While mushrooms are typically associated with damp, dark environments like forests and gardens, the idea of them growing on human feet is a common misconception. Mushrooms require specific conditions to thrive, including a substrate rich in organic matter, adequate moisture, and often a symbiotic relationship with other organisms. Human skin, however, lacks the necessary nutrients and environment for mushrooms to grow. What people often mistake for mushrooms on their feet are actually fungal infections, such as athlete’s foot, caused by dermatophytes—fungi that feed on keratin in the skin, hair, and nails. These infections manifest as itching, redness, and peeling, but they are not mushrooms. Understanding the difference between fungal infections and actual mushrooms is crucial for proper treatment and prevention.
| Characteristics | Values |
|---|---|
| Can mushrooms grow on your feet? | No |
| Reason | Mushrooms require specific conditions to grow, including a substrate rich in organic matter, moisture, and warmth. Human skin does not provide the necessary nutrients or environment for mushroom growth. |
| Common misconceptions | Fungal infections like athlete's foot (tinea pedis) are often mistaken for mushrooms due to their appearance, but they are caused by fungi, not mushrooms. |
| Fungal infections on feet | Common, caused by dermatophytes (e.g., Trichophyton), leading to itching, redness, and peeling skin. |
| Mushroom growth requirements | Organic substrate (e.g., wood, soil), high humidity, warmth, and darkness. |
| Human skin conditions | Not suitable for mushroom growth due to lack of organic nutrients and constant shedding of skin cells. |
| Prevention of fungal infections | Keep feet clean and dry, wear breathable footwear, and avoid walking barefoot in public areas. |
| Treatment of fungal infections | Antifungal creams, powders, or oral medications prescribed by a healthcare professional. |
| Related conditions | Toenail fungus (onychomycosis), jock itch (tinea cruris), and ringworm (tinea corporis). |
Explore related products
What You'll Learn

Causes of Fungal Infections
Fungal infections on the feet, often referred to as athlete’s foot (tinea pedis), are caused by dermatophytes—microscopic fungi that thrive in warm, moist environments. These organisms feed on keratin, a protein found in skin, hair, and nails, making the feet an ideal breeding ground. Unlike mushrooms, which require soil and specific conditions to grow, dermatophytes are adapted to human skin, though their presence can lead to symptoms resembling moldy, mushroom-like patches. Understanding the causes of these infections is the first step in prevention and treatment.
Environmental Factors: The Breeding Ground for Fungi
Fungi flourish in damp, humid conditions, making sweaty shoes and socks prime culprits. Prolonged exposure to moisture softens the skin, allowing fungi to penetrate more easily. Public spaces like locker rooms, swimming pools, and communal showers are common sources of infection, as fungi can survive on surfaces for weeks. Wearing tight, non-breathable footwear further exacerbates the issue by trapping sweat and heat. To minimize risk, opt for moisture-wicking socks, rotate shoes daily to allow them to dry, and avoid walking barefoot in public areas.
Lifestyle and Health Conditions: Who’s at Risk?
Certain habits and health conditions increase susceptibility to fungal infections. People with diabetes, compromised immune systems, or poor circulation are more vulnerable, as their bodies struggle to fight off infections. Sharing personal items like towels or shoes can also spread fungi. Additionally, age plays a role—older adults are more prone due to reduced skin integrity and slower healing. For those at risk, daily foot inspections and prompt treatment of cuts or blisters are essential. Over-the-counter antifungal creams (e.g., clotrimazole 1%) can be effective for mild cases, but severe infections may require prescription medications.
Prevention Strategies: A Proactive Approach
Preventing fungal infections requires a combination of hygiene and awareness. After bathing, thoroughly dry your feet, especially between the toes, where fungi often take hold. Apply antifungal powder or spray to shoes and feet, particularly if you’re prone to sweating. Trim toenails straight across to avoid ingrown nails, which can create entry points for fungi. For athletes or those with active lifestyles, consider using foot deodorants and changing socks mid-day if necessary. Remember, fungi thrive in darkness and warmth, so airing out shoes and exposing feet to sunlight can help keep infections at bay.
When to Seek Professional Help: Red Flags and Remedies
While most fungal infections are manageable with home care, persistent or worsening symptoms warrant medical attention. Signs of a severe infection include intense itching, cracked skin, blisters, or a foul odor. If over-the-counter treatments fail after two weeks, consult a dermatologist. They may prescribe oral antifungal medications (e.g., terbinafine 250 mg daily for 6 weeks) or recommend a combination therapy. Ignoring symptoms can lead to complications like bacterial infections or nail fungus, which are harder to treat. Early intervention is key to restoring foot health and preventing recurrence.
Mushrooms on Rocks: Unveiling the Surprising Truth About Their Growth
You may want to see also

Symptoms of Foot Fungi
Foot fungi, often referred to as athlete’s foot (tinea pedis), is a common condition caused by dermatophytes, molds, or yeasts thriving in warm, moist environments. While mushrooms cannot grow on your feet, fungal infections can mimic their presence with symptoms like thickening, discoloration, and texture changes in the skin. Recognizing these signs early is crucial for effective treatment and prevention of spread.
Symptoms to Watch For: The first noticeable symptom is often itching, particularly between the toes, where fungi flourish due to trapped moisture. This may progress to burning or stinging sensations, especially after removing shoes. As the infection advances, the skin may peel, crack, or develop blisters, creating entry points for bacteria and secondary infections. In severe cases, toenails can become discolored, brittle, or thickened, resembling the texture of mushroom caps, though this is a separate condition called onychomycosis.
Comparative Analysis: Unlike mushrooms, which require soil and organic matter to grow, foot fungi feed on keratin in the skin and nails. However, both thrive in damp conditions, making sweaty socks, communal showers, and tight shoes prime breeding grounds. While mushrooms release spores into the air, foot fungi spread through direct contact with infected surfaces or skin scales, making hygiene and environmental cleanliness critical.
Practical Tips for Management: To alleviate symptoms, keep feet dry by changing socks daily and using antifungal powders. Over-the-counter treatments like clotrimazole or terbinafine creams are effective for mild cases, applied twice daily for 4–6 weeks. For persistent infections, consult a dermatologist for prescription-strength medications or oral antifungals. Prevent recurrence by wearing breathable footwear, avoiding walking barefoot in public areas, and disinfecting shoes regularly.
Takeaway: While mushrooms cannot grow on your feet, fungal infections can cause symptoms that may resemble their presence. Early detection and proper care are key to managing foot fungi effectively. By understanding the unique symptoms and taking proactive steps, you can maintain healthy feet and prevent complications.
Can Mushrooms Thrive on Rusted Metal Surfaces? Exploring Fungal Growth
You may want to see also

Prevention Tips for Athletes
Athletes, particularly those in endurance sports or training in humid environments, are prone to fungal infections like athlete’s foot, which thrives in damp, warm conditions. While mushrooms cannot grow on your feet, the same moisture-rich environments that fungi love can lead to persistent skin issues. Prevention hinges on disrupting fungal breeding grounds. After workouts, immediately remove sweaty socks and shoes, and thoroughly dry your feet, especially between toes. Carry a microfiber towel in your gym bag for this purpose—paper towels are less effective at absorbing moisture.
Footwear hygiene is non-negotiable. Alternate shoes daily to allow them to air out for at least 24 hours, reducing dampness where fungi flourish. Invest in moisture-wicking socks made of merino wool or synthetic blends, which pull sweat away from the skin faster than cotton. For shoes, choose breathable materials like mesh or leather, and consider using antifungal powder or spray inside them weekly. If you train in shared spaces like locker rooms, wear waterproof sandals to avoid contact with contaminated floors.
Proactive skin care can fortify your defenses. Apply a thin layer of antifungal cream (e.g., clotrimazole or miconazole) to clean, dry feet twice weekly, particularly during high-risk seasons like summer. For those with recurring issues, consult a dermatologist for prescription-strength solutions. Trim toenails straight across and file sharp edges to prevent ingrown nails, which can create pockets for fungal growth. Exfoliate feet weekly to remove dead skin cells, but avoid harsh scrubs that may cause micro-tears.
Environmental awareness is key. Avoid walking barefoot in communal areas, and disinfect gym equipment before use. If renting shoes (e.g., for rock climbing or bowling), wipe the interior with alcohol wipes beforehand. For athletes training in wet conditions, change into dry footwear immediately after exposure to water. Lastly, monitor your feet for early signs of infection—itching, redness, or peeling—and address them promptly. Prevention is less about eliminating risk and more about stacking small, consistent habits to outpace fungal threats.
Can Mushrooms Thrive in Water? Exploring Aquatic Fungal Growth
You may want to see also
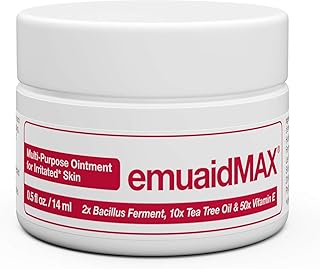
Explore related products

Treatment Options for Infections
While mushrooms themselves don't grow on feet, fungal infections like athlete's foot mimic the appearance of mushroom patches, thriving in warm, moist environments. Treatment hinges on eradicating the fungus, not cultivating a garden. Topical antifungal creams containing clotrimazole (1% strength, applied twice daily for 4-6 weeks) or terbinafine (1% strength, once daily for 1-2 weeks) are frontline defenses. For severe cases, oral medications like itraconazole (200mg daily for 1-2 weeks) or fluconazole (150mg once weekly for 2-4 weeks) may be prescribed, though these require monitoring for potential liver interactions.
Beyond pharmaceuticals, preventative measures are crucial. Keep feet dry by changing socks daily, opting for moisture-wicking materials like merino wool, and alternating shoes to allow them to fully dry between wears. Powdered antifungal agents like miconazole can be dusted inside shoes to inhibit fungal growth. For those prone to recurrent infections, a diluted vinegar soak (1 part vinegar to 2 parts water, 15-20 minutes daily) can help restore the skin’s pH, creating an inhospitable environment for fungi.
Natural remedies, while less studied, offer adjunctive options. Tea tree oil, diluted to 25-50% in a carrier oil, has demonstrated antifungal properties in some studies, though consistency varies. Garlic, rich in allicin, can be crushed and applied topically (cautiously, as it may irritate sensitive skin). However, these should complement, not replace, evidence-based treatments, especially in immunocompromised individuals or those with diabetes, where infections can escalate rapidly.
Finally, recognizing when to escalate care is critical. If symptoms persist beyond two weeks of treatment, spread to other areas, or are accompanied by signs of bacterial infection (pus, warmth, fever), consult a healthcare provider. Untreated fungal infections can lead to cellulitis or systemic complications, particularly in vulnerable populations. Treatment isn’t just about clearing the "mushroom-like" lesions—it’s about restoring foot health and preventing recurrence through a combination of targeted therapy and vigilant self-care.
Can Mushrooms Thrive in Cold Climates? Exploring Low-Temperature Growth
You may want to see also

Common Misconceptions About Fungi
Fungi are often misunderstood, and one of the most bizarre misconceptions is that mushrooms can grow on human feet. This idea likely stems from the damp, dark environments both fungi and feet often inhabit, but the reality is far less sensational. Mushrooms require specific conditions to grow, including a food source like decaying wood or soil, which human skin does not provide. While fungi like athlete’s foot (tinea pedis) thrive on feet, they are superficial infections, not mushroom-producing organisms. Understanding this distinction is crucial to dispel myths and address fungal concerns accurately.
Another common misconception is that all fungi are harmful. In truth, only a small fraction of fungal species cause disease in humans. For instance, *Candida albicans* can lead to yeast infections, but this is rare in healthy individuals with intact immune systems. Beneficial fungi, such as those used in fermentation (e.g., *Saccharomyces cerevisiae* for bread and beer), play vital roles in food production and ecosystems. Even mushrooms, often feared as toxic, are largely safe when properly identified—edible varieties like button, shiitake, and oyster mushrooms are nutritional powerhouses. The key is education: learning to differentiate between harmful and helpful fungi can transform fear into appreciation.
A pervasive myth is that antifungal treatments are universally effective. In reality, efficacy depends on the type of fungus and the product used. Topical creams like clotrimazole work well for skin infections, but oral medications such as fluconazole are needed for systemic issues like thrush. Dosage and duration matter too—for example, athlete’s foot treatment typically requires 2–6 weeks of consistent application. Overuse of antifungals can lead to resistance, similar to antibiotics, so it’s essential to follow guidelines. For stubborn cases, consult a healthcare provider to ensure the right treatment is used.
Finally, many believe fungi only thrive in dirty environments, but cleanliness alone isn’t a guarantee against fungal growth. Fungi are opportunistic and can colonize even well-maintained spaces if conditions are right—warmth, moisture, and organic material. Gym showers, for instance, are hotspots for fungal spores despite regular cleaning. Practical tips include keeping feet dry, wearing breathable footwear, and avoiding walking barefoot in public areas. By focusing on environmental factors rather than just hygiene, individuals can reduce their risk of fungal infections more effectively.
Can Mushrooms Thrive in Potting Soil? A Complete Guide
You may want to see also
Frequently asked questions
No, mushrooms cannot grow on your feet. Mushrooms require specific conditions like soil, organic matter, and moisture to grow, which are not present on human skin.
The misconception likely stems from fungal infections like athlete’s foot, which can cause symptoms such as itching, peeling, and discoloration, resembling mold or fungus. However, these are not mushrooms but rather dermatophytes (fungal organisms).
To prevent fungal infections, keep your feet clean and dry, wear breathable footwear, change socks regularly, avoid walking barefoot in public areas, and use antifungal powders or sprays if needed.