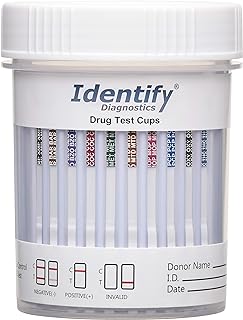
The question of whether drug tests can detect psychedelic mushrooms, which contain the psychoactive compound psilocybin, is a topic of growing interest as these substances gain attention for their potential therapeutic benefits and increasing decriminalization efforts. Standard drug tests, such as those used in workplaces or legal settings, typically screen for common substances like cannabis, opioids, cocaine, and amphetamines, but they do not usually detect psilocybin or its metabolite, psilocin. Specialized tests can identify these compounds, but they are not routinely administered due to cost and limited demand. However, as research and public interest in psychedelics expand, the availability and use of such tests may increase, raising questions about privacy, legality, and the implications for individuals using these substances for medicinal or recreational purposes.
| Characteristics | Values |
|---|---|
| Detectable Substance | Psilocybin and psilocin (primary active compounds in psychedelic mushrooms) |
| Standard Drug Tests | Typically not detected in standard 5-panel or 10-panel drug tests (e.g., urine, saliva, blood, hair) |
| Specialized Testing | Detectable in urine and blood for up to 24 hours after ingestion with specific psilocybin/psilocin tests |
| Hair Testing | Can be detected in hair follicles for up to 90 days with specialized testing |
| Detection Window | Urine: 24 hours; Blood: 24 hours; Hair: Up to 90 days |
| False Positives | Unlikely, as psilocybin/psilocin tests are highly specific |
| Legal Status | Psilocybin is a Schedule I controlled substance in the U.S., but testing is rare unless specifically targeted |
| Common Use of Testing | Rarely used in routine drug screenings; more common in forensic, research, or specialized medical settings |
| Metabolism | Psilocybin is rapidly metabolized into psilocin, which is then broken down and excreted quickly |
| Availability of Tests | Specialized tests are available but not widely used due to cost and limited demand |
Explore related products
What You'll Learn
- Detection methods: Urine, blood, hair tests for psilocybin metabolites, detection windows, and accuracy
- Legal implications: Laws on testing for psychedelics, workplace policies, and legal consequences
- False positives: Substances causing incorrect test results for psychedelic mushrooms
- Testing frequency: How often tests are conducted and factors influencing testing schedules
- Privacy concerns: Ethical issues around testing for psychedelic use and personal rights

Detection methods: Urine, blood, hair tests for psilocybin metabolites, detection windows, and accuracy
Psilocybin, the active compound in psychedelic mushrooms, breaks down into metabolites like psilocin and 4-hydroxyindole-3-acetic acid (4-OH-IAA) once ingested. Detecting these metabolites in biological samples is the cornerstone of drug testing for mushroom use. Urine tests, the most common method, can identify psilocin for up to 24 hours after ingestion, though this window shrinks with occasional use. Blood tests offer a narrower detection window of 6 to 12 hours, making them less practical for routine screening. Hair tests, while less frequently used due to higher costs and complexity, can detect psilocybin metabolites for up to 90 days, providing a longer-term usage history. Each method’s efficacy depends on factors like dosage (typically 10–50 mg of psilocybin), frequency of use, and individual metabolism.
Urine testing is the go-to method for psilocybin detection due to its simplicity and cost-effectiveness. Laboratories use immunoassay screening followed by confirmatory gas chromatography-mass spectrometry (GC-MS) to ensure accuracy. However, false positives can occur due to cross-reactivity with structurally similar compounds, such as certain antidepressants or over-the-counter medications. To minimize errors, individuals should disclose all medications to the testing facility. For those anticipating a test, staying hydrated can dilute urine concentration, though this may trigger retesting if the sample is deemed too weak.
Blood tests, while less common, are highly accurate for recent psilocybin use. They detect psilocin directly, with levels peaking 20–40 minutes after ingestion and declining rapidly thereafter. This method is often used in forensic or medical settings rather than workplace screenings. Hair tests, on the other hand, provide a historical record of drug use. Psilocybin metabolites are incorporated into hair strands as they grow, with each centimeter representing approximately one month of history. However, external contamination (e.g., touching mushrooms) can lead to false positives, necessitating careful sample preparation.
Detection windows vary significantly across methods and individuals. For instance, a single dose of 20 mg psilocybin may be undetectable in urine after 24 hours, while chronic users might test positive for up to 72 hours. Hair tests offer the longest window but are less useful for pinpointing recent use. Accuracy also differs: urine tests are 95–99% accurate when confirmed with GC-MS, while hair tests have a higher margin of error due to environmental factors. Understanding these nuances is crucial for interpreting results, whether for legal, medical, or personal reasons.
Practical tips for individuals facing psilocybin testing include abstaining from use for at least 48 hours before a urine test and avoiding hair treatments that could strip metabolites from strands. For those in states where psilocybin is decriminalized or used medically, documentation from a healthcare provider may be necessary to contextualize positive results. Employers and testing facilities should also be aware of the limitations of each method to avoid unjust consequences. Ultimately, while detection methods exist, their effectiveness hinges on the testing approach, individual factors, and the context of use.
Can Bears Safely Eat Mushrooms? Exploring Their Diet and Risks
You may want to see also

Legal implications: Laws on testing for psychedelics, workplace policies, and legal consequences
Drug testing for psychedelic mushrooms, primarily psilocybin, is legally complex and varies widely by jurisdiction. In the United States, psilocybin is classified as a Schedule I controlled substance under federal law, meaning it is illegal to possess, manufacture, or distribute. However, some states and cities, such as Oregon and Denver, have decriminalized or legalized psilocybin for medical or therapeutic use. This patchwork of laws creates ambiguity for employers and individuals regarding drug testing policies. For instance, while federal law permits testing for psilocybin, local laws may protect employees from adverse actions based on its use in certain contexts.
Workplace policies on drug testing for psychedelics are equally nuanced. Employers must navigate federal, state, and local regulations to ensure compliance. In states where psilocybin is decriminalized, companies may still enforce zero-tolerance policies, but they risk legal challenges if employees argue discrimination based on protected medical use. For example, Oregon’s Measure 109 allows for regulated psilocybin therapy, potentially shielding employees who use it under professional supervision. Employers should consult legal counsel to draft policies that balance safety concerns with evolving legal protections for psychedelic use.
The legal consequences of testing positive for psilocybin depend on the context. In workplaces, employees may face disciplinary action, including termination, if they violate company policies. However, in jurisdictions with decriminalization or legalization, employees might have grounds to contest such actions, particularly if the use was medically sanctioned. Criminally, possession of psilocybin remains a federal offense, punishable by fines and imprisonment, though enforcement varies. For instance, small amounts in decriminalized areas may result in a citation rather than arrest, but this is not a guarantee of leniency.
Practical tips for individuals and employers include staying informed about local laws, as they change rapidly. Employees should disclose medically supervised psilocybin use to employers proactively, especially in states with protections. Employers should update drug testing policies to reflect legal shifts and consider whether testing for psychedelics aligns with workplace safety goals. For example, testing for psilocybin, which has a short detection window (24–48 hours), may not effectively address long-term impairment concerns. Instead, focus on observable behaviors and performance metrics to ensure a fair and legally sound approach.
In conclusion, the legal landscape surrounding drug testing for psychedelic mushrooms is dynamic and requires careful consideration. Employers and individuals must stay informed, adapt policies, and seek legal guidance to navigate this complex terrain. As laws continue to evolve, proactive measures will be essential to avoid unintended legal consequences and ensure compliance with both federal and local regulations.
Can Yeast Create Mushrooms? Unraveling the Fungal Connection
You may want to see also

False positives: Substances causing incorrect test results for psychedelic mushrooms
Substances like over-the-counter medications and certain foods can trigger false positives for psychedelic mushrooms on drug tests. Psilocybin, the active compound in magic mushrooms, is typically detected through specialized urine or blood tests, but these tests aren’t always foolproof. For instance, antihistamines such as diphenhydramine (found in Benadryl) or ibuprofen have been known to cause false positives for psychedelics. Even something as common as a high-protein diet or consuming hemp seeds can lead to misleading results due to cross-reactivity with test antibodies. Understanding these potential pitfalls is crucial for accurate interpretation of drug test outcomes.
Consider the case of a 28-year-old who tested positive for psilocybin after taking a high dose of melatonin for sleep. Melatonin, a popular supplement, has been reported to interfere with certain drug test panels, particularly those using immunoassay methods. Similarly, SSRI antidepressants like sertraline or fluoxetine can produce false positives due to their structural similarity to psychedelic compounds. Even prescription medications for ADHD, such as methylphenidate, have been flagged in isolated cases. These examples highlight the importance of confirming positive results with more precise tests, such as gas chromatography-mass spectrometry (GC-MS), which can differentiate between substances more accurately.
For those concerned about false positives, proactive steps can minimize risk. First, disclose all medications and supplements to the testing authority beforehand. Second, avoid consuming large amounts of hemp or poppy seeds, as they contain trace amounts of compounds that mimic psychedelics in tests. Third, request a confirmatory test if a positive result seems unlikely. For example, a 30-year-old vegan who tested positive for psilocybin later discovered the culprit was a daily smoothie containing lion’s mane mushrooms, which share some chemical similarities with psychedelic varieties. Awareness and transparency are key to avoiding misinterpretations.
Comparatively, false positives for psychedelics are less common than for substances like THC or opioids, but their impact can be equally disruptive. Unlike THC, which lingers in the body for weeks, psilocybin is metabolized quickly, typically undetectable in urine after 24 hours. However, cross-reactivity with other substances means even short-term exposure to certain medications or foods can lead to confusion. For instance, a 45-year-old on a prescription for tramadol (a pain reliever) tested positive for psychedelics due to the drug’s metabolic byproducts. This underscores the need for nuanced testing protocols and informed decision-making by both testers and test-takers.
In practical terms, anyone facing a drug test should approach it with caution and knowledge. Avoid self-medicating with over-the-counter drugs or supplements without understanding their potential impact on test results. For employers or testing facilities, investing in advanced testing methods can reduce the likelihood of false positives. For individuals, keeping a detailed log of consumed substances in the days leading up to a test can provide critical context if results are disputed. Ultimately, while false positives for psychedelic mushrooms are rare, their consequences can be significant, making vigilance and education essential tools in navigating drug testing accurately.
Reheating Mushrooms: Safe Practices and Tips for Delicious Results
You may want to see also
Explore related products
$76.95 $81.99

Testing frequency: How often tests are conducted and factors influencing testing schedules
Drug testing for psychedelic mushrooms, specifically psilocybin, is a nuanced process influenced by detection windows and testing methodologies. Psilocybin is typically detectable in urine for 24-48 hours after ingestion, in blood for up to 12 hours, and in hair follicles for up to 90 days. However, testing frequency is not solely determined by detection times. Employers, legal systems, or medical professionals may conduct tests based on specific triggers or policies, such as post-accident investigations, reasonable suspicion, or routine screenings in safety-sensitive industries. Understanding these factors is crucial for interpreting testing schedules and their implications.
In workplace settings, testing frequency often aligns with industry regulations and company policies. For instance, transportation and aviation sectors may enforce random testing quarterly or biannually to ensure compliance with safety standards. In contrast, creative industries might forgo testing unless there is a direct concern about impairment. Age categories can also play a role; younger employees (under 25) in high-risk roles may face more frequent testing due to statistical correlations between age and substance use. Employers must balance legal requirements with ethical considerations, ensuring testing schedules are fair and justified.
Medical and legal contexts introduce additional variables. Probation or parole programs may require biweekly or monthly testing for individuals with substance-related offenses, regardless of the specific drug. In clinical trials involving psilocybin, participants undergo frequent testing (e.g., weekly or biweekly) to monitor dosage adherence and safety. Dosage values, such as microdoses (0.1-0.3 grams) versus macrodoses (2-5 grams), can influence detection times and testing frequency, as higher doses may leave longer-lasting metabolites. Practical tip: Always disclose psilocybin use to medical professionals if undergoing testing, as false positives or misinterpretations can occur.
Comparatively, self-imposed testing schedules differ significantly. Individuals using psilocybin for therapeutic or recreational purposes may test themselves periodically to ensure compliance with personal goals or legal boundaries. At-home test kits, while less accurate than lab-based methods, offer a convenient way to monitor psilocybin metabolites. However, reliance on these kits should be tempered with awareness of their limitations, such as shorter detection windows (24-48 hours) and potential cross-reactivity with other substances. For precise results, professional testing remains the gold standard.
In conclusion, testing frequency for psilocybin is shaped by a complex interplay of detection windows, regulatory mandates, and individual circumstances. Whether in workplace, legal, medical, or personal contexts, understanding these factors empowers individuals to navigate testing schedules effectively. Practical takeaway: Stay informed about the specific policies governing your situation and consider the dosage and frequency of psilocybin use when anticipating potential tests. Transparency and knowledge are key to managing outcomes in drug testing scenarios.
Mushrooms and Antidepressants: Safe Combination or Risky Interaction?
You may want to see also

Privacy concerns: Ethical issues around testing for psychedelic use and personal rights
Psychedelic mushrooms, containing psilocybin, are increasingly recognized for their therapeutic potential, yet the ability to test for their use raises profound privacy concerns. Unlike substances like cannabis or opioids, psilocybin is metabolized quickly, leaving a narrow detection window in urine or blood tests. However, advancements in hair follicle testing and biomarker research threaten to extend this window, potentially exposing individuals to scrutiny long after use. This technological creep challenges the ethical boundaries of personal autonomy, particularly when testing is mandated by employers or institutions.
Consider the case of a therapist undergoing routine workplace drug screening. A positive test for psilocybin metabolites could jeopardize their career, even if the use was legal, therapeutic, or outside of work hours. This scenario underscores the tension between organizational policies and individual rights. While employers argue for safety and productivity, employees counter that off-duty conduct should remain private, especially when it involves substances with proven medical benefits. The lack of clear legal protections for psychedelic users exacerbates this conflict, leaving individuals vulnerable to discrimination.
From a legal standpoint, the Fourth Amendment protects against unreasonable searches, but courts have often sided with employers in drug testing cases, citing workplace safety as a compelling interest. However, this rationale weakens when applied to psychedelics, which are not associated with immediate impairment like alcohol or stimulants. For instance, psilocybin’s effects typically last 4–6 hours, and residual metabolites do not correlate with current intoxication. Testing for past use thus becomes a privacy invasion rather than a safety measure, raising questions about the legitimacy of such practices.
To mitigate these concerns, policymakers could adopt a tiered approach to drug testing. For example, testing for psychedelics could be restricted to roles with high safety risks, such as transportation or heavy machinery operation. Even then, detection methods should focus on current impairment rather than past use. Additionally, individuals should have the right to explain positive results, particularly if the use was medicinal or occurred in a decriminalized jurisdiction. Such safeguards would balance organizational needs with respect for personal autonomy.
Ultimately, the ethical dilemma of testing for psychedelic mushrooms boils down to a clash between societal control and individual freedom. As research continues to validate their therapeutic value, society must reconsider whether monitoring their use aligns with principles of privacy and justice. Without clear boundaries, the expansion of testing capabilities risks stigmatizing users and stifling access to potentially life-changing treatments. Protecting this realm of personal choice is not just a legal issue—it’s a moral imperative.
Creamy Comfort: Campbell's Mushroom Chicken Soup Recipe Ideas & Tips
You may want to see also
Frequently asked questions
Yes, drug tests can detect psychedelic mushrooms, specifically psilocybin and its metabolite psilocin, through specialized tests like urine, blood, or hair follicle screenings.
Psilocybin and psilocin are typically detectable in urine for 24–48 hours after use, though this can vary based on factors like dosage, metabolism, and frequency of use.
No, standard drug tests (e.g., 5-panel or 10-panel tests) do not screen for psilocybin or psilocin. Specialized tests are required to detect these substances.
Yes, hair follicle tests can detect psilocybin use for up to 90 days or longer, as drug metabolites are incorporated into the hair shaft as it grows.
![[5 pack] Prime Screen 14 Panel Urine Drug Test Cup - Instant Testing Marijuana (THC),OPI,AMP, BAR, BUP, BZO, COC, mAMP, MDMA, MTD, OXY, PCP, PPX, TCA](https://m.media-amazon.com/images/I/71cI114sLUL._AC_UL320_.jpg)
![Prime Screen [5 Pack] 6 Panel Urine Drug Test Kit (THC-Marijuana, BZO-Benzos, MET-Meth, OPI, AMP, COC), WDOA-264](https://m.media-amazon.com/images/I/71hU5zzuEaL._AC_UL320_.jpg)
![Easy@Home 5 Panel Urine Drug Test Kit [5 Pack] - THC/Marijuana, Cocaine, OPI/Opiates, AMP, BZO All Drugs Testing Strips in One Kit - at Home Use Screening Test with Results in 5 Mins #EDOAP-754](https://m.media-amazon.com/images/I/81pqr85M3-L._AC_UL320_.jpg)

![Prime Screen-12 Panel Multi Drug Urine Test Compact Cup (THC 50, AMP,BAR,BUP,BZO,COC,mAMP/MET,MDMA,MOP/OPI,MTD,OXY,PCP) C-Cup-[1 Pack]](https://m.media-amazon.com/images/I/714z5mLCPkL._AC_UL320_.jpg)



![Easy@Home Marijuana Urine Drug Test Kit [15 Pack] - THC Tests for Home Use - Weed Detox Testing Kits with 50ng/ml Cutoff Level #EDTH-114](https://m.media-amazon.com/images/I/71oGjFr07tL._AC_UL320_.jpg)





![Prime Screen [5 Pack] 5 Panel Urine Drug Test Kit - Testing Instantly for 5 Different Drugs AMP, COC, MET (Meth), OPI, THC (Marijuana) - WDOA-254](https://m.media-amazon.com/images/I/71FsDMfvdFL._AC_UL320_.jpg)

![Prime Screen [10 Pack] 6 Panel Urine Test Kit](https://m.media-amazon.com/images/I/810ZqCaS13L._AC_UL320_.jpg)
![Prime Screen 14 Panel Urine Drug Test Cup Instant Testing Marijuana (THC),OPI,AMP, BAR, BUP, BZO, COC, mAMP, MDMA, MTD, OXY, PCP, PPX, TCA [1 Pack]](https://m.media-amazon.com/images/I/7176xYFYqTL._AC_UL320_.jpg)