The question of whether mushrooms can cause depression is a complex and multifaceted one, rooted in both scientific research and cultural perceptions. While certain types of mushrooms, such as psilocybin-containing magic mushrooms, have been studied for their potential therapeutic effects on mental health, including depression, others may pose risks. Psilocybin has shown promise in clinical trials for treating treatment-resistant depression, but its use is highly controlled and requires professional guidance. Conversely, some mushrooms, particularly those that are toxic or misidentified, can lead to physical and psychological distress, potentially exacerbating depressive symptoms. Additionally, individual reactions to mushrooms vary widely, influenced by factors like dosage, setting, and personal mental health history. As interest in both medicinal and recreational mushroom use grows, understanding their effects on mental health remains crucial for informed decision-making.
| Characteristics | Values |
|---|---|
| Psilocybin Mushrooms | Some studies suggest psilocybin (found in certain mushrooms) can temporarily induce anxiety, paranoia, or mood disturbances in susceptible individuals, but it is not directly linked to long-term depression. |
| Individual Sensitivity | Effects vary widely based on genetics, mental health history, dosage, and setting. Those with predispositions to mental health issues may experience worsened symptoms. |
| Short-Term Effects | Can cause emotional distress, confusion, or fear during the "trip," which may mimic or exacerbate depressive feelings temporarily. |
| Long-Term Effects | Research indicates psilocybin, when used in controlled settings, may reduce depression and anxiety in some cases, but recreational use without supervision carries risks. |
| Non-Psilocybin Mushrooms | Most edible mushrooms (e.g., button, shiitake) have no known link to depression. Poisonous mushrooms can cause severe health issues but not directly related to depression. |
| Psychological Factors | Negative experiences or trauma associated with mushroom use can contribute to depressive symptoms. |
| Medical Context | Psilocybin is being studied as a potential treatment for depression, with some trials showing promise in reducing symptoms when administered therapeutically. |
| Recreational Use Risks | Unsupervised use increases the likelihood of adverse psychological reactions, including temporary depressive episodes. |
| Cultural and Legal Factors | Stigma or legal consequences related to mushroom use may indirectly contribute to stress or depressive feelings in some individuals. |
| Conclusion | Mushrooms themselves do not directly cause depression, but psilocybin mushrooms can trigger or worsen mood disturbances in vulnerable individuals. Context and setting play a critical role. |
Explore related products
What You'll Learn
- Psilocybin's Impact on Mood: Research shows psilocybin can cause temporary depression-like symptoms in some users
- Toxic Mushroom Effects: Certain toxic mushrooms may induce neurological symptoms, including mood disturbances and depression
- Individual Sensitivity: Genetic and psychological factors influence how mushrooms affect mental health, including depression risk
- Long-Term Psychological Effects: Repeated use of psychedelic mushrooms may lead to persistent depressive symptoms in some individuals
- Nutritional Deficiencies: Overconsumption of mushrooms with low nutritional value could indirectly contribute to depressive symptoms

Psilocybin's Impact on Mood: Research shows psilocybin can cause temporary depression-like symptoms in some users
Psilocybin, the psychoactive compound found in certain mushrooms, has been hailed for its potential to alleviate depression and anxiety. Yet, paradoxically, research indicates that it can also induce temporary depression-like symptoms in some users. This duality underscores the complexity of psilocybin’s effects on the brain, which are influenced by factors like dosage, set, and setting. Studies often administer doses ranging from 10 to 30 milligrams, with higher amounts more likely to provoke intense emotional responses, including feelings of sadness or hopelessness. These effects are typically short-lived, lasting hours rather than days, but they highlight the importance of supervised use in clinical settings.
Consider the mechanism at play: psilocybin binds to serotonin receptors in the brain, altering neural pathways and potentially amplifying latent emotional states. For individuals predisposed to depression or anxiety, this amplification can manifest as transient depressive symptoms. A 2021 study published in *JAMA Psychiatry* found that while many participants experienced significant mood improvements after psilocybin therapy, a subset reported acute distress during sessions. This variability suggests that psilocybin is not a one-size-fits-all solution and requires careful screening and monitoring.
Practical tips for minimizing risks include starting with a low dose (e.g., 10–15 milligrams) and ensuring a supportive environment. Users should avoid psilocybin if they have a personal or family history of mental health disorders, as this increases the likelihood of adverse reactions. Additionally, integrating therapy before and after sessions can help process any difficult emotions that arise. For instance, preparatory sessions can establish coping strategies, while follow-up discussions can contextualize and reframe challenging experiences.
Comparatively, the temporary depression-like symptoms induced by psilocybin differ from chronic depression in their duration and context. Unlike clinical depression, which persists over weeks or months, psilocybin-induced symptoms are acute and often part of a broader therapeutic process. This distinction is crucial for users and practitioners alike, as it frames these experiences not as failures but as potential steps toward healing. However, it also emphasizes the need for caution, particularly in recreational settings where control over dosage and environment is limited.
In conclusion, while psilocybin holds promise as a treatment for mood disorders, its ability to cause temporary depression-like symptoms in some users cannot be overlooked. Understanding this risk allows for better preparation and management, ensuring that the benefits of psilocybin are maximized while minimizing potential harm. As research progresses, tailored approaches that account for individual differences will be key to harnessing its therapeutic potential safely.
Mushroom Cultivation on Half Slabs: Exploring Unique Growing Surfaces
You may want to see also

Toxic Mushroom Effects: Certain toxic mushrooms may induce neurological symptoms, including mood disturbances and depression
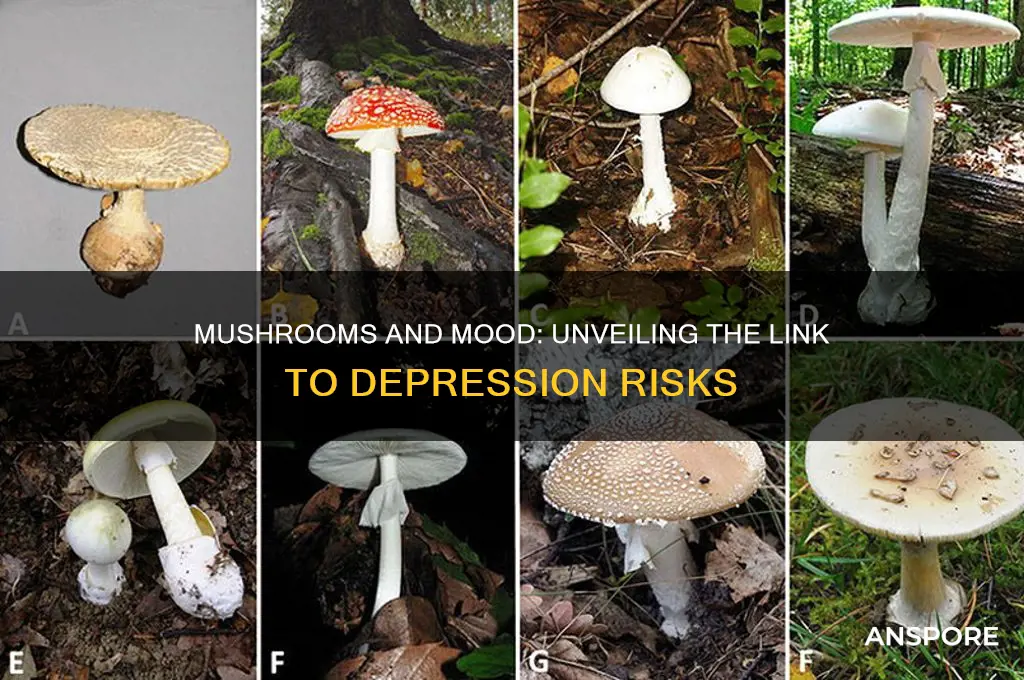
Toxic mushrooms, often lurking in forests and gardens, can wreak havoc on the human body, particularly the nervous system. Among their sinister effects, certain species are known to induce neurological symptoms that extend beyond physical discomfort. Mood disturbances, including depression, have been reported in individuals who inadvertently ingest these fungi. For instance, the Amanita muscaria, commonly known as the fly agaric, contains compounds like muscimol and ibotenic acid, which can alter brain chemistry and lead to emotional instability. Similarly, the Amanita pantherina, or panther cap, has been linked to severe psychological effects, including profound sadness and anxiety. These cases underscore the importance of accurately identifying mushrooms before consumption, as even small doses of toxic species can trigger significant mental health issues.
Understanding the mechanisms behind these effects is crucial for prevention and treatment. Toxic mushrooms often contain psychoactive compounds that interfere with neurotransmitters like serotonin and dopamine, which play pivotal roles in regulating mood. For example, the toxin amatoxin, found in the deadly Amanita phalloides (death cap), can cause liver failure, but its early symptoms include confusion, agitation, and depression. These neurological manifestations are not merely side effects but direct consequences of the toxins disrupting neural pathways. Individuals, especially foragers and enthusiasts, should be aware that even a single bite of a toxic mushroom can lead to long-lasting psychological distress. Educating oneself about mushroom identification and seeking expert advice when uncertain can be life-saving measures.
A comparative analysis of toxic mushroom species reveals varying degrees of risk. While some, like the Psilocybe genus, are known for their hallucinogenic properties and are sometimes used recreationally, others, such as the Galerina marginata (deadly galerina), are outright dangerous. The latter contains amatoxins similar to the death cap and can cause severe depression alongside other symptoms. Interestingly, the onset of mood disturbances can vary depending on the species and dosage. For instance, symptoms from Amanita muscaria may appear within 30 minutes to 2 hours, while those from amatoxin-containing mushrooms can take 6 to 24 hours to manifest. This delayed onset often leads to misdiagnosis, making it critical to disclose any recent mushroom consumption to healthcare providers.
Practical tips for avoiding toxic mushroom-induced depression are straightforward yet essential. First, never consume wild mushrooms unless positively identified by an expert. Second, be cautious of mushrooms growing near poisonous plants or in contaminated areas, as they may absorb harmful substances. Third, if accidental ingestion occurs, seek medical attention immediately, even if symptoms seem mild. Activated charcoal may be administered in some cases to reduce toxin absorption, but this should only be done under professional guidance. Lastly, educate children about the dangers of wild mushrooms, as their curiosity can lead to accidental poisoning. By taking these precautions, individuals can enjoy the beauty of fungi without falling victim to their darker side.
Mushrooms and Hair Loss: Unraveling the Surprising Connection
You may want to see also

Individual Sensitivity: Genetic and psychological factors influence how mushrooms affect mental health, including depression risk
Not everyone reacts to mushrooms in the same way, and this variability is a critical factor when discussing their potential link to depression. Individual sensitivity plays a pivotal role, shaped by a complex interplay of genetic and psychological elements. For instance, certain genetic variations can influence how the body metabolizes psilocybin, the active compound in many mushrooms, leading to differing mental health outcomes. A person with a family history of mental health disorders might experience heightened anxiety or depressive symptoms after consumption, while another individual with no such history could have a neutral or even positive reaction. This genetic predisposition underscores the importance of understanding one’s family medical history before experimenting with mushrooms.
Psychological factors further complicate this landscape. Stress levels, pre-existing mental health conditions, and even personality traits can amplify or mitigate the effects of mushrooms. For example, individuals with high neuroticism scores on personality tests may be more susceptible to negative psychological experiences, including depressive episodes, after ingesting mushrooms. Conversely, those with a resilient mindset or strong emotional support system might navigate these experiences with fewer adverse effects. A study published in *JAMA Psychiatry* highlighted that individuals with a history of depression or anxiety were more likely to report worsened symptoms after psilocybin use, emphasizing the need for caution in vulnerable populations.
Dosage and context are equally important in this equation. Microdosing, typically involving 0.1 to 0.3 grams of dried psilocybin mushrooms, is often touted for its potential cognitive and mood benefits. However, even at these low doses, individuals with heightened sensitivity may experience unintended consequences, such as mood swings or increased rumination. Full doses (1 to 3 grams) in uncontrolled settings can lead to intense emotional experiences, which, for some, may trigger or exacerbate depressive symptoms. Practical advice includes starting with the lowest possible dose and maintaining a stable, supportive environment during use.
To mitigate risks, individuals should consider a few key steps. First, consult a healthcare professional, especially if there is a history of mental health issues. Second, avoid self-medicating with mushrooms without proper guidance, as this can lead to unpredictable outcomes. Third, monitor your mental state closely in the days following consumption, noting any changes in mood or behavior. For those under 25, whose brains are still developing, the risks may be higher, and caution is particularly advised.
In conclusion, while mushrooms can offer therapeutic potential for some, their impact on mental health is far from universal. Genetic and psychological factors create a spectrum of responses, making personalized awareness and caution essential. Understanding these nuances can help individuals make informed decisions, ensuring that the exploration of mushrooms does not inadvertently contribute to depression or other mental health challenges.
Exploring Mushrooms' Potential Role in Schizophrenia Treatment and Management
You may want to see also
Explore related products

Long-Term Psychological Effects: Repeated use of psychedelic mushrooms may lead to persistent depressive symptoms in some individuals
Psychedelic mushrooms, often hailed for their potential therapeutic benefits, carry a less-discussed risk: repeated use may trigger persistent depressive symptoms in some individuals. This phenomenon, though not universal, warrants careful consideration, especially as interest in psychedelics grows. Research suggests that frequent exposure to psilocybin, the active compound in these mushrooms, can disrupt serotonin regulation in the brain. Serotonin, a neurotransmitter linked to mood, may become dysregulated over time, leading to prolonged feelings of sadness or anhedonia. For instance, a 2021 study published in *JAMA Psychiatry* found that individuals with a history of heavy psychedelic use were more likely to report depressive episodes lasting weeks or months after cessation.
Understanding the dosage and frequency of use is critical in assessing risk. Recreational users often consume between 1 to 5 grams of dried mushrooms per session, with effects lasting 4 to 6 hours. However, repeated use—defined as weekly or daily consumption—amplifies the potential for long-term psychological effects. Younger users, particularly those under 25, are more vulnerable due to ongoing brain development. For example, a longitudinal study from the *Journal of Psychopharmacology* noted that adolescents who used psychedelics regularly were twice as likely to develop depressive symptoms by age 30 compared to non-users. These findings underscore the importance of age and dosage as key factors in risk assessment.
To mitigate risks, individuals should adopt harm-reduction strategies. First, limit psychedelic mushroom use to occasional, intentional experiences rather than habitual consumption. Second, maintain a detailed journal to track dosage, frequency, and emotional responses, which can help identify early signs of mood changes. Third, integrate experiences with therapy or guided sessions to process emotions constructively. For those already experiencing depressive symptoms, discontinuing use and seeking professional help is essential. Therapists specializing in substance-induced mood disorders can provide tailored interventions, such as cognitive-behavioral therapy or medication management.
Comparing psychedelic mushrooms to other substances highlights their unique risks. Unlike stimulants or opioids, psychedelics primarily affect mood and perception rather than physical dependence. However, their psychological impact can be more insidious, often going unnoticed until symptoms become severe. For instance, while alcohol’s depressive effects are immediate and dose-dependent, psilocybin’s mood alterations may emerge weeks or months after use. This delayed onset complicates diagnosis and treatment, emphasizing the need for proactive monitoring.
In conclusion, while psychedelic mushrooms hold promise for mental health treatment, their long-term psychological effects cannot be ignored. Repeated use, especially in high doses or among younger individuals, may lead to persistent depressive symptoms. By understanding the risks, adopting harm-reduction practices, and seeking timely intervention, users can navigate these substances more safely. As research evolves, a balanced perspective—acknowledging both benefits and risks—remains crucial for informed decision-making.
Mushrooms and Mental Health: Exploring the Link to Psychosis
You may want to see also

Nutritional Deficiencies: Overconsumption of mushrooms with low nutritional value could indirectly contribute to depressive symptoms
While mushrooms are celebrated for their umami flavor and versatility in cooking, not all varieties offer substantial nutritional benefits. Overconsuming mushrooms with low nutritional value can inadvertently lead to dietary imbalances, potentially exacerbating or contributing to depressive symptoms. This occurs when these mushrooms displace more nutrient-dense foods in your diet, creating deficiencies in vitamins and minerals critical for mental health.
Consider the common button mushroom, a staple in many kitchens. While it contains some B vitamins and antioxidants, its nutritional profile pales in comparison to leafy greens, nuts, or lean proteins. If a significant portion of your daily vegetable intake consists of button mushrooms, you may be missing out on essential nutrients like magnesium, zinc, and omega-3 fatty acids—all of which play a role in mood regulation. For instance, magnesium deficiency has been linked to increased anxiety and depression, while low zinc levels can impair neurotransmitter function.
The risk is particularly pronounced in individuals following restrictive diets or those who rely heavily on mushrooms as a primary vegetable source. A 2020 study published in the *Journal of Affective Disorders* found that dietary patterns lacking in essential nutrients were associated with a higher prevalence of depressive symptoms, especially in younger adults aged 18–30. To mitigate this, aim to diversify your diet by pairing mushrooms with nutrient-rich foods like spinach, quinoa, or fatty fish. For example, instead of a mushroom-only stir-fry, add bell peppers, broccoli, and tofu to ensure a broader spectrum of vitamins and minerals.
Practical steps can help balance mushroom consumption. First, prioritize nutrient-dense mushroom varieties like shiitake or maitake, which contain higher levels of B vitamins and antioxidants. Second, limit daily mushroom intake to 1–2 servings (approximately 1 cup cooked) to avoid over-reliance. Finally, consult a dietitian if you suspect nutritional deficiencies, especially if you experience persistent fatigue, mood swings, or other depressive symptoms. By being mindful of mushroom consumption and its nutritional context, you can enjoy their culinary benefits without compromising mental well-being.
Preserving Mushrooms in Alcohol: A Year-Long Storage Solution?
You may want to see also
Frequently asked questions
There is no scientific evidence to suggest that consuming common edible mushrooms causes depression. However, certain wild mushrooms contain toxins that can lead to severe health issues, including psychological symptoms, if ingested.
Some psychoactive mushrooms, like those containing psilocybin, can induce intense emotional experiences. While they are being studied for potential therapeutic use in depression, they can also trigger anxiety or worsen symptoms in susceptible individuals if used improperly.
Allergic reactions to mushrooms can cause physical discomfort, but there is no direct link between mushroom allergies and depression. However, chronic health issues or discomfort may indirectly affect mood and mental health.
Some medicinal mushrooms, such as reishi and lion's mane, are being studied for their potential to support mental health. While they may have adaptogenic properties, there is insufficient evidence to confirm they directly treat or prevent depression. Always consult a healthcare provider before use.