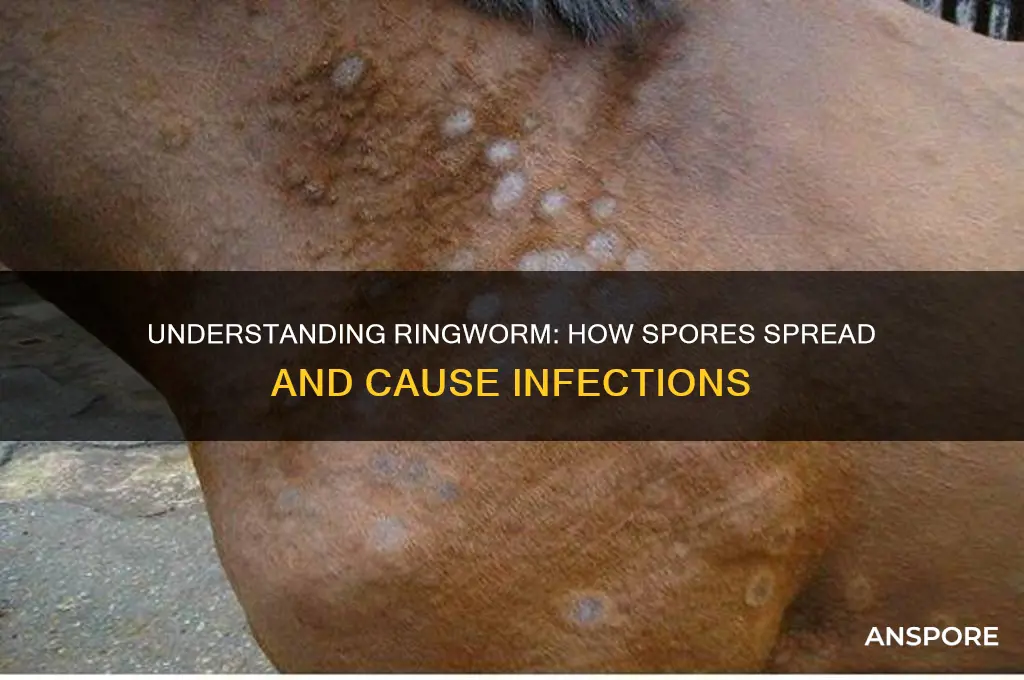
Ringworm, despite its name, is not caused by a worm but by a fungus known as dermatophytes. These fungi produce spores that are highly resilient and can survive for extended periods in various environments, including soil, surfaces, and even on the skin of infected individuals or animals. Ringworm spores spread primarily through direct contact with an infected person, animal, or contaminated object, such as clothing, towels, or grooming tools. Additionally, spores can be transmitted indirectly through shared spaces like locker rooms, gyms, or areas where pets roam. Once the spores come into contact with a suitable host, they can germinate and cause a ringworm infection, characterized by circular, red, itchy rashes. Understanding how these spores spread is crucial for implementing effective prevention and control measures.
| Characteristics | Values |
|---|---|
| Mode of Transmission | Direct contact with infected humans, animals, or contaminated objects. |
| Survival on Surfaces | Spores can survive on surfaces like combs, brushes, towels, and soil for months. |
| Airborne Spread | Limited; spores may become airborne in dusty environments but are not primarily spread this way. |
| Skin-to-Skin Contact | Highly effective in spreading spores between humans or animals. |
| Animal-to-Human Transmission | Common, especially from pets like cats, dogs, and livestock. |
| Environmental Contamination | Spores thrive in warm, moist environments, increasing risk of spread. |
| Incubation Period | 4–14 days after exposure before symptoms appear. |
| Reinfection Risk | High if contaminated items are not disinfected or replaced. |
| Seasonal Prevalence | More common in warm, humid climates. |
| Immune System Impact | Individuals with weakened immune systems are more susceptible. |
Explore related products
What You'll Learn
- Direct Skin Contact: Spores transfer through touch with infected humans, animals, or contaminated surfaces
- Shared Items: Spores spread via clothing, towels, bedding, or sports gear used by infected individuals
- Animal Transmission: Pets like cats and dogs can carry spores and infect humans through contact
- Soil Exposure: Prolonged contact with soil containing spores can lead to ringworm infection
- Environmental Survival: Spores remain viable in environments for months, increasing indirect transmission risk

Direct Skin Contact: Spores transfer through touch with infected humans, animals, or contaminated surfaces
Ringworm spores, known as arthrospores, are remarkably resilient and can survive on surfaces for months, waiting for the right conditions to infect a new host. Direct skin contact is one of the most common ways these spores spread, making it a critical area of focus for prevention. When you touch an infected person, animal, or contaminated object, the spores can easily transfer to your skin, where they thrive in warm, moist environments. This is why activities like sharing personal items, petting infected animals, or even leaning against a contaminated gym bench can unknowingly expose you to ringworm.
Consider the scenario of a child playing with a pet cat that has ringworm. The cat’s fur carries the spores, and when the child pets the animal, the spores transfer to their hands. If the child then touches their face, scalp, or another part of their body without washing their hands, the spores can take hold and cause an infection. Similarly, in a gym setting, athletes often share equipment like mats or towels, which can harbor spores from an infected individual. A single touch is all it takes for the spores to find a new host, underscoring the importance of hygiene in shared spaces.
To minimize the risk of ringworm through direct skin contact, adopt a proactive approach to personal and environmental cleanliness. After interacting with animals, especially those with unknown health histories, wash your hands thoroughly with soap and water for at least 20 seconds. In public spaces, avoid sharing personal items like towels, brushes, or clothing, and wipe down gym equipment before and after use with disinfectant wipes. Parents should educate children about the importance of handwashing, particularly after playing with pets or other children, as kids are more susceptible to ringworm due to their developing immune systems and frequent close contact with others.
Comparing human-to-human and animal-to-human transmission highlights the need for tailored precautions. While both routes involve direct skin contact, animals often carry ringworm asymptomatically, making it harder to identify the risk. Regularly inspect pets for signs of infection, such as circular patches of hair loss or scaling skin, and consult a veterinarian if you suspect ringworm. For humans, encourage early treatment of infections to reduce spore shedding and avoid close contact with infected individuals until their treatment is complete. By understanding these nuances, you can take targeted steps to protect yourself and others from this highly contagious fungal infection.
Do Spores Carry Their Own Food Supply? Unveiling the Survival Mechanism
You may want to see also

Shared Items: Spores spread via clothing, towels, bedding, or sports gear used by infected individuals
Ringworm spores, known as arthrospores, are remarkably resilient and can survive on inanimate objects for months, silently waiting for a new host. This makes shared items like clothing, towels, bedding, and sports gear prime vectors for transmission. When an infected person uses these items, the spores cling to the fabric, ready to transfer to the next person who comes into contact with them. A single infected towel, for instance, can become a breeding ground for spores, spreading the fungus to multiple individuals in a household or gym setting.
Consider the lifecycle of a shared gym towel. An athlete with ringworm wipes their sweat, unknowingly depositing spores onto the fabric. Hours later, another gym-goer uses the same towel, providing the spores with warmth, moisture, and direct skin contact—ideal conditions for infection. This scenario highlights the importance of personal hygiene and the need for dedicated, frequently washed items in high-traffic areas. For children, who often share clothing and bedding during sleepovers or sports activities, the risk is even higher due to their developing immune systems and close physical interactions.
To mitigate this risk, adopt a proactive approach to laundry and item handling. Wash shared items in hot water (at least 140°F or 60°C) to kill spores, and use antifungal detergents or additives like tea tree oil for added protection. For sports gear, such as wrestling mats or helmets, wipe surfaces with a disinfectant containing at least 70% isopropyl alcohol after each use. Educate children and teens about the importance of not sharing personal items like socks, hats, or brushes, especially in communal settings like schools or camps.
Comparing household and athletic environments reveals distinct challenges. In homes, the focus should be on isolating infected items—for example, using separate laundry baskets and avoiding shared bedding until the infection clears. In contrast, athletic settings require systemic solutions, such as mandatory gear disinfection protocols and regular inspections for fungal outbreaks. Both contexts demand vigilance, but the scale and nature of shared items dictate the strategy.
Ultimately, breaking the chain of spore transmission through shared items is a matter of awareness and action. By understanding how easily spores cling to fabrics and survive, individuals can adopt simple yet effective habits to protect themselves and others. Whether at home, school, or the gym, treating shared items as potential carriers of ringworm spores is a small but critical step in preventing outbreaks.
Customizing Spores in Civilization Age: Possibilities and Limitations Explored
You may want to see also

Animal Transmission: Pets like cats and dogs can carry spores and infect humans through contact
Pets, particularly cats and dogs, can silently harbor ringworm spores, becoming unsuspecting carriers that transmit the fungus to humans through direct contact. Unlike many infections, ringworm doesn’t require visible symptoms in the animal to spread. Even asymptomatic pets can shed spores from their fur, skin, or claws, making routine interactions like petting, grooming, or sharing bedding potential risk factors. This stealthy transmission underscores the importance of vigilance, especially in households with young children, elderly individuals, or immunocompromised family members who are more susceptible to infection.
To minimize the risk of animal-to-human transmission, proactive measures are essential. Regular veterinary check-ups can identify fungal infections early, even if your pet shows no signs of illness. Vacuuming and disinfecting pet areas frequently, using antifungal cleaners, can reduce spore accumulation in the environment. Washing hands thoroughly after handling pets, particularly before eating or touching the face, is a simple yet effective preventive step. For high-risk households, keeping pets out of shared sleeping areas and laundering their bedding separately can further limit exposure.
Comparing the transmission dynamics between cats and dogs reveals subtle differences. Cats, especially kittens and long-haired breeds, are more likely to carry ringworm due to their grooming habits and close contact with contaminated surfaces. Dogs, on the other hand, often contract the fungus through soil or infected animals, making outdoor exposure a significant risk factor. Understanding these species-specific patterns can help pet owners tailor their preventive strategies, such as limiting a dog’s access to potentially contaminated areas or regularly brushing a cat’s coat to remove loose spores.
Persuasively, the financial and emotional costs of untreated ringworm in pets and subsequent human infection far outweigh the effort of preventive care. Treating a ringworm outbreak in a household can involve costly antifungal medications, veterinary bills, and missed workdays. By contrast, investing in routine pet care, environmental hygiene, and personal precautions is a minor commitment that yields significant long-term benefits. Prioritizing prevention not only safeguards human health but also ensures the well-being of beloved pets, fostering a healthier, happier home environment.
Does Sarcina Lutea Form Spores? Unraveling the Mystery of Its Reproduction
You may want to see also
Explore related products

Soil Exposure: Prolonged contact with soil containing spores can lead to ringworm infection
Ringworm spores, known as arthrospores, are remarkably resilient, capable of surviving in soil for months to years under favorable conditions. This longevity makes soil a persistent reservoir for infection, particularly in areas frequented by humans and animals. Gardens, playgrounds, and farms are common culprits, as the spores thrive in warm, moist environments often found in these settings. Prolonged contact with contaminated soil—whether through gardening, playing, or working—increases the risk of spores adhering to skin, leading to infection. Even brief exposure can be problematic if the skin is compromised, such as through cuts or scratches, which provide an entry point for the spores.
To minimize risk, adopt protective measures during soil-related activities. Wear gloves when gardening or handling soil, especially if you have open wounds or sensitive skin. For children, who are more susceptible due to frequent outdoor play, ensure they wash hands thoroughly after playing in dirt or sandboxes. Regularly inspect outdoor areas for signs of fungal growth, such as discolored patches in soil or plants, which may indicate spore presence. If you suspect contamination, avoid the area or treat it with fungicides labeled for soil use. These precautions are particularly critical for individuals with weakened immune systems, as they face higher infection risks.
Comparatively, soil exposure differs from other transmission routes, such as direct contact with infected animals or humans, due to its passive nature. While petting an infected dog requires immediate contact, soil exposure is often incidental and cumulative. For instance, a gardener may not notice repeated exposure over weeks until symptoms appear. This underscores the importance of consistent preventive practices, unlike one-time interventions like treating a pet. Additionally, soil contamination can spread indirectly—shoes or tools carrying spores from one area to another—amplifying the risk beyond the initial source.
A practical takeaway is to treat soil exposure as a long-term hazard, not a single event. After activities involving soil, clean tools, clothing, and footwear to prevent spore transfer. For high-risk areas, consider using raised garden beds or barriers to reduce direct soil contact. If infection occurs, antifungal treatments like clotrimazole or terbinafine are typically effective, but consult a healthcare provider for proper diagnosis and dosage, especially for children or severe cases. By understanding the unique risks of soil exposure, individuals can enjoy outdoor activities while safeguarding against ringworm.
Hot Water vs. Ringworm Spores: Effective Treatment or Myth?
You may want to see also

Environmental Survival: Spores remain viable in environments for months, increasing indirect transmission risk
Ringworm spores, known as arthrospores, are remarkably resilient, capable of surviving in various environments for months. This longevity significantly amplifies the risk of indirect transmission, as contaminated surfaces, objects, or soil become silent carriers of infection. Unlike many pathogens that degrade quickly outside their host, ringworm spores maintain their viability, waiting for an opportunity to infect a new host. This persistence underscores the importance of understanding their environmental survival to mitigate spread effectively.
Consider the practical implications of this survival capability. A single infected pet shedding spores into a carpet can contaminate the area for weeks, posing a risk to anyone who comes into contact with it. Similarly, shared gym equipment, shower floors, or even wrestling mats can harbor spores long after the infected individual has left. For instance, studies have shown that ringworm spores can remain viable on comb surfaces for up to 18 months under favorable conditions. This highlights the need for rigorous cleaning protocols, particularly in high-traffic areas where indirect transmission is most likely.
To combat this risk, proactive measures are essential. Regular cleaning with antifungal agents is critical, especially in environments frequented by children, athletes, or pets, who are more susceptible to infection. For surfaces, a solution of chlorine bleach (1:10 dilution) or a commercial disinfectant effective against fungi should be used. Vacuuming carpets and upholstery can help remove spores, but the vacuum bag must be disposed of immediately to prevent recontamination. In agricultural settings, contaminated soil should be treated with fungicides or left fallow to reduce spore viability.
Age and immunity play a role in vulnerability to indirect transmission. Young children, the elderly, and immunocompromised individuals are at higher risk due to weaker immune responses. For example, a daycare center with a single infected child can become a hotspot if toys, play mats, or furniture are not sanitized regularly. Parents and caregivers should be vigilant about hygiene, ensuring hands are washed frequently and shared items are cleaned thoroughly. Pets, particularly cats and dogs, should be checked regularly for ringworm and treated promptly to prevent environmental contamination.
In conclusion, the environmental survival of ringworm spores demands a strategic approach to prevention. By understanding their resilience and implementing targeted cleaning practices, the risk of indirect transmission can be significantly reduced. Whether in homes, schools, gyms, or farms, awareness and action are key to breaking the chain of infection. This knowledge empowers individuals and communities to protect themselves and others from this persistent and pervasive pathogen.
Do All Animals Produce Diploid Spores? Unraveling the Biology
You may want to see also
Frequently asked questions
Ringworm spores (fungal spores) spread through direct skin-to-skin contact with an infected person or by touching contaminated surfaces like clothing, towels, or sports equipment.
Ringworm spores do not typically spread through the air. They require direct contact with infected skin, animals, or contaminated items to transmit.
Yes, ringworm spores can spread from infected pets (like cats or dogs) to humans through direct contact with the animal’s skin, fur, or contaminated grooming tools.