Contaminated mushrooms pose a significant health risk, as they can contain toxins that lead to severe illness or even death. While many mushroom species are safe and nutritious, others, such as the deadly Amanita phalloides or the hallucinogenic Psilocybe species, can cause poisoning if consumed. Accidental ingestion often occurs due to misidentification of wild mushrooms or improper handling during cultivation. Symptoms of mushroom poisoning range from gastrointestinal distress to organ failure, depending on the toxin involved. Public awareness and proper education on mushroom identification are crucial to prevent such incidents, yet cases of contamination continue to be reported worldwide, raising concerns about food safety and the need for stricter regulations in foraging and distribution.
| Characteristics | Values |
|---|---|
| Common Symptoms | Nausea, vomiting, diarrhea, abdominal pain, hallucinations, confusion, seizures, liver failure, kidney failure, death |
| Time of Onset | 6 hours to 24 hours after ingestion, depending on mushroom type |
| Common Contaminated Mushrooms | Amanita phalloides (Death Cap), Amanita ocreata (Destroying Angel), Galerina marginata, Lepiota species |
| Toxic Compounds | Amatoxins (most common), Orellanine, Muscarine, Ibotenic acid |
| Treatment | Activated charcoal, gastric lavage, supportive care, liver transplant in severe cases |
| Prevention | Proper identification of mushrooms before consumption, avoid foraging unless experienced, cook mushrooms thoroughly |
| Fatality Rate | 10-50% for Amanita phalloides poisoning |
| Geographic Distribution | Worldwide, with higher incidence in regions with abundant wild mushrooms |
| Demographics | Often foragers, immigrants, children, and those mistaking toxic mushrooms for edible ones |
| Recent Cases | Data varies by region, but cases are reported annually worldwide. Specific numbers are not readily available in a single source. |
Explore related products
What You'll Learn

Symptoms of mushroom poisoning
Mushroom poisoning occurs when someone ingests toxic mushrooms, which can lead to a range of symptoms depending on the type of mushroom and the toxins involved. Symptoms can appear anywhere from 20 minutes to several hours after consumption, making it crucial to recognize the signs early. The severity of symptoms varies widely, from mild gastrointestinal discomfort to life-threatening organ failure. Understanding these symptoms is essential for prompt treatment and prevention of long-term harm.
One of the most common types of mushroom poisoning involves gastrointestinal symptoms, often caused by mushrooms containing toxins like amatoxins or muscarine. These symptoms typically include nausea, vomiting, abdominal pain, and diarrhea. Such reactions can be mistaken for food poisoning but may persist or worsen over time. If someone experiences these symptoms after consuming wild mushrooms, it is vital to seek medical attention immediately, as delayed treatment can lead to dehydration or more severe complications.
Neurological symptoms are another significant indicator of mushroom poisoning, particularly with mushrooms containing toxins like ibotenic acid or muscimol. These symptoms may include confusion, hallucinations, dizziness, and muscle spasms. In severe cases, seizures or loss of consciousness can occur. Such neurological effects can be alarming and require urgent medical intervention to prevent long-term brain damage or other serious outcomes.
Cardiovascular and respiratory symptoms may also arise in cases of mushroom poisoning, especially with toxins like coprine or orellanine. These symptoms can include rapid heartbeat, low blood pressure, difficulty breathing, or even respiratory failure. Orellanine, for instance, is known to cause delayed kidney damage, leading to symptoms like reduced urine output or swelling. These systemic effects highlight the importance of identifying the specific mushroom involved to guide appropriate treatment.
In severe cases, mushroom poisoning can lead to organ failure, particularly liver or kidney damage, which may be irreversible without timely intervention. Symptoms of liver failure include jaundice, dark urine, and abdominal swelling, while kidney failure may present as reduced urine output or swelling in the legs. Such life-threatening complications underscore the need for immediate medical care, including supportive treatments like dialysis or, in extreme cases, organ transplantation.
Finally, it is crucial to note that some toxic mushrooms, like those containing amatoxins, can cause symptoms that initially subside, giving a false sense of recovery. However, this can be followed by a more severe phase of organ damage. This biphasic pattern emphasizes the importance of monitoring and medical supervision even if initial symptoms seem to improve. Always avoid consuming wild mushrooms unless they are positively identified by an expert, as misidentification is a common cause of poisoning.
Does Mario Eat Mushrooms? Exploring the Iconic Power-Up Mystery
You may want to see also

Common toxic mushroom species
While I cannot directly search the internet, I can provide you with a comprehensive overview of common toxic mushroom species, which is crucial information for anyone concerned about mushroom poisoning. Mushroom poisoning cases are not uncommon, and many instances occur due to the misidentification of toxic species with edible ones. Here is an in-depth look at some of the most notorious toxic mushrooms:
Amanita Species: The Amanita genus is perhaps the most infamous group of poisonous mushrooms. It includes the deadly *Amanita phalloides*, commonly known as the Death Cap, and *Amanita ocreata*, the Destroying Angel. These mushrooms are responsible for the majority of fatal mushroom poisonings worldwide. They often resemble edible species like the Paddy Straw mushroom (*Agaricus campestris*) and can be found in similar habitats, making them a significant risk for foragers. The toxins in Amanitas, such as amatoxins, cause severe liver and kidney damage, leading to symptoms like vomiting, diarrhea, and in severe cases, organ failure and death.
Galerina Marginata: This small brown mushroom is often found growing on wood and is sometimes mistaken for edible species like the Common Store Mushroom (*Agaricus bisporus*). *Galerina marginata* contains the same deadly amatoxins as the Amanita species, making it extremely dangerous. Its unassuming appearance and habitat can easily deceive inexperienced foragers.
Conocybe Filaris: Commonly known as the 'Conocybe,' this mushroom is another producer of amatoxins. It is often found in lawns and gardens, especially in urban areas, and can be mistaken for edible lawn mushrooms. Its small size and nondescript appearance make it a hidden danger, especially for children who might encounter it while playing outdoors.
Cortinarius Species: The Cortinarius genus includes a large number of species, many of which are toxic. These mushrooms often have a rusty-brown spore print and can be found in forests. Some Cortinarius species contain the toxin orellanine, which causes severe kidney damage. The symptoms of poisoning may not appear for several days, making it challenging to associate the illness with mushroom consumption.
False Morels (Gyromitra Species): These mushrooms are known for their brain-like appearance and are sometimes collected by foragers due to their resemblance to true morels. However, false morels contain a toxic compound called gyromitrin, which can cause severe gastrointestinal symptoms and, in some cases, lead to coma or death. Proper identification is crucial, as some people attempt to detoxify false morels through cooking, which is not always effective.
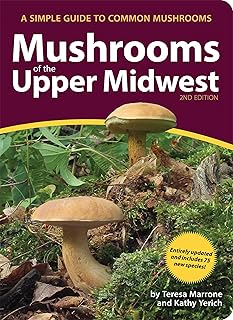
It is essential to emphasize that proper identification is key to avoiding toxic mushroom species. Many poisonous mushrooms have edible look-alikes, and even experienced foragers can make mistakes. Always consult reliable field guides and, if possible, seek guidance from mycologists or local mushroom experts before consuming any wild mushrooms. Remember, when in doubt, throw it out!
Mushrooms Before Colonoscopy: Safe or Risky Prep Choice?
You may want to see also

Treatment for contamination exposure
When someone has ingested contaminated mushrooms, immediate and appropriate treatment is crucial to mitigate potential health risks. The first step is to identify the symptoms, which can vary widely depending on the type of mushroom and the toxins involved. Common symptoms include gastrointestinal distress (nausea, vomiting, diarrhea), hallucinations, confusion, seizures, or liver and kidney damage. If any symptoms are observed or if there is suspicion of mushroom poisoning, seek medical attention immediately. Do not wait for symptoms to worsen, as some toxins can cause life-threatening complications within hours.
Upon arrival at a medical facility, gastric decontamination may be initiated to prevent further absorption of toxins. This can involve induced vomiting or gastric lavage (stomach pumping), but these procedures are typically performed only if the ingestion was recent (within 1-2 hours). Activated charcoal may also be administered to bind the toxins in the gastrointestinal tract and prevent their absorption into the bloodstream. However, the effectiveness of these measures depends on the timing and the specific toxin involved.
Supportive care is a cornerstone of treatment for mushroom poisoning. This includes intravenous fluids to maintain hydration and electrolyte balance, especially if the patient is experiencing severe vomiting or diarrhea. In cases of severe toxicity, medications may be given to manage specific symptoms, such as anticonvulsants for seizures or benzodiazepines for agitation or hallucinations. Monitoring of vital signs, liver and kidney function, and blood work is essential to assess the extent of organ damage and guide treatment.
For certain types of mushroom poisoning, specific antidotes may be available. For example, silybin (a component of milk thistle) has been used in cases of *Amanita phalloides* (death cap) poisoning to protect the liver from damage. Similarly, N-acetylcysteine may be used to treat poisoning from mushrooms containing hepatotoxic compounds. However, the availability and effectiveness of these antidotes vary, and their use should be guided by medical professionals familiar with mushroom toxicity.
Prevention is always the best approach. If you are foraging for mushrooms, ensure you are knowledgeable about the species or consult an expert. Avoid consuming any mushroom unless you are absolutely certain it is safe. In case of accidental ingestion, do not induce vomiting or use home remedies without medical advice, as these actions can sometimes worsen the situation. Instead, contact a poison control center or healthcare provider immediately and provide as much information as possible about the mushroom consumed, including photographs if available. Prompt and informed action can significantly improve outcomes in cases of contaminated mushroom ingestion.
Do Mockingbirds Eat Mushrooms? Unveiling Their Surprising Diet Habits
You may want to see also
Explore related products
$19 $34.95

Preventing accidental mushroom ingestion
Avoid foraging without expertise unless you are accompanied by an experienced mycologist or forager. Even seasoned foragers double-check their findings, as misidentification is a common cause of accidental poisoning. If you are unsure about a mushroom’s identity, do not consume it. Additionally, teach children about the dangers of eating wild mushrooms and supervise them during outdoor activities to prevent curiosity-driven ingestion. Pets are also at risk, so monitor them in areas where mushrooms grow and remove any suspicious fungi from your yard.
Properly label and store edible mushrooms to avoid confusion in the kitchen. If you forage or purchase wild mushrooms, store them separately from other foods and clearly label them. Cross-contamination can occur if toxic mushrooms are mixed with safe ones, so always handle them with care. Be especially cautious when preparing meals for others, as accidental inclusion of a toxic mushroom can have dire consequences for multiple people. If you are serving wild mushrooms, inform your guests of their source and assure them of their safety.
When in doubt, seek professional guidance. If you suspect someone has ingested a contaminated mushroom, act quickly. Save a sample of the mushroom for identification and contact a poison control center or healthcare provider immediately. Time is critical in treating mushroom poisoning, and early intervention can significantly improve outcomes. Remember, symptoms may not appear immediately, so do not wait for signs of illness before seeking help.
Finally, promote community awareness about the risks of accidental mushroom ingestion. Share knowledge with friends, family, and neighbors, especially in areas where wild mushrooms are prevalent. Local health departments or mycological societies may offer workshops or resources to help educate the public. By fostering a culture of caution and informed decision-making, we can reduce the incidence of accidental mushroom poisoning and ensure safer enjoyment of the natural world.
Do Amphibians Eat Mushrooms? Exploring Their Diet and Habits
You may want to see also

Long-term health effects of poisoning
Consuming contaminated mushrooms can lead to severe long-term health effects, depending on the type of toxin ingested. One of the most well-known toxins is amatoxin, found in certain species of Amanita mushrooms. Amatoxin poisoning can cause irreversible liver damage, a condition known as hepatotoxicity. Even after surviving the acute phase of poisoning, individuals may develop chronic liver disease, cirrhosis, or liver failure, requiring long-term medical management or even liver transplantation. Regular monitoring of liver function is essential for survivors to detect and manage complications early.
Another long-term consequence of mushroom poisoning involves kidney damage, particularly from toxins like orellanine found in mushrooms such as *Cortinarius* species. Orellanine poisoning often presents with delayed symptoms, sometimes appearing days after ingestion. Chronic kidney disease or renal failure can develop, necessitating dialysis or kidney transplantation in severe cases. Survivors may face lifelong restrictions on diet and fluid intake to manage kidney function.
Neurological damage is another significant long-term effect, especially from mushrooms containing toxins like ibotenic acid or muscimol, found in *Amanita muscaria* and *Amanita pantherina*. These toxins can cause persistent neurological symptoms such as memory loss, cognitive impairment, seizures, or psychiatric disorders like anxiety and depression. Rehabilitation and ongoing neurological care may be required to address these issues.
Gastrointestinal complications can also persist in individuals who have ingested contaminated mushrooms. Repeated exposure to certain toxins can lead to chronic gastrointestinal disorders, including irritable bowel syndrome (IBS), malabsorption issues, or recurrent gastrointestinal infections. Dietary modifications and long-term medications may be necessary to manage these conditions effectively.
Lastly, psychological trauma and post-traumatic stress disorder (PTSD) are often overlooked long-term effects of mushroom poisoning. Survivors may experience anxiety, fear of food, or avoidance behaviors related to foraging or consuming mushrooms. Psychological support and therapy can play a crucial role in helping individuals recover from the emotional impact of such a traumatic event.
In summary, the long-term health effects of mushroom poisoning can be severe and multifaceted, affecting the liver, kidneys, nervous system, gastrointestinal tract, and mental health. Prompt medical intervention and long-term monitoring are critical to managing these complications and improving the quality of life for survivors.
Can Dwarf Hamsters Safely Eat Mushrooms? A Complete Dietary Guide
You may want to see also
Frequently asked questions
Yes, many people have accidentally consumed contaminated or poisonous mushrooms, often mistaking them for edible varieties.
Symptoms vary depending on the type of mushroom but can include nausea, vomiting, diarrhea, abdominal pain, hallucinations, organ failure, and in severe cases, death.
Only consume mushrooms that are positively identified by an expert, purchased from a reputable source, or foraged with absolute certainty. Never eat wild mushrooms unless you are 100% sure of their safety.