Surgical masks have become a ubiquitous tool in both medical and everyday settings, primarily used to prevent the spread of respiratory droplets and protect against airborne pathogens. However, their effectiveness in blocking mold spores, which are microscopic particles released by fungi, remains a topic of interest. Mold spores are significantly smaller than bacteria and viruses, raising questions about whether the porous structure of surgical masks can adequately filter them out. While surgical masks are designed to capture larger particles, their ability to prevent mold spore inhalation depends on factors such as the mask’s fit, material, and the concentration of spores in the environment. Understanding this relationship is crucial for individuals in mold-prone areas or those with mold allergies, as it can influence their choice of protective measures.
| Characteristics | Values |
|---|---|
| Effectiveness Against Mold Spores | Surgical masks are not specifically designed to filter mold spores. |
| Filtration Efficiency | Typically filters particles ≥ 5-10 microns (mold spores range 3-100 microns). |
| Material | Made of non-woven polypropylene, which does not inherently block spores. |
| Fit | Loose-fitting; does not create a seal, allowing spores to bypass. |
| Recommended Use | Primarily for large droplets and splashes, not airborne particles like spores. |
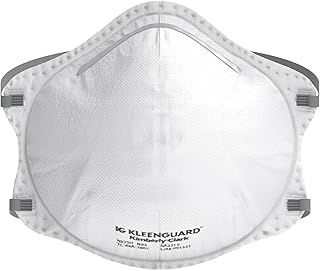
| Alternatives | N95 respirators or P100 masks are more effective against mold spores. |
| Reusability | Not designed for reuse; may lose efficacy if exposed to moisture/mold. |
| Regulatory Standards | Meets ASTM Level 1/2/3 for fluid resistance, not spore filtration. |
| Common Misconception | Often mistaken for protection against all airborne particles. |
| Practical Application | Offers minimal protection; not a substitute for proper mold remediation PPE. |
Explore related products
What You'll Learn

Effectiveness of Surgical Masks Against Mold Spores
Surgical masks, primarily designed to block large respiratory droplets, offer limited protection against mold spores due to their size and the masks’ filtration capabilities. Mold spores, typically ranging from 2 to 10 microns, can penetrate the loose-fitting structure of surgical masks, which are not designed to filter particles smaller than 100 microns effectively. While surgical masks can trap some larger mold spores, they are not a reliable barrier for prolonged or high-exposure situations. For individuals with mold allergies or those working in mold-prone environments, this limitation is critical to understand.
To maximize protection against mold spores, consider pairing surgical masks with additional measures. Using a mask with a higher filtration efficiency, such as an N95 respirator, is more effective because it can filter particles as small as 0.3 microns. Additionally, ensuring a tight seal around the nose and mouth is crucial, as mold spores can easily bypass gaps in the mask. For those in mold remediation or inspection roles, combining masks with protective eyewear and gloves provides a more comprehensive defense. Always follow OSHA guidelines for mold exposure, which emphasize proper ventilation and personal protective equipment (PPE).
A comparative analysis reveals that surgical masks are better suited for preventing the spread of respiratory illnesses rather than protecting against environmental allergens like mold spores. Cloth masks, often considered less effective than surgical masks for virus protection, perform similarly against mold spores due to their inability to filter microscopic particles. In contrast, HEPA filters, commonly used in air purifiers, are far more effective at capturing mold spores, trapping 99.97% of particles as small as 0.3 microns. This highlights the importance of selecting the right tool for the specific hazard at hand.
Practical tips for minimizing mold spore exposure include reducing indoor humidity below 50%, fixing leaks promptly, and using dehumidifiers in damp areas. When cleaning moldy surfaces, wear an N95 respirator and ensure the area is well-ventilated. For individuals with mold sensitivities, avoiding outdoor activities during high-spore seasons (typically late summer to early fall) can help manage symptoms. While surgical masks may offer minimal protection, they should not be relied upon as the sole defense against mold spores in high-risk scenarios. Always prioritize equipment and practices specifically designed for mold mitigation.
Effective Ways to Remove Mold Spores from Clothing Safely
You may want to see also

Filtration Capabilities of Surgical Mask Materials
Surgical masks are primarily designed to filter out large respiratory droplets and particles, but their effectiveness against smaller entities like mold spores depends heavily on the materials used. The most common material in surgical masks is polypropylene, a non-woven fabric that forms the mask’s primary filtration layer. This layer typically captures particles through a combination of mechanical interception, inertial impaction, and electrostatic attraction. While surgical masks are not certified as respirators (like N95 masks), they can still trap particles as small as 0.3 microns with varying efficiency, generally ranging from 60% to 80%. Mold spores, which average between 3 to 40 microns in size, fall well within this range, suggesting that surgical masks can provide some level of protection against them.
To maximize filtration, surgical masks often incorporate multiple layers, each serving a distinct purpose. The outer layer repels fluids, the middle layer filters particles, and the inner layer absorbs moisture from the wearer’s breath. This multi-layered design enhances the mask’s ability to trap mold spores, which are often carried in airborne dust or water droplets. However, it’s crucial to note that surgical masks are not airtight; gaps around the edges can allow particles to bypass the filter. Proper fit, achieved by molding the nose bridge and ensuring snug coverage, significantly improves filtration efficiency. For individuals exposed to mold in environments like construction sites or water-damaged buildings, combining a surgical mask with additional protective measures, such as goggles and gloves, is advisable.
Comparing surgical masks to higher-grade respirators highlights their limitations in mold spore filtration. N95 respirators, for instance, are designed to filter out at least 95% of airborne particles, including those as small as 0.3 microns, and provide a tighter seal to minimize leakage. In contrast, surgical masks are not regulated for fit or filtration efficiency to the same degree. For individuals with mold allergies or asthma, prolonged exposure to mold spores can trigger severe reactions, making the choice of protective gear critical. While surgical masks offer a practical and cost-effective solution for general use, they may not provide sufficient protection in high-risk scenarios. In such cases, opting for a respirator with a higher filtration rating is a safer choice.
Practical tips for enhancing the filtration capabilities of surgical masks include ensuring they are worn correctly, replacing them regularly (especially if damp or soiled), and using masks with additional features like activated carbon layers. Activated carbon can help absorb volatile organic compounds (VOCs) often associated with mold growth, though it does not directly filter spores. For those working in mold-prone areas, pairing a surgical mask with a portable air purifier or HEPA filter system can further reduce airborne spore concentrations. While surgical masks are not a foolproof solution, their proper use can significantly reduce the risk of inhaling mold spores in low to moderate exposure situations. Always assess the specific conditions and consult guidelines from health and safety organizations to determine the most appropriate protective measures.
Milky Spore for Blueberries: Is It Necessary for Healthy Plants?
You may want to see also

Proper Usage to Prevent Mold Inhalation
Surgical masks, while primarily designed to block large respiratory droplets, can also act as a barrier against mold spores, which typically range from 3 to 100 microns in size. However, their effectiveness depends on proper usage and fit. Mold spores are ubiquitous in damp environments, and inhalation can lead to respiratory issues, allergies, or infections. To maximize protection, ensure the mask fits snugly over the nose and mouth, minimizing gaps where spores could enter. This is particularly crucial in mold-prone areas like basements, attics, or during cleanup after water damage.
Proper usage begins with selecting the right type of mask. Standard surgical masks are sufficient for most mold exposure scenarios, but in high-concentration environments, consider using an N95 respirator, which filters out 95% of airborne particles, including smaller mold spores. Always check for proper certification (e.g., NIOSH approval for N95 masks) to ensure reliability. Before entering a moldy area, inspect the mask for tears or damage, as even small defects can compromise its effectiveness.
Wearing the mask correctly is equally important. Place it over your nose and mouth, securing it with ear loops or ties. Press the metal strip over the bridge of your nose to create a tight seal. Avoid touching the mask while in use, as this can contaminate it or disrupt the fit. If the mask becomes damp or soiled, replace it immediately, as moisture can reduce its filtering efficiency and potentially harbor mold growth itself.
Duration of use is another critical factor. Surgical masks are not designed for extended wear and can lose their effectiveness over time. Replace the mask every 4–6 hours or sooner if it becomes uncomfortable or compromised. For individuals with respiratory conditions or weakened immune systems, consult a healthcare provider for personalized recommendations on mask usage and exposure limits.
Finally, combine mask usage with other preventive measures for comprehensive protection. Maintain good ventilation in mold-prone areas by using fans or opening windows. Wear protective clothing, such as gloves and long sleeves, to avoid skin contact with mold. After exposure, dispose of the mask properly and wash your hands thoroughly to prevent cross-contamination. By adhering to these guidelines, you can significantly reduce the risk of mold inhalation and its associated health risks.
Do Rhizopus Spores Have Flagella? Unraveling the Fungal Mobility Mystery
You may want to see also
Explore related products

Limitations of Surgical Masks in Moldy Environments
Surgical masks, while effective in blocking large respiratory droplets, offer limited protection against mold spores due to their size and the masks’ design. Mold spores, typically ranging from 2 to 100 microns in diameter, can easily pass through the loose-fitting edges and porous material of standard surgical masks. For context, N95 respirators, which filter out particles as small as 0.3 microns, are far more effective in moldy environments. If you’re working in an area with visible mold growth or high spore counts, relying solely on a surgical mask could leave you exposed to airborne contaminants.
Consider the scenario of a homeowner cleaning mold from a damp basement. Wearing a surgical mask might provide a false sense of security, as it primarily protects against larger particles like dust and debris, not the microscopic spores that become airborne during disturbance. Without a proper seal and filtration, these spores can enter the respiratory system, potentially triggering allergies, asthma, or other health issues. In such cases, pairing a surgical mask with goggles and gloves is a start, but upgrading to a respirator is the safer choice.
From a practical standpoint, surgical masks are not designed for prolonged use in mold remediation. Their primary function is to prevent the spread of pathogens from the wearer, not to protect the wearer from environmental hazards. For individuals with pre-existing respiratory conditions or weakened immune systems, exposure to mold spores can be particularly dangerous. If you must work in a moldy environment, follow the EPA’s guidelines: use an N95 respirator, ensure proper ventilation, and limit exposure time to minimize risk.
Comparatively, surgical masks are adequate for everyday use in low-risk settings but fall short in specialized scenarios like mold cleanup. For instance, a study published in the *Journal of Occupational and Environmental Hygiene* found that surgical masks filtered only 30-50% of airborne particles in the 1-5 micron range, which includes many mold spores. In contrast, N95 respirators achieved over 95% filtration efficiency. This stark difference highlights why surgical masks should not be the go-to choice for mold-related tasks.
In conclusion, while surgical masks serve a vital role in healthcare and general hygiene, their limitations in moldy environments cannot be overlooked. Their inability to filter small particles, lack of a secure seal, and unsuitability for prolonged exposure make them inadequate for protecting against mold spores. For anyone dealing with mold, investing in proper protective equipment, such as an N95 respirator, is a critical step in safeguarding health. Always prioritize safety over convenience when working in contaminated areas.
Befriending Epic Creatures in Spore: A Guide to Unlikely Alliances
You may want to see also

Comparing Surgical Masks to Respirators for Mold Protection
Surgical masks, while effective at blocking large respiratory droplets, are not designed to filter out microscopic mold spores. These spores, typically 2-10 microns in size, can easily pass through the loose-fitting, porous material of a surgical mask. This limitation makes surgical masks inadequate for protecting against mold exposure, especially in environments with high spore concentrations.
Respirators, particularly N95 or higher-rated models, offer significantly better protection against mold spores due to their tighter fit and advanced filtration capabilities. These devices are designed to filter out at least 95% of airborne particles, including mold spores, when worn correctly. For individuals working in mold remediation, construction, or other high-risk environments, respirators are essential. The Occupational Safety and Health Administration (OSHA) recommends using N95 respirators or better for tasks involving mold exposure, emphasizing the importance of proper fit testing to ensure maximum effectiveness.
When comparing the two, the key difference lies in their design and intended use. Surgical masks are primarily meant to protect others from the wearer’s respiratory emissions, while respirators are engineered to protect the wearer from inhaling hazardous particles. For mold protection, respirators provide a critical barrier that surgical masks cannot. However, respirators require careful handling, including proper donning, doffing, and storage, to maintain their integrity. Surgical masks, though less effective for mold, are more convenient for everyday use in low-risk settings.
Practical considerations also play a role in choosing between the two. Respirators can be more expensive and less comfortable to wear for extended periods, whereas surgical masks are lightweight and disposable. For short-term, low-exposure situations, a surgical mask may suffice, but for prolonged or high-risk mold exposure, investing in a respirator is non-negotiable. Always follow manufacturer guidelines and OSHA regulations to ensure proper use and maximum protection.
Are Mirasmius Spores White? Unveiling the Truth About Their Color
You may want to see also
Frequently asked questions
Surgical masks can provide some level of protection against mold spores by acting as a physical barrier, but they are not specifically designed to filter out all airborne particles, especially smaller spores.
Surgical masks offer limited protection in moldy environments. For better protection, N95 respirators or masks with higher filtration efficiency are recommended.
Wearing a surgical mask may reduce exposure to mold spores and alleviate allergy symptoms, but it is not a guaranteed solution. Proper ventilation and mold remediation are essential.
Surgical masks can trap some mold spores on their surface, but they are not airtight and may allow smaller spores to pass through. Regularly changing the mask is important in moldy conditions.