused by keratinophilic fungi, which thrive on the keratin in skin, hair, and nails. Species like *Trichophyton verrucosum* and *Microsporum gypseum* are commonly associated with these infections, often contracted through handling contaminated soil or infected animals. Symptoms include ringworm-like lesions, itching, and scaling, typically appearing 4–10 days after exposure. Treatment involves topical antifungals such as clotrimazole or terbinafine, applied twice daily for 2–4 weeks, depending on severity.
Another type is mycetoma, a chronic granulomatous infection caused by fungi (eumycetoma) or bacteria. Fungi like *Madurella mycetomatis* and *Falciformispora tompkinsii* are common culprits, often entering the skin through cuts or punctures. This infection manifests as firm, painless swelling with sinus tracts that discharge grains or granules. Mycetoma is more prevalent in tropical and subtropical regions, affecting individuals who work outdoors. Treatment is complex, often requiring surgical debridement combined with long-term antifungal therapy, such as itraconazole (200–400 mg/day) for 6–12 months.
Allergic contact dermatitis is a less severe but more common mushroom-related skin issue, triggered by exposure to fungal allergens. For instance, handling raw mushrooms like shiitake (*Lentinula edodes*) can cause "shiitake dermatitis," characterized by a flagellate pattern of erythematous, itchy streaks. This reaction is due to the heat-labile toxin lentinan, found in raw or undercooked mushrooms. Prevention is straightforward: always cook mushrooms thoroughly before consumption or handling. Topical corticosteroids like hydrocortisone 1% cream can alleviate symptoms, applied twice daily for 3–5 days.
Lastly, onychomycosis, or fungal nail infection, can be caused by dermatophytes like *Trichophyton rubrum* or nondermatophyte molds such as *Aspergillus* species. While not exclusively mushroom-related, these fungi are present in environments where mushrooms grow, increasing exposure risk. Symptoms include nail thickening, discoloration, and brittleness. Treatment options include oral antifungals like terbinafine (250 mg/day for 6–12 weeks) or topical solutions such as efinaconazole, applied daily for 48 weeks. Maintaining dry feet and avoiding walking barefoot in damp areas can reduce infection risk.
Understanding these specific types of mushroom-related skin infections allows for targeted prevention and treatment. Whether through antifungal medications, proper mushroom handling, or environmental precautions, awareness is key to minimizing risk and managing symptoms effectively.
Slimy Brown Mushrooms: Safe to Cook or Toss Out?
You may want to see also

Symptoms of Mushroom-Induced Dermatitis
Mushroom-induced dermatitis, though relatively rare, can manifest as a range of skin symptoms following direct contact with certain mushroom species or their spores. The severity and type of reaction depend on the individual’s sensitivity and the specific mushroom involved. Symptoms typically appear within hours to days after exposure, often localized to the area of contact. Recognizing these signs early is crucial for prompt treatment and prevention of complications.
One of the most common symptoms is an erythematous rash, characterized by redness, itching, and mild swelling. This reaction often resembles contact dermatitis and may be accompanied by small blisters or hives. For instance, handling raw *Agaricus bisporus* (common button mushrooms) without gloves has been reported to cause skin irritation in some individuals, particularly those with pre-existing sensitivities. The rash usually resolves within a week with proper care, such as gentle cleansing and application of over-the-counter hydrocortisone cream.
In more severe cases, mushroom-induced dermatitis can lead to vesiculobullous lesions, which are larger, fluid-filled blisters that may rupture and crust over. This is often seen with exposure to toxic species like *Clitocybe acromelalga*, known to cause acromelalga syndrome. Such reactions require medical attention, as they can be painful and may lead to secondary bacterial infections if not managed properly. Avoiding direct skin contact with wild mushrooms and wearing protective gloves when handling unfamiliar species is a practical preventive measure.
Interestingly, systemic symptoms like fever, fatigue, or joint pain may accompany skin reactions in rare instances, particularly if spores are inhaled or if there is a significant allergic response. Children and individuals with compromised immune systems are more susceptible to severe reactions. If symptoms extend beyond localized skin irritation, seeking medical advice is essential. A dermatologist may recommend patch testing to identify specific mushroom allergens and prescribe stronger corticosteroids or antihistamines for relief.
To minimize the risk of mushroom-induced dermatitis, it’s advisable to wash hands thoroughly after handling mushrooms, avoid touching the face during preparation, and ensure proper ventilation when cooking to reduce spore inhalation. While most culinary mushrooms are safe, unfamiliar or wild species should be approached with caution. Understanding the symptoms and taking preventive steps can help individuals enjoy mushrooms without adverse skin reactions.
Mushrooms as Eco-Friendly Alternatives: Can They Replace Greens Sustainably?
You may want to see also

Common Mushroom Species Causing Skin Issues
While mushrooms are celebrated for their culinary and medicinal benefits, certain species can trigger skin infections when handled or consumed. Among the culprits, Dermatophagoides farinae, a fungus commonly found in decaying organic matter, is known to cause allergic reactions and skin irritation in sensitive individuals. Exposure often occurs through inhalation or direct skin contact, leading to symptoms like itching, redness, and hives. For those with compromised immune systems or pre-existing skin conditions, even brief encounters can exacerbate issues. To minimize risk, wear gloves when handling compost or soil, and ensure proper ventilation in damp areas where fungi thrive.
Another notable offender is Trichophyton mentagrophytes, a dermatophyte fungus that can cause ringworm infections in humans. While it primarily infects nails and scalp, it can also lead to skin lesions if transmitted through contaminated surfaces or infected animals. Pet owners, farmers, and gardeners are particularly vulnerable. Prevention involves maintaining good hygiene, avoiding contact with stray animals, and regularly cleaning tools and equipment. If symptoms appear, antifungal creams like clotrimazole or terbinafine can be applied topically, but consult a healthcare provider for persistent cases.
Coprinus comatus, or the shaggy mane mushroom, is generally edible but has been linked to skin irritation in rare cases. Individuals with mushroom allergies may experience contact dermatitis after handling its spores or gills. Symptoms include localized swelling, blisters, or a rash. To avoid this, wash hands thoroughly after foraging or cooking with mushrooms, and consider wearing protective clothing. If irritation occurs, over-the-counter hydrocortisone cream can provide relief, but severe reactions warrant medical attention.
Lastly, Clitocybe dealbata, also known as the ivory funnel, is a toxic mushroom that can cause systemic reactions, including skin manifestations like sweating, flushing, or rashes, when ingested. While not a direct skin infection, these symptoms highlight the importance of accurate identification when foraging. Always consult a mycology guide or expert before consuming wild mushrooms. In case of accidental ingestion, seek immediate medical help, as symptoms can escalate rapidly. Awareness and caution are key to avoiding mushroom-related skin and health issues.
Can K9 Dogs Detect Mushrooms? Exploring Their Olfactory Abilities
You may want to see also
Explore related products

Prevention of Fungal Skin Reactions
Fungal skin infections, though often associated with mold or yeast, can indeed be triggered by certain mushrooms, particularly when their spores come into contact with the skin. While rare, these reactions underscore the importance of proactive prevention strategies. Understanding the conditions that foster fungal growth—warmth, moisture, and compromised skin barriers—is the first step in safeguarding your skin.
Practical Prevention Steps:
Maintain skin dryness, especially in folds and crevices where fungi thrive. After bathing or sweating, thoroughly dry areas like the armpits, groin, and feet. Opt for breathable fabrics like cotton or moisture-wicking materials, and change out of damp clothing promptly. For those prone to fungal infections, dusting antifungal powders (e.g., miconazole or clotrimazole) in at-risk areas can create a protective barrier. Avoid sharing personal items like towels or shoes, as fungi can transfer easily.
Environmental Awareness:
Mushrooms and fungi flourish in damp, organic environments, so limit prolonged exposure to such settings. When gardening, foraging, or hiking in wooded areas, wear gloves and long sleeves to minimize skin contact with spores. After outdoor activities, wash hands and exposed skin thoroughly. If handling mushrooms, whether wild or store-bought, avoid touching your face or open wounds, as spores can enter through breaks in the skin.
Strengthening Skin Defenses:
A healthy skin barrier is your best defense against fungal invaders. Moisturize regularly with non-comedogenic lotions to prevent dryness and cracking, which can invite infection. For individuals with conditions like eczema or diabetes, diligent skin care is critical, as compromised skin is more susceptible. Incorporate probiotics or fermented foods into your diet to support a balanced microbiome, which can indirectly reduce fungal overgrowth.
Early Detection and Intervention:
Recognize the signs of fungal infections—itching, redness, scaling, or blisters—and act swiftly. Over-the-counter antifungal creams (e.g., terbinafine or ketoconazole) are effective for mild cases, but follow dosage instructions carefully (typically twice daily for 2–4 weeks). For persistent or severe infections, consult a dermatologist, as oral medications or stronger treatments may be necessary. Regularly inspect skin, especially after potential exposures, to catch issues early.
By combining vigilance, hygiene, and environmental awareness, you can significantly reduce the risk of fungal skin reactions, even those linked to mushrooms. Prevention is not just about avoiding fungi but about creating an environment where they cannot take hold.
Diverticulitis Diet: Are Mushrooms and Cheese Safe to Eat?
You may want to see also

Treatment Options for Mushroom Skin Infections
Mushroom-related skin infections, though rare, can occur when fungal spores come into contact with the skin, leading to conditions like ringworm or dermatitis. Treatment options vary depending on the severity and type of infection, but they generally involve antifungal medications, topical creams, and preventive measures. Here’s a focused guide on managing these infections effectively.
Step-by-Step Treatment Approach: For mild cases, over-the-counter antifungal creams containing clotrimazole (1%) or miconazole (2%) are often sufficient. Apply the cream twice daily to the affected area for 2–4 weeks, ensuring the skin is clean and dry before application. For more persistent infections, oral antifungal medications like terbinafine (250 mg daily for adults) or itraconazole (200 mg daily) may be prescribed by a healthcare provider. Always complete the full course of medication, even if symptoms improve, to prevent recurrence.
Cautions and Considerations: Avoid self-diagnosis, as symptoms like redness, itching, or rashes can mimic other skin conditions. Consult a dermatologist for a proper diagnosis, especially if the infection spreads or worsens. Individuals with weakened immune systems, such as those on immunosuppressive therapy or with diabetes, should seek immediate medical attention, as they are at higher risk for severe infections. Additionally, avoid sharing personal items like towels or clothing to prevent fungal spores from spreading.
Preventive Measures: To minimize the risk of mushroom-related skin infections, wear gloves when handling mushrooms or working in damp environments where fungi thrive. Keep skin dry and clean, especially in folds and crevices where moisture can accumulate. Regularly wash and dry clothing, bedding, and other fabrics that come into contact with the skin. For those prone to fungal infections, incorporating antifungal powders or sprays into daily routines can provide an extra layer of protection.
Natural Remedies and Lifestyle Adjustments: While medical treatments are often necessary, complementary approaches can support healing. Tea tree oil, diluted to 5–10% in a carrier oil, has antifungal properties and can be applied topically to affected areas. Maintaining a balanced diet rich in probiotics and vitamins can also strengthen the immune system, aiding in infection prevention. However, natural remedies should not replace prescribed treatments but rather complement them under professional guidance.
Mushrooms and Cancer: Safe or Risky for Patients to Eat?
You may want to see also
Frequently asked questions
Mushrooms themselves do not typically cause skin infections. However, handling certain mushrooms or coming into contact with their spores can irritate the skin or trigger allergic reactions in some individuals.
Some mushrooms, like the Poison Ivy mushroom (*Dacrymyces tortus*), can cause skin irritation or allergic dermatitis in sensitive individuals. Additionally, mold fungi (not true mushrooms) like *Aspergillus* or *Penicillium* can lead to skin infections if they grow on the skin.
Eating mushrooms rarely causes skin infections, but consuming toxic or allergenic species can lead to systemic reactions, including skin rashes, hives, or itching. Always ensure mushrooms are properly identified and cooked before consumption.