The idea of mushrooms growing on human feet may seem bizarre, but it raises intriguing questions about the conditions under which fungi thrive. While mushrooms typically grow in damp, dark environments rich in organic matter, human feet can sometimes create similar conditions due to prolonged moisture, warmth, and lack of airflow, especially in cases of athlete’s foot or fungal infections. However, true mushrooms require specific substrates like soil or wood to develop, which the human body does not provide. Instead, what might appear as mushrooms on feet is likely a fungal infection or dermatophyte growth, not actual mushrooms. Understanding this distinction highlights the importance of foot hygiene and the fascinating ways fungi interact with our bodies.
| Characteristics | Values |
|---|---|
| Possibility of Feet Growing Mushrooms | No, human feet cannot grow mushrooms. Mushrooms require specific conditions (e.g., organic matter, moisture, and spores) that human skin does not provide. |
| Common Misconception | The idea may stem from fungal infections like athlete's foot, which can cause skin discoloration or texture changes, but these are not mushrooms. |
| Fungal Infections on Feet | Conditions like athlete's foot, toenail fungus, or ringworm are caused by fungi (e.g., Trichophyton), not mushrooms. |
| Mushroom Growth Requirements | Mushrooms need a substrate (e.g., wood, soil), moisture, warmth, and spores, none of which are naturally present on human feet. |
| Skin Conditions Mimicking Mushrooms | Warts, corns, or severe fungal infections might resemble mushroom-like growths but are not mushrooms. |
| Medical Advice | Persistent foot abnormalities should be evaluated by a healthcare professional to rule out infections or other conditions. |
| Prevention of Fungal Infections | Keep feet clean, dry, and avoid walking barefoot in damp public areas. Use antifungal treatments if necessary. |
Explore related products
What You'll Learn
- Causes of Fungal Growth: Damp, dark environments and poor foot hygiene can lead to fungal infections
- Types of Foot Fungi: Athlete’s foot, toenail fungus, and ringworm are common fungal infections
- Symptoms to Watch For: Itching, redness, peeling skin, and discolored nails indicate fungal growth
- Prevention Tips: Keep feet dry, wear breathable shoes, and avoid walking barefoot in public areas
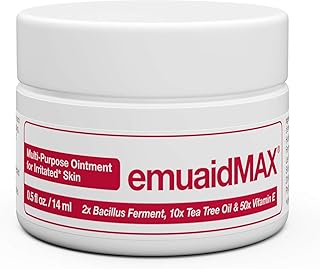
- Treatment Options: Antifungal creams, powders, and medications can effectively treat foot fungi

Causes of Fungal Growth: Damp, dark environments and poor foot hygiene can lead to fungal infections
Fungal infections thrive in environments that mimic their natural habitats—damp, dark, and warm spaces. Your feet, when confined in sweaty shoes or socks, become the perfect breeding ground for fungi like *Trichophyton*, the culprit behind athlete’s foot. Moisture softens the skin, making it easier for fungi to penetrate, while darkness and warmth accelerate their growth. For instance, wearing non-breathable footwear for extended periods can increase foot temperature by up to 3°C, creating an ideal fungal incubator.
To prevent this, adopt a two-pronged approach: reduce moisture and improve airflow. After showers or workouts, thoroughly dry your feet, especially between the toes, where moisture lingers. Rotate shoes daily to allow them to air out for at least 24 hours, and opt for moisture-wicking socks made of natural fibers like cotton or merino wool. For those prone to sweating, antiperspirant foot sprays or powders containing aluminum chloride (6%–20% concentration) can help control moisture.
Poor foot hygiene compounds the problem by allowing dead skin cells and dirt to accumulate, providing fungi with a food source. Neglecting to wash your feet daily or walking barefoot in communal areas like locker rooms increases exposure to fungal spores. A study published in the *Journal of Clinical Medicine* found that individuals who washed their feet daily were 40% less likely to develop fungal infections compared to those who did not. Incorporate a gentle exfoliation routine once a week to remove dead skin, and disinfect nail clippers and pumice stones after each use to avoid cross-contamination.
Comparatively, while mushrooms require specific conditions like organic matter and prolonged darkness to grow, foot fungi are far more opportunistic. Unlike mushrooms, which take weeks to develop, fungal infections like athlete’s foot can manifest within days of exposure. However, both thrive in similar environments, underscoring the importance of keeping feet clean, dry, and well-ventilated. By addressing these factors, you not only prevent fungal infections but also eliminate the conditions that could theoretically support mushroom growth—though such cases remain firmly in the realm of myth.
Shipping Dry Mushrooms to the USA: Legal Guidelines and Tips
You may want to see also

Types of Foot Fungi: Athlete’s foot, toenail fungus, and ringworm are common fungal infections
While your feet won't sprout portobellos, they can become a breeding ground for various fungi, leading to uncomfortable and sometimes unsightly infections. Let's delve into three common culprits: athlete's foot, toenail fungus, and ringworm.
Athlete's Foot: The Itchy Invader
Imagine a persistent itch between your toes, accompanied by burning, cracking skin, and an unpleasant odor. This is the hallmark of athlete's foot, caused by fungi thriving in warm, moist environments like sweaty socks and shoes. Athletes, gym-goers, and anyone prone to sweaty feet are particularly susceptible. Treatment involves keeping feet dry, using antifungal powders or creams (like clotrimazole or miconazole), and wearing breathable footwear. Severe cases may require oral antifungal medication prescribed by a doctor.
Toenail Fungus: A Stubborn Discoloration
Yellowed, thickened, and brittle toenails are telltale signs of a fungal infection. This fungus, often the same culprit behind athlete's foot, infiltrates the nail bed, feeding on keratin. Treatment is notoriously slow, requiring consistent application of topical antifungal medications for several months. Oral antifungals are more effective but come with potential side effects and require monitoring by a healthcare professional. Prevention is key: keep nails trimmed short, avoid walking barefoot in public areas, and disinfect nail clippers regularly.
Ringworm: Not a Worm, But a Circular Woe
Despite its name, ringworm is caused by a fungus, not a worm. It manifests as a red, scaly, ring-shaped rash that can appear anywhere on the body, including the feet. This highly contagious infection thrives in warm, humid environments and can spread through direct contact or shared items like towels and shoes. Treatment involves antifungal creams or ointments applied directly to the rash. Keeping the affected area clean and dry is crucial for healing.
Beyond the Itch: When to Seek Help
While these fungal infections are common and often treatable at home, seeking medical attention is crucial if:
- Symptoms persist despite over-the-counter treatments.
- The infection spreads rapidly or becomes severe.
- You have diabetes or a weakened immune system, as fungal infections can lead to more serious complications.
Remember, while mushrooms won't sprout from your feet, these fungal infections can cause significant discomfort and embarrassment. By understanding the types, causes, and treatment options, you can take proactive steps to keep your feet healthy and fungus-free.
Can Psilocybe Mushrooms Thrive Outside Sterile Environments? Exploring Growth Conditions
You may want to see also

Symptoms to Watch For: Itching, redness, peeling skin, and discolored nails indicate fungal growth
While your feet won’t sprout mushrooms like a forest floor, they can become a breeding ground for fungal infections that mimic the conditions fungi thrive in. Damp, dark environments—think sweaty socks and tight shoes—create the perfect habitat for fungi to flourish. The first signs of this unwelcome invasion often manifest as subtle yet persistent symptoms: itching, redness, peeling skin, and discolored nails. These aren’t just minor annoyances; they’re your body’s alarm system signaling a fungal takeover.
Itching, the earliest and most common symptom, is your skin’s response to the irritation caused by fungal spores. It’s not just a fleeting discomfort—persistent itching can lead to scratching, which breaks the skin’s barrier and allows the fungus to spread further. Redness typically accompanies itching, indicating inflammation as your immune system battles the intruder. If left unchecked, the skin may begin to peel, a sign that the fungus is disrupting the skin’s natural renewal process. This peeling isn’t just unsightly; it’s a clear indicator that the infection is deepening.
Discolored nails are another telltale sign, often overlooked until the condition worsens. Nails may turn yellow, brown, or even black as the fungus feeds on the keratin in the nail bed. This discoloration is usually accompanied by thickening and brittleness, making the nails difficult to trim and prone to cracking. While it’s tempting to hide these changes with polish, doing so traps moisture and exacerbates the problem. Early intervention is key—over-the-counter antifungal creams or oral medications prescribed by a dermatologist can halt the progression before permanent damage occurs.
Prevention is just as critical as treatment. Keep feet dry by changing socks frequently, especially after exercise, and opt for breathable footwear. Dust antifungal powder in shoes and rotate them daily to allow them to dry completely. For those prone to fungal infections, incorporating a weekly foot soak with diluted vinegar (1 part vinegar to 2 parts water) can help maintain a pH level hostile to fungi. Remember, fungi thrive in neglect—regular inspection and care can keep your feet fungus-free and healthy.
Can You Freeze Sautéed Mushrooms? A Complete Preservation Guide
You may want to see also
Explore related products

Prevention Tips: Keep feet dry, wear breathable shoes, and avoid walking barefoot in public areas
Feet, constantly encased in shoes, are prime real estate for moisture buildup, creating an environment where fungi thrive. This is the core principle behind preventing foot-related fungal infections, including those that might metaphorically make your feet a "mushroom garden."
The Moisture-Fungus Connection: Fungi, including those causing athlete's foot and toenail fungus, adore damp, dark environments. Sweat trapped in socks and shoes provides the perfect breeding ground. Every step generates heat and moisture, and without proper ventilation, this creates a sauna-like condition ideal for fungal growth.
Imagine a damp basement – it's a haven for mold. Your feet, similarly, become susceptible when moisture lingers.
Breathable Footwear: Your First Line of Defense
Think of your shoes as a second skin for your feet. Opt for materials like leather, canvas, or mesh that allow air circulation. Avoid synthetic materials that trap moisture. Consider it a ventilation system for your feet. Rotate your shoes daily, allowing them to fully dry out between wears. This simple practice disrupts the fungal life cycle by denying them a consistently damp habitat.
For active individuals or those prone to sweating, moisture-wicking socks are essential. Look for materials like merino wool or synthetic blends designed to draw sweat away from the skin.
Barefoot Beware: Public Spaces are Fungal Hotspots
Public showers, pool decks, and locker rooms are breeding grounds for fungi. Walking barefoot in these areas exposes your feet to spores that can easily take hold in a warm, moist environment. Think of it as walking through a fungal minefield. Always wear flip-flops or shower shoes in these spaces. It's a small habit with a significant impact on preventing fungal infections.
Drying Rituals: A Crucial Step
After showers, baths, or any activity that wets your feet, thorough drying is paramount. Pay special attention to the spaces between your toes, where moisture tends to linger. Use a clean towel and consider a hairdryer on a cool setting for extra thoroughness. This simple act removes the moisture fungi crave, making it harder for them to establish a foothold.
Adaptogenic Mushrooms and Digestion: Unlocking Gut Health Benefits
You may want to see also

Treatment Options: Antifungal creams, powders, and medications can effectively treat foot fungi
Foot fungi, though not literal mushrooms, thrive in the same damp, warm conditions that mushrooms favor. Fortunately, antifungal treatments are designed to combat these unwelcome guests effectively. Antifungal creams, such as terbinafine (Lamisil) or clotrimazole (Lotrimin), are a frontline defense. Apply a thin layer to clean, dry skin twice daily for 2–4 weeks, ensuring coverage of the entire affected area and surrounding skin to prevent recurrence. For best results, pair this with good foot hygiene: wash feet daily, dry thoroughly (especially between toes), and wear moisture-wicking socks.
Powders offer an alternative for those who prefer a drier application or have extensive foot sweating. Products like miconazole powder (Zeasorb) or tolnaftate (Tinactin) can be dusted onto feet and inside shoes daily. Powders work by absorbing moisture, creating an inhospitable environment for fungal growth. However, they’re less effective for severe infections, as they may not penetrate deeply enough. Combine powders with creams for stubborn cases, using the cream at night and powder during the day to maximize efficacy.
For persistent or severe infections, oral antifungal medications like terbinafine or itraconazole may be prescribed. These systemic treatments target fungi from within but require caution due to potential side effects, such as liver function abnormalities. Typically, a 6–12 week course is prescribed, with dosage varying by age and weight (e.g., 250 mg daily for adults). Regular blood tests may be necessary to monitor liver health. Oral medications are often reserved for cases unresponsive to topical treatments or when the infection has spread extensively.
Practical tips can enhance treatment success: rotate shoes daily to allow them to dry completely, avoid walking barefoot in communal areas, and disinfect footwear with antifungal sprays. For children, ensure medications are age-appropriate and follow pediatrician guidance, as dosages differ significantly. While antifungals are effective, consistency is key—stopping treatment prematurely can lead to recurrence. With the right approach, foot fungi can be eradicated, restoring healthy skin and preventing the conditions that might otherwise make your feet a breeding ground for unwanted growth.
Delicious Porcini Mushroom Creations: Recipes and Culinary Inspiration
You may want to see also
Frequently asked questions
No, human feet cannot biologically grow mushrooms. Mushrooms are fungi that grow in specific environmental conditions, not on human skin.
The joke often stems from the idea that sweaty, unwashed feet can create a damp, dark environment similar to where mushrooms thrive, though they don’t actually grow on feet.
Certain fungal infections, like athlete’s foot, can cause skin changes, but they do not resemble mushrooms. These infections require medical treatment.
Keep feet clean, dry, and well-ventilated. Wear breathable footwear, change socks regularly, and avoid walking barefoot in damp public areas.