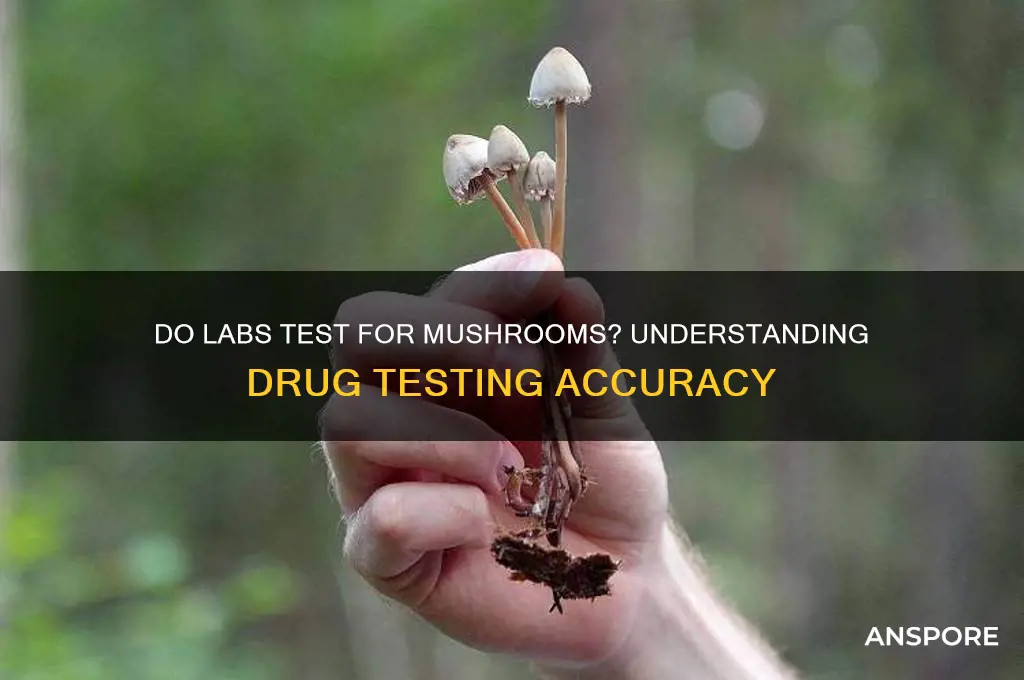
The question of whether labs test for mushrooms is a pertinent one, especially given the increasing interest in psychedelic substances and their potential therapeutic applications. Laboratories often conduct tests to detect the presence of various substances, including mushrooms, for a range of purposes such as forensic analysis, medical research, or drug screening. These tests can identify specific compounds found in mushrooms, like psilocybin or psilocin, which are responsible for their psychoactive effects. The methods employed may include sophisticated techniques such as liquid chromatography-tandem mass spectrometry (LC-MS/MS) or enzyme-linked immunosorbent assays (ELISAs), ensuring accurate and reliable results. Understanding the capabilities of labs in detecting mushrooms is crucial for legal, medical, and research contexts, as it impacts areas from drug policy to clinical trials.
| Characteristics | Values |
|---|---|
| Test Type | Laboratory-based testing |
| Purpose | Detect presence of mushrooms or their components (e.g., psilocybin, psilocin) |
| Sample Types | Urine, blood, hair, saliva, or tissue samples |
| Detection Window | Varies by sample type: urine (1-3 days), blood (12-24 hours), hair (up to 90 days) |
| Testing Methods | Gas chromatography-mass spectrometry (GC-MS), liquid chromatography-tandem mass spectrometry (LC-MS/MS), enzyme-linked immunosorbent assay (ELISA) |
| Accuracy | High, especially with confirmatory testing using GC-MS or LC-MS/MS |
| Common Targets | Psilocybin, psilocin, baeocystin, norbaeocystin |
| Legal Status | Depends on jurisdiction; psilocybin is illegal in many countries but decriminalized or legalized in some regions for medical/therapeutic use |
| Medical Use | Increasingly studied for therapeutic purposes (e.g., depression, anxiety, PTSD) |
| False Positives | Possible but rare; confirmatory testing minimizes risk |
| Cost | Varies by lab and method; typically $50-$200 per test |
| Turnaround Time | 24-72 hours for initial results; confirmatory testing may take longer |
| Availability | Widely available in forensic, clinical, and research labs |
Explore related products
What You'll Learn

Types of mushroom tests
When it comes to testing for mushrooms, laboratories employ various methods to identify the presence of specific fungal species or their byproducts. These tests are crucial in fields such as medicine, food safety, and environmental monitoring. The types of mushroom tests can be broadly categorized based on their purpose, methodology, and the substances they detect. Here are some of the primary types of mushroom tests conducted in labs:
Microscopic Identification is one of the most traditional and widely used methods for mushroom testing. This technique involves examining the physical characteristics of fungal samples under a microscope. Mycologists look for distinct features such as spore shape, size, and color, as well as the structure of hyphae and fruiting bodies. While this method is highly accurate for identifying known species, it requires expertise and may not be suitable for detecting microscopic fungal fragments or toxins. It is commonly used in research and forensic settings to classify mushroom species.
DNA-Based Testing has revolutionized mushroom identification by providing a highly accurate and efficient method. This approach involves extracting and analyzing the genetic material (DNA) from a fungal sample. Techniques like polymerase chain reaction (PCR) and DNA sequencing are employed to identify specific genes or sequences unique to certain mushroom species. DNA-based testing is particularly useful for identifying mushrooms that are difficult to distinguish morphologically or for detecting hidden fungal contaminants in food and environmental samples. It is widely used in clinical labs to diagnose fungal infections and in the food industry to ensure product safety.
Biochemical Tests focus on detecting specific enzymes, proteins, or metabolites produced by mushrooms. For example, certain fungi produce unique enzymes that can be identified using enzymatic assays. Additionally, tests like high-performance liquid chromatography (HPLC) and mass spectrometry (MS) are used to detect fungal toxins, such as aflatoxins or ochratoxins, which are harmful to humans and animals. These tests are critical in food safety and medical diagnostics, as they can quantify the presence of toxic substances even at low concentrations. Biochemical tests are often used in conjunction with other methods to provide comprehensive results.
Immunological Assays utilize antibodies to detect specific fungal proteins or antigens. Techniques such as enzyme-linked immunosorbent assay (ELISA) are commonly employed to identify mushrooms or their toxins rapidly. These tests are highly sensitive and specific, making them ideal for screening large numbers of samples in clinical or industrial settings. Immunological assays are particularly useful for detecting fungal infections in patients or monitoring fungal contamination in agricultural products. However, they require the availability of specific antibodies, which may limit their application to well-studied fungal species.
Chromatographic and Spectroscopic Methods are advanced techniques used to analyze the chemical composition of mushrooms. Gas chromatography (GC) and liquid chromatography (LC) coupled with mass spectrometry (MS) can identify and quantify a wide range of fungal compounds, including secondary metabolites and toxins. These methods provide detailed information about the chemical profile of a mushroom sample, making them invaluable in research and quality control. They are often used in pharmaceutical development to study medicinal mushrooms or in environmental studies to assess fungal biodiversity.
In summary, the types of mushroom tests available in labs vary widely, each with its strengths and applications. From traditional microscopic identification to cutting-edge DNA and biochemical analyses, these methods ensure accurate detection and characterization of mushrooms in diverse contexts. Understanding these testing types is essential for professionals in fields where fungal identification and monitoring are critical.
Mushrooms: Mammals or Not?
You may want to see also

Accuracy of lab testing methods
The accuracy of lab testing methods for detecting mushrooms is a critical aspect of ensuring reliable results, whether for medical, forensic, or environmental purposes. Labs commonly employ techniques such as polymerase chain reaction (PCR), liquid chromatography-mass spectrometry (LC-MS), and enzyme-linked immunosorbent assay (ELISA) to identify mushroom species or their compounds. PCR is highly accurate for DNA-based identification, offering species-level precision, but its effectiveness depends on the quality of the sample and the reference database used. Contamination or degraded DNA can lead to false negatives or misidentification, highlighting the need for rigorous sample preparation and validation protocols.
LC-MS is another widely used method, particularly for detecting specific mushroom compounds like psilocybin or amanitin. This technique provides high sensitivity and specificity, allowing labs to quantify trace amounts of these substances. However, accuracy can be compromised by matrix effects, where other components in the sample interfere with the analysis. Calibration with standards and proper sample extraction techniques are essential to mitigate these issues. Additionally, the choice of ionization method and chromatographic conditions can significantly impact the reliability of results, requiring skilled technicians and standardized procedures.
ELISA is often employed for rapid screening of mushroom toxins or allergens but is generally less accurate than PCR or LC-MS. Its reliance on antibodies can lead to cross-reactivity with similar compounds, resulting in false positives. While ELISA is cost-effective and quick, confirmatory testing with more precise methods is often necessary to ensure accuracy. This two-tiered approach is particularly important in clinical or forensic settings, where incorrect results can have serious consequences.
Emerging technologies, such as next-generation sequencing (NGS) and biosensors, are enhancing the accuracy of mushroom testing. NGS provides comprehensive genetic profiling, enabling the identification of multiple species or strains in a single sample. However, its high cost and complexity limit its widespread use. Biosensors, on the other hand, offer real-time detection with high sensitivity but may lack the specificity required for complex samples. As these technologies evolve, they hold promise for improving the accuracy and efficiency of mushroom testing.
In conclusion, the accuracy of lab testing methods for mushrooms depends on the technique used, sample quality, and procedural rigor. While PCR, LC-MS, and ELISA are effective, each has limitations that must be addressed through careful validation and standardization. Advances in technology continue to refine these methods, but ongoing research and quality control are essential to ensure reliable results in diverse applications. Labs must stay informed about best practices and invest in training and equipment to maintain high accuracy in mushroom testing.
Mushroom and Lamb: A Match Made in Heaven?
You may want to see also

Common mushrooms detected in tests
When it comes to laboratory testing for mushrooms, certain species are more commonly detected due to their prevalence in the environment, their psychoactive properties, or their potential toxicity. One of the most frequently tested mushrooms is Psilocybe cubensis, a psychoactive species known for its psilocybin content. Labs often screen for this mushroom in drug tests or forensic analyses, as its consumption can lead to altered states of consciousness. Psilocybin is a controlled substance in many countries, making its detection crucial in legal and medical contexts. Tests typically identify the presence of psilocybin or its metabolite, psilocin, using techniques like liquid chromatography-mass spectrometry (LC-MS).
Another common mushroom detected in tests is Amanita muscaria, also known as the fly agaric. This mushroom is recognizable by its bright red cap with white spots and contains psychoactive compounds like muscimol and ibotenic acid. While it is less commonly consumed recreationally compared to psilocybin mushrooms, its distinctive appearance and potential for toxicity make it a target for identification in poisoning cases. Labs use specific assays to detect muscimol and ibotenic acid, often in cases of accidental ingestion or intentional misuse.
Amanita phalloides, or the death cap, is a highly toxic mushroom frequently detected in poisoning cases. This species contains amatoxins, which can cause severe liver and kidney damage, often leading to fatal outcomes if left untreated. Labs prioritize testing for amatoxins in cases of mushroom poisoning, as early detection is critical for administering appropriate medical interventions. Techniques such as enzyme-linked immunosorbent assays (ELISA) and polymerase chain reaction (PCR) are commonly used to identify the presence of these toxins.
In addition to toxic species, labs also test for edible mushrooms like Agaricus bisporus, the common button mushroom, and Lentinula edodes, known as shiitake. While these mushrooms are safe for consumption, testing may be conducted to ensure they are free from contaminants such as heavy metals, pesticides, or harmful bacteria. Such tests are particularly important in the food industry to maintain safety standards and consumer trust.
Lastly, Cordyceps species, known for their medicinal properties, are increasingly detected in labs due to their use in dietary supplements. Tests often focus on identifying active compounds like cordycepin and ensuring product authenticity. As the demand for functional mushrooms grows, so does the need for accurate testing to verify their composition and safety. In summary, labs commonly detect a range of mushrooms, from psychoactive and toxic species to edible and medicinal varieties, using specialized techniques tailored to each type.
Mushrooms for Babies: Are They Safe?
You may want to see also
Explore related products

Purpose of mushroom testing in labs
Mushroom testing in labs serves multiple critical purposes, primarily centered around safety, identification, and research. One of the primary reasons labs test for mushrooms is to ensure food safety. Many mushrooms are consumed globally, and while some are edible and nutritious, others are toxic or even deadly. Labs analyze mushroom samples to detect harmful species or toxins, such as amatoxins found in certain poisonous varieties like the Death Cap (*Amanita phalloides*). This testing is essential for food producers, restaurants, and consumers to prevent accidental poisoning and ensure compliance with regulatory standards.
Another key purpose of mushroom testing is species identification. Mushrooms exhibit significant morphological diversity, and many species look alike, making visual identification challenging even for experts. Labs use advanced techniques like DNA sequencing, microscopy, and biochemical assays to accurately identify mushroom species. This is particularly important in forensic cases, ecological studies, and commercial applications where precise identification is required. For example, distinguishing between a toxic look-alike and an edible species can have life-saving implications.
Mushroom testing also plays a vital role in pharmacological and medical research. Many mushrooms contain bioactive compounds with potential therapeutic benefits, such as antioxidants, anti-inflammatory agents, and anticancer properties. Labs test mushrooms to isolate, identify, and quantify these compounds, contributing to drug development and natural medicine research. For instance, the mushroom *Ganoderma lucidum* (Reishi) is studied for its immunomodulatory effects, and *Psathyrella candolleana* has been investigated for its potential in treating neurological disorders.
In addition to safety and research, mushroom testing supports environmental monitoring and conservation efforts. Mushrooms are sensitive bioindicators of ecosystem health, as they absorb and accumulate environmental contaminants like heavy metals and pesticides. Labs analyze mushroom samples to assess soil and air quality, providing valuable data for environmental studies and policy-making. This testing helps identify pollution hotspots and monitor the impact of human activities on natural habitats.
Lastly, mushroom testing is crucial for commercial and industrial applications. The mushroom industry, including cultivation and product development, relies on lab testing to ensure quality, consistency, and safety. Labs test for factors like nutrient content, contamination, and shelf life in mushroom-based products. Additionally, testing supports innovation in areas like mycoremediation, where mushrooms are used to clean up environmental pollutants, and biomaterials, where fungal mycelium is explored as a sustainable alternative to plastics.
In summary, the purpose of mushroom testing in labs is multifaceted, encompassing safety, identification, research, environmental monitoring, and commercial applications. These tests are essential for protecting public health, advancing scientific knowledge, and leveraging the potential of mushrooms in various fields. As interest in mushrooms grows, so does the importance of rigorous lab testing to unlock their benefits while mitigating risks.
Drying Chanterelle Mushrooms: A Step-by-Step Guide
You may want to see also

Timeframe for mushroom test results
When considering the timeframe for mushroom test results, it’s essential to understand that labs do indeed test for mushrooms, but the process and duration vary depending on the type of test and the lab’s capabilities. Typically, mushroom testing falls into two main categories: identification of mushroom species and detection of psychoactive compounds (such as psilocybin). For species identification, which is often done for forensic or safety purposes, results can be available within 24 to 48 hours if the lab uses rapid methods like microscopy or DNA sequencing. However, more comprehensive analysis may take 3 to 5 business days to ensure accuracy.
For tests detecting psychoactive compounds like psilocybin, the timeframe can be slightly longer due to the complexity of the analysis. Labs often use techniques like high-performance liquid chromatography (HPLC) or mass spectrometry (MS), which require careful preparation and processing. In such cases, results may take 2 to 7 days, depending on the lab’s workload and the urgency of the request. If the sample needs to be shipped to a specialized facility, additional time for transit should be factored in, potentially extending the timeframe to 1 to 2 weeks.
Urgent or expedited testing is sometimes available for an additional fee, which can reduce the turnaround time to 24 to 48 hours for both species identification and compound detection. This option is particularly useful in medical emergencies or legal cases where quick results are critical. However, not all labs offer expedited services, so it’s important to inquire in advance.
For home testing kits, which are becoming more popular for personal use, the timeframe is significantly shorter. These kits typically provide results within 15 to 30 minutes, but their accuracy can vary. They are best used for preliminary screening rather than definitive identification or quantification of compounds. Always confirm home test results with a professional lab for reliability.
In summary, the timeframe for mushroom test results ranges from 15 minutes to 2 weeks, depending on the type of test, lab capabilities, and urgency. For precise and reliable results, professional lab testing is recommended, with most standard results available within 2 to 7 days. Always communicate your specific needs with the lab to ensure the appropriate testing method and timeframe are selected.
The Ultimate Guide to Perfectly Seared Mushrooms
You may want to see also
Frequently asked questions
Standard lab drug tests, such as those for employment or probation, typically do not test for mushrooms (psilocybin or psilocin) unless specifically requested. Most panels focus on common substances like marijuana, cocaine, opioids, and amphetamines.
Yes, specialized drug tests can detect mushrooms. These tests look for psilocybin or psilocin, the active compounds in mushrooms, but they are not routinely included in standard screenings and must be specifically ordered.
Mushrooms (psilocybin/psilocin) are typically detectable in urine for 24-48 hours after use, in blood for up to 12 hours, and in hair follicles for up to 90 days. Detection times can vary based on dosage, metabolism, and individual factors.
![Easy@Home 5 Panel Urine Drug Test Kit [5 Pack] - THC/Marijuana, Cocaine, OPI/Opiates, AMP, BZO All Drugs Testing Strips in One Kit - at Home Use Screening Test with Results in 5 Mins #EDOAP-754](https://m.media-amazon.com/images/I/81pqr85M3-L._AC_UL320_.jpg)


![Prime Screen [5 Pack] 6 Panel Urine Drug Test Kit (THC-Marijuana, BZO-Benzos, MET-Meth, OPI, AMP, COC), WDOA-264](https://m.media-amazon.com/images/I/71hU5zzuEaL._AC_UL320_.jpg)



![Prime Screen Multi-Drug Urine Test Cup 16 Panel Kit (AMP,BAR,BUP,BZO,COC,mAMP,MDMA,MOP/OPI,MTD,OXY,PCP,THC, ETG, FTY, TRA, K2) -[1 Pack]-CDOA-9165EFTK](https://m.media-amazon.com/images/I/718HvC-tp-L._AC_UL320_.jpg)