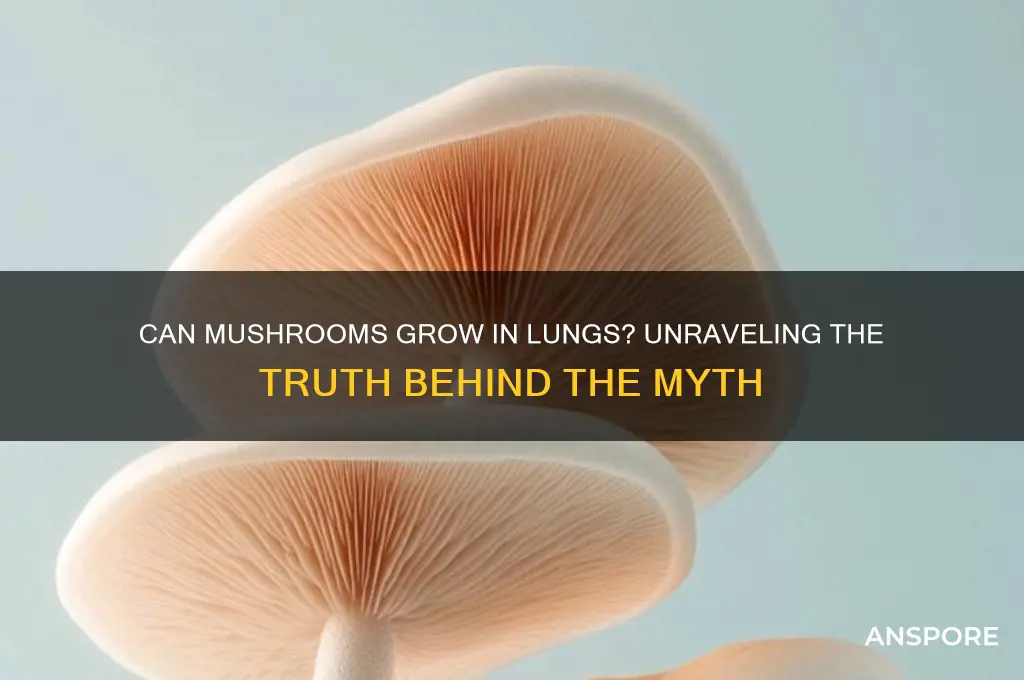
The idea of mushrooms growing in human lungs may sound like something out of a science fiction novel, but it has been a topic of both medical curiosity and urban legend. While mushrooms typically thrive in environments rich in organic matter, moisture, and specific nutrients, the human lung is an inhospitable place for fungal growth due to its sterile, warm, and oxygen-rich conditions. However, rare cases of fungal infections, such as aspergillosis, have been documented where mold-like fungi can colonize the lungs, often in individuals with compromised immune systems or pre-existing lung conditions. The concept of actual mushrooms, with their complex structures, growing in lungs remains biologically implausible, though it continues to spark fascination and misinformation.
| Characteristics | Values |
|---|---|
| Can mushrooms grow in lungs? | No, mushrooms cannot grow in human lungs under normal circumstances. |
| Reason for myth | Misinterpretation of rare cases of fungal infections in lungs, which are not mushrooms but molds or yeasts. |
| Fungal infections in lungs | Possible, caused by fungi like Aspergillus, Candida, or Cryptococcus, but these are not mushrooms. |
| Conditions for fungal growth | Requires specific environment (e.g., compromised immune system, exposure to fungal spores). |
| Symptoms of fungal lung infections | Cough, fever, chest pain, difficulty breathing, fatigue. |
| Diagnosis | Imaging tests (X-rays, CT scans), fungal cultures, or biopsies. |
| Treatment | Antifungal medications, surgery in severe cases. |
| Prevention | Avoid exposure to fungal spores, maintain good hygiene, manage underlying health conditions. |
| Scientific consensus | Mushrooms (basidiomycetes) cannot grow in human lungs; fungal infections are caused by different types of fungi. |
Explore related products
What You'll Learn

Can mushroom spores germinate inside human lungs?
Mushroom spores are remarkably resilient, capable of surviving in extreme environments, from arid deserts to radioactive zones. However, the human lung presents a unique challenge. For germination to occur, spores require specific conditions: adequate moisture, nutrients, and a suitable substrate. The lung environment, while humid, lacks the organic matter and stable conditions necessary for fungal growth. Spores that enter the lungs are more likely to be cleared by the immune system or trapped in mucus, rather than finding a hospitable niche for development.
Consider the biological barriers at play. The human respiratory system is designed to filter and expel foreign particles. When inhaled, mushroom spores typically become lodged in the upper airways or are engulfed by macrophages, immune cells that neutralize potential threats. Even if spores reach the alveoli, the microscopic air sacs where gas exchange occurs, they face a nutrient-poor environment. Unlike soil or decaying wood, lung tissue does not provide the carbohydrates, proteins, and minerals essential for fungal metabolism. Without these resources, spores remain dormant or perish.
A comparative analysis highlights the stark contrast between lung tissue and natural fungal habitats. Mushrooms thrive in environments rich in cellulose, lignin, and other complex organic compounds, which they break down using enzymes. In contrast, lung tissue is composed primarily of proteins, lipids, and water, with no accessible energy sources for fungi. Additionally, the lung’s dynamic environment—subject to constant ventilation, temperature fluctuations, and immune surveillance—further inhibits spore germination. While rare cases of fungal infections like aspergillosis exist, these involve opportunistic pathogens adapted to exploit compromised immune systems, not common mushroom species.
For those concerned about exposure, practical precautions can minimize risk. Avoid inhaling dust from moldy environments, where fungal spores may concentrate. Individuals with respiratory conditions or weakened immunity should use N95 masks in areas with visible mold or decaying organic matter. If accidental inhalation occurs, monitor for symptoms like persistent coughing, fever, or chest pain, and seek medical attention if they arise. While mushroom spores in the lungs are unlikely to germinate, vigilance against fungal pathogens remains crucial, especially in immunocompromised populations.
Mushrooms in Horse Manure: Unveiling the Surprising Growth Potential
You may want to see also

Cases of fungal infections resembling mushrooms in lungs
Fungal infections in the lungs, while rare, have occasionally presented with growths that resemble mushrooms in medical imaging. These cases, though not literal mushrooms, highlight the invasive nature of certain fungi and their ability to form mass-like structures within the pulmonary tissue. One notable example is aspergillosis, caused by the Aspergillus fungus, which can lead to the formation of aspergillomas—fungal balls that appear as distinct, mushroom-like lesions on X-rays or CT scans. Such infections typically occur in individuals with pre-existing lung conditions, such as tuberculosis cavities or chronic obstructive pulmonary disease (COPD), where the fungus colonizes damaged lung tissue.
Diagnosing these infections requires a combination of imaging and laboratory tests. High-resolution CT scans often reveal characteristic features like the "air crescent sign" in aspergillomas, where the fungal mass is surrounded by a crescent of air. Sputum cultures and serum antibody tests can confirm the presence of the fungus, though biopsy remains the gold standard for definitive diagnosis. Early detection is critical, as delayed treatment can lead to complications such as hemoptysis (coughing up blood) or the spread of the infection to other organs.
Treatment strategies vary depending on the severity and type of infection. For aspergillomas, surgical resection may be necessary if the fungal ball causes significant bleeding or fails to respond to antifungal therapy. Antifungal medications like voriconazole or itraconazole are commonly prescribed, with dosages tailored to the patient’s age, weight, and renal function. For instance, voriconazole is typically administered at 6 mg/kg every 12 hours for adults, while pediatric dosing is adjusted based on body surface area. Adjunctive therapies, such as bronchial artery embolization for hemoptysis, may also be employed in severe cases.
Preventive measures are particularly important for at-risk populations, including immunocompromised individuals and those with chronic lung diseases. Avoiding environments with high fungal spore counts, such as construction sites or compost piles, can reduce exposure. For patients with COPD or cystic fibrosis, regular pulmonary function tests and imaging can help identify early signs of fungal colonization. In healthcare settings, strict infection control practices, such as HEPA filtration in ventilation systems, are essential to prevent nosocomial outbreaks.
While the idea of "mushrooms growing in lungs" remains a medical curiosity rather than a literal phenomenon, these cases underscore the importance of recognizing and managing fungal infections promptly. By understanding the clinical presentation, diagnostic tools, and treatment options, healthcare providers can improve outcomes for patients with these rare but potentially life-threatening conditions. Public awareness and proactive monitoring, especially in vulnerable populations, play a crucial role in preventing the progression of such infections.
Mushrooms in Granola: Unlikely Growth or Culinary Myth Explored
You may want to see also

Conditions required for mushrooms to grow in lungs
Mushrooms require specific conditions to thrive, and the human lung environment is not naturally conducive to their growth. However, rare cases of fungal infections, such as aspergillosis, have raised questions about whether mushrooms could theoretically grow in lungs. For this to occur, several critical conditions must align: a compromised immune system, the presence of organic matter, and a humid, warm environment. While mushrooms typically need soil or decaying material to grow, the lungs’ sterile, nutrient-poor environment presents a significant barrier. Yet, in cases of severe immunosuppression or foreign bodies in the lungs, the possibility becomes slightly less far-fetched.
Analyzing the conditions further, temperature and humidity play pivotal roles. Mushrooms thrive in temperatures between 55°F and 60°F (13°C and 15°C), which is cooler than the human body’s 98.6°F (37°C). This mismatch makes lung growth unlikely unless external factors, such as prolonged exposure to cooler environments, are involved. Humidity, however, is less of an issue, as the lungs naturally maintain a moist environment. The real challenge lies in the absence of a substrate—mushrooms need organic material to decompose, which the lungs do not provide unless there is an unusual presence of foreign debris or dead tissue.
From a practical standpoint, preventing such conditions is far more feasible than addressing them after they arise. For individuals with weakened immune systems, such as those undergoing chemotherapy, organ transplant recipients, or individuals with HIV/AIDS, regular medical monitoring is essential. Avoiding environments with high fungal spore counts, such as damp basements or compost piles, can reduce the risk of fungal infections. Additionally, maintaining good respiratory hygiene, such as wearing masks in dusty or moldy areas, can minimize spore inhalation. These precautions are critical, as once a fungal infection takes hold, treatment can be complex and prolonged.
Comparatively, while plants and some bacteria can adapt to extreme environments, mushrooms lack the biological mechanisms to survive in the lungs’ harsh conditions. Their growth cycle relies on external nutrients and specific environmental cues, neither of which are present in healthy lungs. However, in rare instances where foreign objects (e.g., aspirated food or medical devices) create localized pockets of organic material, the theoretical possibility of fungal growth emerges. Such cases are documented in medical literature but remain exceptionally rare, often requiring a perfect storm of circumstances.
In conclusion, while the conditions required for mushrooms to grow in lungs are highly specific and unlikely, they are not impossible. A compromised immune system, the presence of foreign organic material, and a humid environment are the key factors. For the general population, the risk is negligible, but for immunocompromised individuals, vigilance and preventive measures are crucial. Understanding these conditions not only satisfies curiosity but also underscores the importance of respiratory health and immune function in preventing rare but serious complications.
Can Mushrooms Thrive Without Oxygen? Exploring Anaerobic Growth Conditions
You may want to see also
Explore related products

Medical risks of fungal growth in lung tissue
Fungal growth in lung tissue, though rare, poses significant medical risks that demand attention. Unlike superficial infections, pulmonary fungal infections can lead to severe complications, particularly in immunocompromised individuals. Aspergillus, Cryptococcus, and Histoplasma are common culprits, infiltrating the lungs through inhalation of spores. These fungi thrive in environments with weakened immune defenses, such as in patients undergoing chemotherapy, living with HIV/AIDS, or taking long-term corticosteroids. The insidious nature of these infections often delays diagnosis, allowing the fungi to colonize and damage lung tissue progressively.
Consider the case of aspergillosis, a condition caused by Aspergillus molds. In healthy individuals, inhaled spores are typically cleared by the immune system. However, in those with compromised immunity, the spores germinate into hyphae, invading lung tissue and blood vessels. This can lead to conditions like allergic bronchopulmonary aspergillosis (ABPA), a hypersensitive reaction in asthmatics, or invasive aspergillosis, which carries a mortality rate exceeding 50% in severe cases. Early symptoms—cough, fever, and chest pain—often mimic other respiratory conditions, complicating timely intervention.
Preventive measures are critical for at-risk populations. Immunocompromised patients should avoid environments with high fungal spore counts, such as construction sites or areas with visible mold. Prophylactic antifungal medications, like posaconazole or itraconazole, may be prescribed for high-risk individuals, particularly during neutropenic phases of chemotherapy. For those diagnosed with fungal lung infections, treatment typically involves antifungal agents such as voriconazole or amphotericin B, often administered intravenously for systemic reach. Adherence to treatment regimens is paramount, as incomplete courses can lead to drug resistance and recurrent infections.
Comparatively, fungal lung infections differ from bacterial or viral pneumonias in their chronicity and treatment complexity. While bacterial infections often respond swiftly to antibiotics, fungi require prolonged antifungal therapy, sometimes lasting months. Surgical intervention may be necessary in cases of severe tissue damage, such as cavitary lesions or fungal balls, which can obstruct airways or lead to hemoptysis. Unlike viral infections, fungal pathogens do not elicit herd immunity, making prevention and early detection the cornerstone of management.
In conclusion, the medical risks of fungal growth in lung tissue are profound and multifaceted. From allergic reactions to life-threatening invasive diseases, these infections demand vigilance, particularly in vulnerable populations. By understanding the pathogens, recognizing early symptoms, and implementing preventive strategies, healthcare providers and patients can mitigate the risks associated with this silent yet dangerous threat. Awareness and proactive management remain the most effective tools in combating fungal colonization of the lungs.
Can Mushrooms Thrive in Partially Colonized Jars? Growing Tips
You may want to see also

Differences between lung fungi and actual mushrooms
Lung fungi and mushrooms, though both fungi, differ fundamentally in their biology, habitat, and impact on human health. While mushrooms are macroscopic, spore-producing structures that grow in soil, wood, or other organic matter, lung fungi are microscopic organisms that can colonize the respiratory system. The key distinction lies in their environment: mushrooms require external substrates to thrive, whereas lung fungi adapt to the warm, moist conditions of the human lung. This adaptation allows lung fungi to evade the immune system and establish infections, a feat impossible for mushrooms due to their size and growth requirements.
Consider the case of *Aspergillus*, a common lung fungus that causes aspergillosis. Unlike mushrooms, which grow visible fruiting bodies, *Aspergillus* exists as a network of thread-like hyphae in the lungs. These hyphae can invade lung tissue, particularly in immunocompromised individuals, leading to conditions like allergic bronchopulmonary aspergillosis (ABPA). Treatment often involves antifungal medications such as itraconazole (200–400 mg/day) or voriconazole (200 mg twice daily), tailored to the patient’s age and immune status. In contrast, mushrooms lack the ability to penetrate human tissue and are not pathogenic in this manner.
From a comparative perspective, the lifecycle of lung fungi and mushrooms highlights their differences. Mushrooms reproduce by releasing spores into the air, which then land on suitable substrates to grow. Lung fungi, however, must adapt to survive in the hostile environment of the respiratory tract. For instance, *Pneumocystis jirovecii*, a lung fungus causing pneumonia in HIV/AIDS patients, has a unique lifecycle involving both asexual and sexual reproduction within the lungs. This intracellular parasitism is a stark contrast to mushrooms, which are free-living organisms with no interaction with human cells.
Practically speaking, preventing lung fungal infections involves reducing exposure to fungal spores, especially in high-risk environments like construction sites or gardens. Wearing N95 masks and maintaining good indoor air quality can minimize inhalation of spores. For those with compromised immunity, prophylactic antifungal therapy may be recommended. Conversely, mushrooms pose no such risk, as their spores, while ubiquitous, do not colonize human tissue. Understanding these differences is crucial for accurate diagnosis and treatment, ensuring that lung fungi are not mistaken for harmless mushrooms in medical contexts.
Mushrooms in Coal Dust: Unlikely Growth or Ecological Innovation?
You may want to see also
Frequently asked questions
No, mushrooms cannot grow in human lungs. Mushrooms require specific conditions like soil, moisture, and organic matter to grow, which are not present in the human body.
There are no scientifically verified cases of mushrooms growing inside human lungs. Such claims are often myths or misunderstandings.
Yes, fungal infections like aspergillosis can cause mold or fungus to grow in the lungs, but these are not mushrooms. They are different types of fungi that can infect humans.
Inhaling mushroom spores is unlikely to cause them to grow in the lungs. The human body’s environment is not suitable for mushroom growth, and the immune system typically clears foreign particles like spores.