The question of whether mushrooms can cure herpes has gained attention in recent years, driven by growing interest in natural remedies and the medicinal properties of fungi. While scientific research on this topic is still limited, certain mushroom species, such as *Reishi* (*Ganoderma lucidum*) and *Turkey Tail* (*Trametes versicolor*), have been studied for their antiviral and immune-boosting effects. These mushrooms contain bioactive compounds like polysaccharides and beta-glucans, which may help strengthen the immune system and potentially inhibit viral activity. However, there is no conclusive evidence to suggest that mushrooms can cure herpes, a viral infection caused by the herpes simplex virus (HSV). Current treatments focus on antiviral medications to manage symptoms and reduce outbreaks, and while mushrooms may offer supportive benefits, they should not replace conventional medical advice. Further research is needed to explore their potential role in herpes management.
| Characteristics | Values |
|---|---|
| Scientific Evidence | Limited; some studies suggest antiviral properties in certain mushrooms, but no conclusive evidence for herpes cure |
| Mushroom Types Mentioned | Reishi (Ganoderma lucidum), Shiitake (Lentinula edodes), Turkey Tail (Trametes versicolor), Maitake (Grifola frondosa) |
| Antiviral Properties | Some mushrooms contain compounds like beta-glucans, polysaccharides, and terpenoids with potential antiviral effects |
| Herpes Types | Herpes Simplex Virus (HSV-1 and HSV-2); no specific mushroom-based cure identified |
| Traditional Medicine | Used in traditional Chinese and Japanese medicine for immune support, but not specifically for herpes |
| Clinical Trials | Few human trials; most studies are in vitro (lab-based) or animal models |
| Safety Concerns | Generally considered safe, but allergic reactions or interactions with medications possible |
| FDA Approval | No mushroom-based products approved by FDA for herpes treatment |
| Expert Consensus | Not recognized as a standard or effective treatment for herpes by medical professionals |
| Alternative Uses | Immune system support, potential adjunct therapy, but not a cure |
| Availability | Widely available as supplements, teas, or extracts, but quality and efficacy vary |
| Conclusion | No scientific evidence supports mushrooms as a cure for herpes; further research needed |
Explore related products
What You'll Learn
- Medicinal Mushroom Types: Exploring varieties like Reishi, Chaga, and Turkey Tail for antiviral properties
- Immune System Boost: How mushrooms enhance immunity to combat herpes outbreaks effectively
- Antiviral Compounds: Identifying active compounds in mushrooms that target herpes viruses
- Scientific Studies: Reviewing research on mushrooms' efficacy against herpes simplex virus
- Usage Methods: Capsules, teas, or extracts—best ways to consume mushrooms for herpes treatment

Medicinal Mushroom Types: Exploring varieties like Reishi, Chaga, and Turkey Tail for antiviral properties
Reishi, Chaga, and Turkey Tail mushrooms have long been revered in traditional medicine for their immune-boosting and antiviral properties. While scientific research on their ability to "cure" herpes is limited, these fungi contain bioactive compounds that may help manage symptoms and support the immune system’s response to the virus. Reishi, for instance, is rich in beta-glucans and triterpenes, which have been shown to modulate immune function and reduce inflammation. Chaga, with its high antioxidant content, may protect cells from viral damage, while Turkey Tail’s polysaccharide-K (PSK) has been studied for its role in enhancing immune activity. Though not a cure, these mushrooms offer a complementary approach to managing herpes outbreaks.
For those considering medicinal mushrooms, dosage and preparation matter. Reishi is commonly consumed as a tea or tincture, with recommended doses ranging from 1.5 to 9 grams daily, depending on the form. Chaga, often brewed as a decoction, can be taken in 1-2 cups per day, though its bitter taste may require blending with other herbs or sweeteners. Turkey Tail is typically consumed as a tea or in capsule form, with doses of 2-3 grams daily. It’s crucial to source these mushrooms from reputable suppliers to ensure purity and avoid contamination. Always consult a healthcare provider before starting any new supplement, especially if you’re pregnant, nursing, or on medication.
Comparing these mushrooms reveals distinct strengths. Reishi excels in stress reduction and immune modulation, making it ideal for those experiencing herpes outbreaks triggered by stress. Chaga’s potent antioxidant profile may help mitigate cellular damage caused by viral activity, while Turkey Tail’s PSK has been extensively studied for its immunostimulatory effects, particularly in cancer patients. However, none of these mushrooms act as a direct antiviral agent against herpes. Instead, their value lies in supporting the body’s natural defenses, potentially reducing the frequency and severity of outbreaks.
Practical tips for incorporating these mushrooms into your routine include combining them with other immune-supporting practices, such as a balanced diet, regular exercise, and adequate sleep. For example, pairing Reishi tea with mindfulness practices can enhance its stress-relieving effects. Chaga can be added to smoothies or soups to mask its flavor, while Turkey Tail capsules offer a convenient option for those with busy lifestyles. While medicinal mushrooms are generally safe, individual reactions vary, so start with lower doses and monitor your body’s response. Remember, they are not a replacement for antiviral medications but can serve as a valuable adjunct in holistic herpes management.
Mushrooms Under Cherry Trees: Exploring the Symbiotic Relationship
You may want to see also

Immune System Boost: How mushrooms enhance immunity to combat herpes outbreaks effectively
Mushrooms have long been celebrated for their immune-boosting properties, and their potential to combat herpes outbreaks is a topic of growing interest. Herpes, a viral infection characterized by periodic outbreaks, relies heavily on the body’s immune response for management. Certain mushrooms, rich in beta-glucans and other bioactive compounds, have been shown to modulate immune function, potentially reducing the frequency and severity of herpes outbreaks. For instance, *Reishi* (*Ganoderma lucidum*) and *Turkey Tail* (*Trametes versicolor*) are among the most studied varieties for their antiviral and immunomodulatory effects. Incorporating these mushrooms into your regimen could be a natural, complementary approach to managing herpes symptoms.
To harness the immune-boosting power of mushrooms effectively, consider both dietary and supplemental forms. Adding shiitake, maitake, or lion’s mane mushrooms to meals provides a culinary way to benefit from their nutrients. For a more concentrated dose, supplements like *Reishi* or *Cordyceps* extracts are available in capsules, powders, or tinctures. Dosage varies by type and form, but a common recommendation is 1–3 grams of mushroom extract daily, divided into two doses. Always consult a healthcare provider before starting any new supplement, especially if you’re pregnant, nursing, or on medication. Consistency is key—immune modulation takes time, so expect to use these mushrooms for several weeks to notice effects.
While mushrooms offer promising immune support, they are not a standalone cure for herpes. Their role is to strengthen the immune system, making it more resilient against viral activity. Pairing mushroom use with other immune-boosting strategies, such as adequate sleep, stress management, and a balanced diet, maximizes their effectiveness. For example, combining *Turkey Tail* supplements with vitamin C and zinc may enhance overall immune function. However, avoid excessive dosages, as overstimulating the immune system can have adverse effects. Practical tips include brewing *Reishi* tea before bed to promote relaxation or adding powdered mushroom extracts to smoothies for easy consumption.
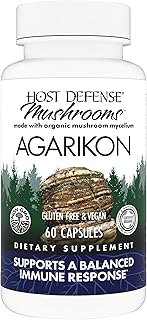
Comparatively, mushrooms stand out from other natural remedies for herpes due to their dual action: they not only support immunity but also exhibit direct antiviral properties in some cases. Studies suggest that *Chaga* and *Agaricus blazei* mushrooms may inhibit viral replication, though research is still emerging. This makes them a multifaceted tool in managing herpes, unlike single-action remedies like lysine supplements. However, their efficacy varies by individual, and results may take longer to manifest compared to pharmaceutical antivirals. For those seeking a holistic approach, mushrooms offer a sustainable, side-effect-minimized option when used thoughtfully and consistently.
Growing Mushrooms from Rye Berries: A Simple Guide for Beginners
You may want to see also

Antiviral Compounds: Identifying active compounds in mushrooms that target herpes viruses
Mushrooms have long been celebrated for their medicinal properties, but their potential to combat herpes viruses remains a fascinating and under-explored area. Recent studies have identified specific antiviral compounds in mushrooms, such as polysaccharides, terpenoids, and lectins, which exhibit inhibitory effects on herpes simplex virus (HSV) types 1 and 2. For instance, research on *Ganoderma lucidum* (Reishi) and *Trametes versicolor* (Turkey Tail) has revealed beta-glucans that can modulate the immune response, potentially reducing viral replication. These findings suggest that mushrooms could offer a natural, complementary approach to managing herpes infections, though clinical trials are still needed to establish efficacy and safety.
To identify active compounds in mushrooms targeting herpes viruses, researchers employ a systematic approach. First, mushroom extracts are screened for antiviral activity using in vitro assays, such as plaque reduction tests or viral yield assays. Compounds showing promise are then isolated and characterized using techniques like high-performance liquid chromatography (HPLC) and mass spectrometry. For example, a study on *Agaricus blazei* identified a protein called blazein, which demonstrated significant anti-HSV activity by inhibiting viral entry into host cells. This process not only highlights the potential of mushrooms but also underscores the importance of rigorous scientific methods in validating their therapeutic use.
While the idea of mushrooms curing herpes is intriguing, practical application requires careful consideration of dosage and form. For instance, Reishi mushroom supplements are often available in capsule or tincture form, with recommended dosages ranging from 1.5 to 9 grams daily for immune support. However, for antiviral effects, higher concentrations of specific compounds like triterpenes may be necessary. It’s crucial to consult a healthcare provider before incorporating mushroom-based treatments, especially for individuals with underlying health conditions or those taking other medications. Additionally, sourcing high-quality, lab-tested products ensures purity and potency, minimizing the risk of contamination or ineffective formulations.
Comparing mushrooms to conventional antiviral medications like acyclovir or valacyclovir reveals both advantages and limitations. While pharmaceutical drugs are proven to suppress herpes outbreaks effectively, they often come with side effects such as nausea or kidney issues. Mushrooms, on the other hand, offer a holistic approach with potential immunomodulatory benefits but lack the immediate potency of synthetic drugs. Combining the two could be a strategic option, leveraging mushrooms’ supportive role while relying on medications for acute management. This comparative perspective highlights the need for integrated treatment plans tailored to individual needs.
In conclusion, the quest to identify antiviral compounds in mushrooms targeting herpes viruses is a promising yet complex endeavor. From laboratory screenings to practical applications, the process demands precision, patience, and collaboration across disciplines. While mushrooms may not yet be a cure, their active compounds offer a compelling avenue for further research and potential integration into herpes management strategies. As science continues to unravel their mysteries, mushrooms could emerge as valuable allies in the fight against this persistent viral infection.
Mushrooms and Menstruation: Are They Safe to Eat During Periods?
You may want to see also
Explore related products

Scientific Studies: Reviewing research on mushrooms' efficacy against herpes simplex virus
The herpes simplex virus (HSV) affects billions globally, with treatments limited to symptom management rather than cure. Amid growing interest in natural remedies, mushrooms have emerged as a potential candidate due to their antiviral properties. Scientific studies have begun to explore whether compounds in mushrooms like polysaccharides, terpenoids, and lectins can inhibit HSV replication or reduce outbreak severity. However, the research remains in its early stages, with most studies conducted in vitro or on animal models, leaving a gap in human clinical trials.
One notable compound, ahcc (active hexose correlated compound), derived from shiitake mushrooms, has shown promise in boosting immune response against HSV. A 2014 study published in *Nutrition Research* found that AHCC supplementation reduced viral load and lesion duration in mice infected with HSV-2. While this suggests potential for immune modulation, the study’s dosage (50 mg/kg daily) cannot be directly translated to humans without further research. Similarly, reishi mushroom (Ganoderma lucidum) has been investigated for its triterpenoids, which demonstrated antiviral activity against HSV-1 in a 2017 *Virology Journal* study. However, the effective concentration (500 μg/mL) was achieved in a lab setting, far from practical oral supplementation levels.
In contrast, turkey tail mushroom (Coriolus versicolor) has been studied for its polysaccharide-K (PSK), a compound approved in Japan for cancer therapy. A 2012 *Antiviral Research* study found PSK inhibited HSV-1 replication in cell cultures by 80% at a concentration of 100 μg/mL. While this is promising, the mechanism of action remains unclear, and no human trials have been conducted for herpes. Such discrepancies highlight the need for standardized dosing and long-term safety studies before mushrooms can be recommended as a treatment.
For those considering mushroom-based remedies, practical tips include starting with low doses of commercially available supplements (e.g., 1–3 grams of reishi or AHCC daily) and monitoring for side effects like digestive discomfort. Combining mushrooms with conventional antiviral medications like acyclovir may enhance efficacy, but this should only be done under medical supervision. Pregnant or immunocompromised individuals should avoid unproven supplements due to potential risks. While mushrooms offer intriguing possibilities, their role in herpes management remains experimental, and reliance on FDA-approved treatments is currently advised.
Can You Eat Mushrooms on the HCG Diet? Facts Revealed
You may want to see also

Usage Methods: Capsules, teas, or extracts—best ways to consume mushrooms for herpes treatment
Mushrooms have been explored for their potential antiviral properties, but their role in treating herpes remains largely anecdotal. When considering usage methods—capsules, teas, or extracts—each offers distinct advantages and challenges. Capsules provide a convenient, measured dose, typically ranging from 500 mg to 1,000 mg per serving, making them ideal for those seeking precision and ease. However, bioavailability can be lower compared to other methods, as the digestive system must break down the capsule before absorption occurs. For individuals with sensitive stomachs or those who prefer a quick, no-fuss approach, capsules may be the best starting point.
Teas, on the other hand, offer a more traditional and soothing method of consumption. Brewing mushroom teas involves steeping dried or powdered mushrooms in hot water for 10–15 minutes, allowing for the extraction of water-soluble compounds. This method is particularly appealing for those who enjoy rituals like tea-making and prefer a gradual release of potential therapeutic effects. However, determining an exact dosage can be tricky, and the taste may be unpalatable for some. Adding honey or lemon can improve flavor while potentially enhancing absorption, though this remains speculative in the context of herpes treatment.
Extracts, often in tincture or liquid form, are highly concentrated and designed for sublingual or oral use. A typical dose might range from 1–2 droppers (around 2–4 ml) per day, depending on the concentration. This method boasts higher bioavailability, as the compounds are absorbed directly into the bloodstream through the mucous membranes. Extracts are ideal for those seeking potent, fast-acting relief, but their strong flavor and higher cost may be deterrents. Additionally, quality varies widely among brands, so sourcing from reputable suppliers is critical.
Comparing these methods, capsules offer convenience but lower bioavailability, teas provide a gentle approach with uncertain dosing, and extracts deliver potency at a premium. For herpes treatment, where consistency and efficacy are key, combining methods—such as taking capsules daily while using extracts during outbreaks—may yield the best results. Always consult a healthcare provider before starting any regimen, especially if you’re pregnant, nursing, or on medication. Practical tips include starting with lower doses to assess tolerance and keeping a symptom journal to track effectiveness. While mushrooms show promise, they are not a substitute for prescribed antiviral medications but may serve as a complementary approach.
Safe Mushroom Consumption: How Often Can You Take Them?
You may want to see also
Frequently asked questions
There is no scientific evidence to support the claim that mushrooms can cure herpes. While some mushrooms have antiviral properties, they are not a proven treatment for herpes, and medical advice should always be sought for managing the condition.
Certain mushrooms, like reishi or turkey tail, are studied for their immune-boosting and antiviral effects, but they are not a cure for herpes. They may support overall health but should not replace prescribed treatments.
Mushroom supplements may support immune function, but they are not proven to prevent herpes outbreaks. Antiviral medications and lifestyle changes remain the most effective ways to manage the virus. Always consult a healthcare provider for guidance.