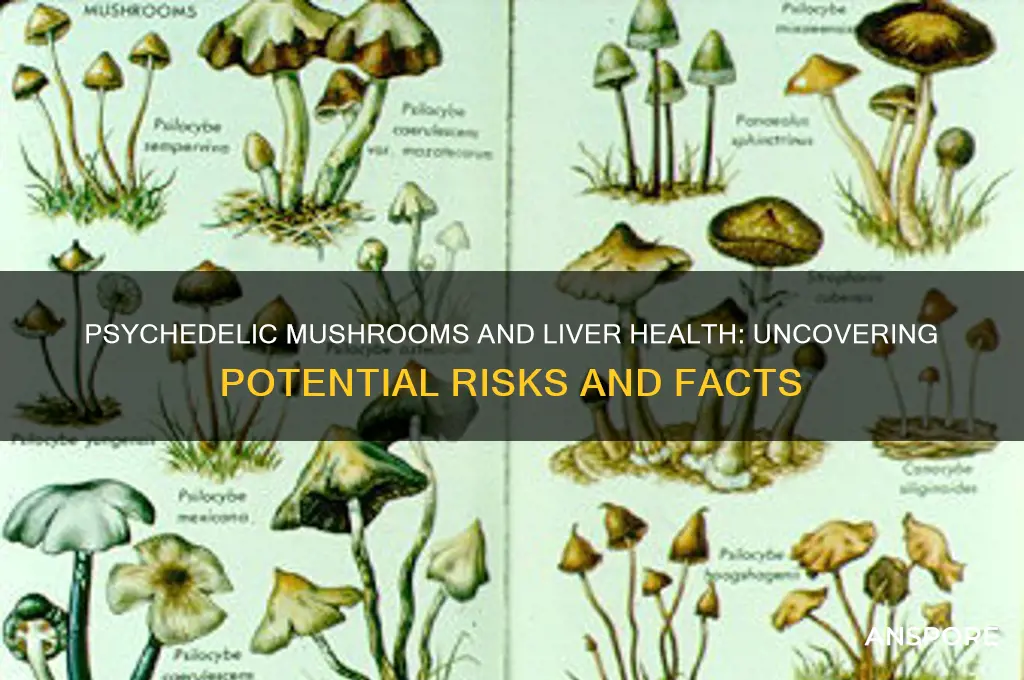
Psychedelic mushrooms, commonly known as magic mushrooms, contain psychoactive compounds like psilocybin, which have gained attention for their potential therapeutic benefits in treating mental health conditions such as depression and anxiety. However, concerns have arisen regarding their safety, particularly their impact on liver health. While psilocybin itself is not typically associated with liver toxicity, the mushrooms may contain other naturally occurring compounds or contaminants that could pose risks. Additionally, the method of consumption, such as ingestion of improperly prepared or misidentified mushrooms, can lead to adverse effects, including potential liver damage. Research on this topic remains limited, and further studies are needed to fully understand the relationship between psychedelic mushrooms and liver health.
| Characteristics | Values |
|---|---|
| Common Psychedelic Mushrooms | Psilocybin-containing mushrooms (e.g., Psilocybe cubensis) |
| Primary Active Compound | Psilocybin, which converts to psilocin in the body |
| Known Liver Toxicity | No direct evidence of liver damage from psilocybin mushrooms |
| Metabolism | Primarily metabolized by the liver (CYP enzymes) |
| Reported Cases of Liver Damage | Extremely rare; no conclusive evidence linking psilocybin to liver harm |
| Potential Risks | Contamination with toxic fungi (e.g., Amanita species) can cause liver damage |
| Comparison to Other Substances | Lower hepatotoxicity compared to alcohol, acetaminophen, or toxic mushrooms |
| Medical Research | Studies focus on psilocybin's therapeutic effects, not liver toxicity |
| User Precautions | Avoid misidentification of mushrooms; ensure proper sourcing |
| Conclusion | Psychedelic mushrooms themselves are not known to cause liver damage |
Explore related products
What You'll Learn

Psilocybin metabolism in the liver
Psilocybin, the primary psychoactive compound in psychedelic mushrooms, undergoes significant transformation in the liver, a process critical to its effects and potential risks. Once ingested, psilocybin is rapidly dephosphorylated into psilocin, its active metabolite, primarily by the enzyme alkaline phosphatase. This conversion is essential for psilocin to cross the blood-brain barrier and induce psychedelic experiences. However, the liver’s role doesn’t end there; it also metabolizes psilocin via phase II conjugation, attaching glucuronic acid to create psilocin glucuronide, a water-soluble compound easily excreted in urine. This dual metabolic pathway highlights the liver’s central role in both activating and deactivating psilocybin.
While the liver efficiently processes psilocybin, concerns about liver damage arise from anecdotal reports and limited studies. High doses or frequent use may overwhelm the liver’s metabolic capacity, potentially leading to transient elevations in liver enzymes. For instance, a case study published in *Journal of Medical Toxicology* documented mild hepatotoxicity in a user who consumed a large quantity of psychedelic mushrooms. However, such cases are rare and typically resolve without long-term consequences. It’s crucial to note that psilocybin itself is not inherently hepatotoxic; rather, excessive intake or pre-existing liver conditions may exacerbate stress on the organ.
To minimize liver-related risks, users should adhere to safe dosing practices. A typical recreational dose ranges from 1 to 3 grams of dried mushrooms, containing approximately 10–30 mg of psilocybin. Exceeding this range increases metabolic burden on the liver and the likelihood of adverse effects. Individuals with liver disease or those taking medications metabolized by the liver (e.g., antidepressants, antipsychotics) should exercise caution, as psilocybin may interact unpredictably with these substances. Consulting a healthcare provider before use is advisable for these populations.
Comparatively, psilocybin’s liver impact pales in contrast to that of substances like alcohol or acetaminophen, which are well-documented hepatotoxins. Unlike these compounds, psilocybin does not cause direct liver cell death or fibrosis. However, its metabolism still warrants respect, particularly in the context of polydrug use. Combining psilocybin with other hepatically metabolized substances, such as alcohol or cannabis, can amplify liver stress. Users should prioritize moderation and avoid mixing substances to reduce cumulative strain on the liver.
In conclusion, while psilocybin metabolism in the liver is generally safe, mindful use is essential to prevent potential harm. Understanding the liver’s role in processing psilocybin empowers users to make informed decisions. By respecting dosage guidelines, considering individual health status, and avoiding harmful combinations, individuals can minimize liver-related risks while exploring the therapeutic or recreational benefits of psychedelic mushrooms.
Mushrooms and Anxiety: Exploring Nature's Potential for Calming Relief
You may want to see also

Potential hepatotoxic effects of mushrooms
Psychedelic mushrooms, primarily known for their psychoactive compounds like psilocybin, are often consumed for their mind-altering effects. However, their potential impact on liver health remains a critical yet under-discussed concern. While psilocybin itself is not typically associated with hepatotoxicity, the presence of secondary compounds or contaminants in wild mushrooms can pose risks. For instance, certain species of mushrooms, such as *Amanita phalloides* (the death cap), contain amatoxins that directly target liver cells, leading to severe damage or failure. Even misidentified psychedelic mushrooms can inadvertently expose users to these toxic substances, highlighting the importance of accurate identification and sourcing.
Analyzing the hepatotoxic potential of psychedelic mushrooms requires distinguishing between intentional use and accidental exposure. Psilocybin mushrooms, when properly identified and consumed in controlled doses (typically 1–3 grams of dried material), are generally considered safe for the liver. However, the liver’s role in metabolizing psilocybin into psilocin means it undergoes increased activity during ingestion. While this process is not inherently harmful, individuals with pre-existing liver conditions, such as hepatitis or cirrhosis, may experience exacerbated stress on their liver function. Additionally, combining psychedelic mushrooms with alcohol or other hepatotoxic substances can compound the risk, as the liver must process multiple toxins simultaneously.
To minimize potential hepatotoxic effects, users should adopt specific precautions. First, ensure mushrooms are sourced from reputable suppliers or foraged by experienced individuals to avoid toxic species. Second, start with low doses (e.g., 1 gram for beginners) to gauge tolerance and reduce metabolic strain. Third, avoid concurrent use of alcohol, acetaminophen, or other liver-stressing substances for at least 24 hours before and after consumption. For those with liver concerns, consulting a healthcare provider before use is essential. Lastly, monitor for symptoms of liver distress, such as jaundice, abdominal pain, or unexplained fatigue, and seek medical attention if they occur.
Comparatively, the hepatotoxic risks of psychedelic mushrooms pale in comparison to those of synthetic drugs or chronic alcohol use. However, their natural origin does not render them risk-free. Unlike pharmaceutical substances, psychedelic mushrooms lack standardized dosing and purity, making their effects less predictable. This variability underscores the need for informed, cautious use. While research on psilocybin’s long-term effects on liver health remains limited, anecdotal evidence and case studies suggest that responsible use minimizes risks. By prioritizing safety and awareness, individuals can enjoy the benefits of psychedelic mushrooms while safeguarding their liver health.
Prepping Port Wine and Mushroom Sauce: Make-Ahead Tips for Busy Cooks
You may want to see also

Liver enzyme changes post-consumption
Psychedelic mushrooms, particularly those containing psilocybin, have been associated with transient changes in liver enzyme levels post-consumption. These changes are typically mild and resolve within a few days, but understanding their implications is crucial for both users and healthcare providers. Liver enzymes such as alanine transaminase (ALT) and aspartate transaminase (AST) are markers of liver health, and elevations in these enzymes can indicate liver stress or damage. Studies have shown that psilocybin mushrooms can cause a temporary increase in these enzymes, often within 24–48 hours after ingestion, though the exact mechanisms remain under investigation.
Analyzing the data, it’s clear that dosage plays a significant role in the extent of liver enzyme changes. Low to moderate doses (1–2 grams of dried mushrooms) are less likely to cause notable elevations, while higher doses (3 grams or more) have been linked to more pronounced enzyme fluctuations. Age and pre-existing liver conditions also influence susceptibility; younger, healthier individuals may experience minimal changes, whereas older adults or those with liver disease could face greater risks. For instance, a 2021 study published in *Journal of Psychopharmacology* noted that participants over 50 years old showed higher ALT levels post-consumption compared to their younger counterparts.
To mitigate potential risks, individuals considering psychedelic mushroom use should follow practical precautions. First, start with a low dose to gauge tolerance and minimize liver stress. Second, avoid mixing mushrooms with alcohol or other hepatotoxic substances, as this can exacerbate enzyme elevations. Third, monitor liver health through blood tests before and after use, especially if repeated consumption is planned. Healthcare providers should be informed of mushroom use to interpret enzyme changes accurately and rule out other causes of liver dysfunction.
Comparatively, the liver enzyme changes caused by psychedelic mushrooms are generally less severe than those associated with chronic alcohol use or acetaminophen overdose. However, the transient nature of these changes does not negate the need for caution. For example, while a single moderate dose may cause a mild, temporary increase in ALT, repeated high-dose use could lead to cumulative liver stress. This underscores the importance of responsible use and awareness of individual health status.
In conclusion, while psychedelic mushrooms can cause temporary liver enzyme changes, these are typically mild and reversible. By understanding the factors influencing these changes—such as dosage, age, and pre-existing conditions—users can take proactive steps to minimize risks. Practical measures like dose moderation, avoiding hepatotoxic combinations, and monitoring liver health can help ensure safer experiences. As research continues to explore the relationship between psilocybin and liver function, informed and cautious use remains the best approach.
Mushrooms and Neurogenesis: Can Fungi Stimulate Brain Cell Growth?
You may want to see also
Explore related products

Risk factors for liver damage
Psychedelic mushrooms, often referred to as magic mushrooms, contain psilocybin, a compound known for its hallucinogenic effects. While research on their direct impact on the liver is limited, understanding the risk factors for liver damage is crucial for anyone considering their use. The liver, a vital organ responsible for detoxifying the body, can be compromised by various factors, and psychedelic mushrooms may interact with these in unpredictable ways.
Dosage and Frequency: The Double-Edged Sword
One of the primary risk factors for liver damage is the dosage and frequency of psychedelic mushroom consumption. Psilocybin itself is not typically hepatotoxic, but high doses or frequent use can strain the liver’s metabolic processes. For instance, a single dose of 1–2 grams of dried mushrooms is commonly considered moderate, but exceeding 5 grams can overwhelm the liver’s ability to process toxins efficiently. Chronic users, especially those consuming mushrooms weekly, may inadvertently increase their risk of liver stress or damage over time. To mitigate this, limit consumption to occasional use and adhere to low to moderate doses, ensuring at least a week between sessions.
Polysubstance Use: A Dangerous Cocktail
Combining psychedelic mushrooms with other substances significantly elevates the risk of liver damage. Alcohol, for example, is a known hepatotoxin, and its simultaneous use with psilocybin can exacerbate liver strain. Similarly, mixing mushrooms with prescription medications, such as acetaminophen (Tylenol), can lead to acute liver injury. Even seemingly harmless substances like caffeine or nicotine can contribute to liver stress when combined with psychedelics. If you must use mushrooms, avoid polysubstance use and consult a healthcare provider if you’re on medication to assess potential interactions.
Individual Health Factors: The Silent Contributors
Pre-existing health conditions play a critical role in determining liver damage risk. Individuals with underlying liver diseases, such as hepatitis or fatty liver, are more susceptible to harm from any hepatotoxic substance, including potential stressors like psilocybin. Age is another factor; older adults (50+) may have reduced liver function, making them more vulnerable. Additionally, genetic predispositions or metabolic disorders can influence how the liver processes toxins. If you fall into any of these categories, it’s advisable to avoid psychedelic mushrooms altogether or proceed with extreme caution under medical supervision.
Contaminants and Misidentification: Hidden Dangers
The risk of liver damage isn’t always tied to psilocybin itself but can stem from contaminants or misidentified mushrooms. Wild mushrooms often harbor toxins like amatoxins, found in species like the Death Cap (*Amanita phalloides*), which cause severe liver damage and can be fatal. Even cultivated mushrooms can be contaminated with pesticides or mold if not sourced responsibly. Always obtain mushrooms from a trusted, verified source, and consider using a test kit to confirm their identity. Foraging without expertise is a gamble that could cost more than a bad trip.
Practical Tips for Minimizing Risk
To protect your liver while using psychedelic mushrooms, follow these actionable steps:
- Start Low, Go Slow: Begin with a small dose (1 gram or less) and gradually increase if needed.
- Stay Hydrated: Proper hydration supports liver function during and after use.
- Avoid Alcohol: Refrain from drinking alcohol for at least 24 hours before and after consumption.
- Monitor Health: If you experience symptoms like abdominal pain, jaundice, or fatigue after use, seek medical attention immediately.
- Know Your Source: Only consume mushrooms from reputable suppliers or grow them under sterile conditions.
While psychedelic mushrooms are not inherently liver-toxic, their misuse or interaction with other factors can pose risks. By understanding and addressing these risk factors, users can minimize potential harm and prioritize liver health.
Can Probation Officers Test for Psilocybin Mushrooms? Legal Insights
You may want to see also

Comparing mushroom toxicity to other substances
Psychedelic mushrooms, often referred to as "magic mushrooms," contain psilocybin, a compound known for its hallucinogenic effects. While their impact on the liver is a concern, it’s crucial to compare their toxicity to other substances to provide context. For instance, psilocybin mushrooms are generally considered less toxic than many common substances, including alcohol and acetaminophen, which are known to cause significant liver damage when consumed in excess. A single dose of psilocybin mushrooms typically ranges from 1 to 3 grams of dried material, and at these levels, liver toxicity is extremely rare. In contrast, chronic alcohol consumption or even a single high dose of acetaminophen (above 4 grams in 24 hours) can lead to severe liver injury or failure.
To illustrate, let’s compare the liver toxicity of psychedelic mushrooms to that of Amanita phalloides, a highly poisonous mushroom species. While psilocybin mushrooms are psychoactive but not inherently toxic to the liver, Amanita phalloides contains amatoxins, which can cause acute liver failure within 24 to 48 hours of ingestion. This stark difference highlights the importance of proper identification when foraging mushrooms. For those experimenting with psychedelics, purchasing from reputable sources or using testing kits can mitigate risks associated with misidentification.
From a comparative standpoint, the liver toxicity of psychedelic mushrooms pales in comparison to that of synthetic drugs like MDMA or cocaine. MDMA, for example, can cause hyperthermia and hepatotoxicity, particularly when used in high doses (over 1.5 mg per kilogram of body weight) or in hot environments. Cocaine, on the other hand, can lead to ischemic hepatitis due to its vasoconstrictive effects. Unlike these substances, psilocybin mushrooms do not typically cause direct liver damage, even in moderate doses. However, individuals with pre-existing liver conditions should exercise caution, as any additional stress on the liver could exacerbate their condition.
A persuasive argument for the relative safety of psychedelic mushrooms lies in their historical and cultural use. Indigenous communities have consumed these mushrooms for centuries without widespread reports of liver damage. Modern research supports this, with studies showing that psilocybin has a low potential for toxicity compared to other recreational substances. For example, the LD50 (lethal dose for 50% of subjects) of psilocybin in rats is approximately 280 mg/kg, a dose far higher than what humans typically consume. In contrast, the LD50 of alcohol is around 150 mg/kg in rats, making it significantly more toxic in high doses.
In practical terms, individuals concerned about liver health should prioritize avoiding substances with known hepatotoxicity, such as excessive alcohol, acetaminophen, and certain prescription medications. For those interested in psychedelic experiences, starting with a low dose of psilocybin mushrooms (e.g., 1 gram) and ensuring proper hydration can further minimize risks. While no substance is entirely without risk, the evidence suggests that psychedelic mushrooms pose a lower threat to liver health compared to many other commonly used drugs. Always consult a healthcare professional if you have specific concerns or pre-existing conditions.
Freezing Psychedelic Mushrooms: Preservation Tips and Potential Risks Explained
You may want to see also
Frequently asked questions
Psychedelic mushrooms, such as those containing psilocybin, are not typically associated with direct liver damage when consumed in moderate amounts. However, contaminants or misidentified mushrooms (e.g., poisonous species like Amanita) can cause severe liver toxicity.
Long-term studies on psychedelic mushrooms and liver health are limited, but there is no strong evidence to suggest they cause chronic liver damage. However, frequent use of any substance can strain the liver indirectly, especially if combined with alcohol or other hepatotoxic substances.
Psychedelic mushrooms may interact with medications metabolized by the liver, potentially increasing the risk of liver damage. For example, combining them with acetaminophen or certain antidepressants could exacerbate liver stress. Always consult a healthcare provider if using medications.