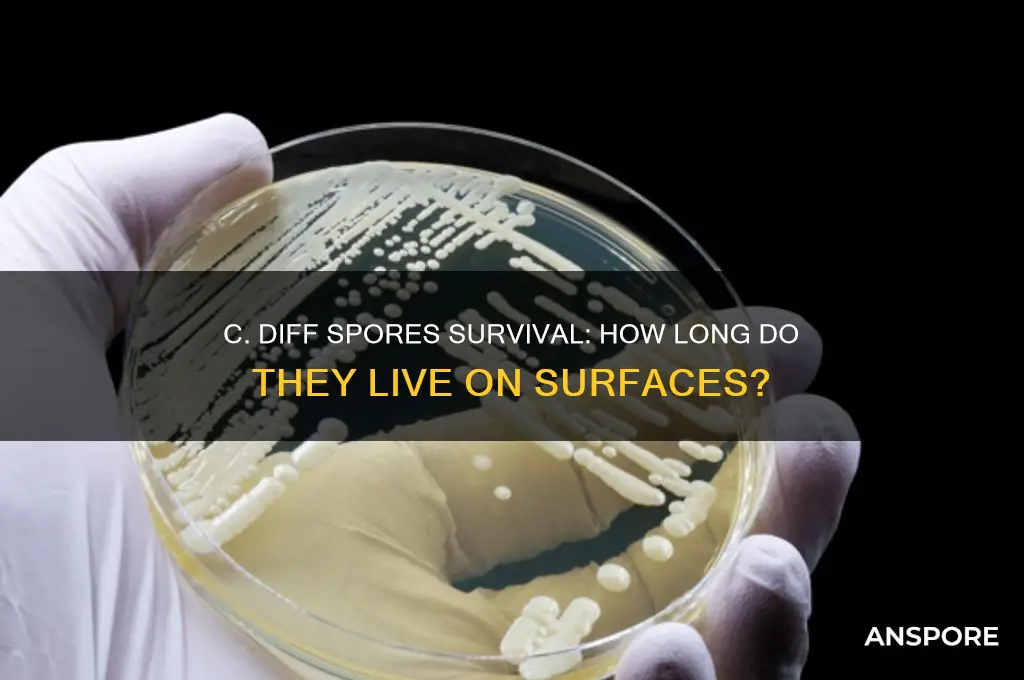
Clostridioides difficile (C. diff) is a spore-forming bacterium that can cause severe intestinal infections, particularly in healthcare settings. One of the most concerning aspects of C. diff is the longevity of its spores, which are highly resistant to environmental conditions and many common disinfectants. C. diff spores can survive on surfaces for extended periods, ranging from weeks to months, depending on factors such as temperature, humidity, and the type of surface material. This resilience makes them a significant challenge in infection control, as contaminated surfaces can serve as a reservoir for transmission even after patients with C. diff have been discharged. Understanding how long C. diff spores live on surfaces is crucial for implementing effective disinfection protocols and reducing the risk of healthcare-associated infections.
| Characteristics | Values |
|---|---|
| Survival Time on Surfaces | Up to 5 months or more (varies based on environmental conditions) |
| Resistance to Disinfectants | Highly resistant to alcohol-based cleaners |
| Effective Disinfectants | Sporocidals like chlorine bleach (5,000–10,000 ppm) or hydrogen peroxide |
| Optimal Survival Conditions | Dry, room temperature environments |
| Impact of Humidity | Lower humidity prolongs spore survival |
| Temperature Tolerance | Survives well at room temperature; reduced survival at extreme temperatures |
| Surface Type Influence | Longer survival on non-porous surfaces (e.g., plastic, metal) |
| UV Light Effect | Minimal impact on spore survival |
| Cross-Contamination Risk | High; spores can easily transfer via hands, equipment, or clothing |
| Decontamination Challenge | Requires thorough cleaning and disinfection of entire environment |
| Relevance to Healthcare Settings | Major concern due to prolonged survival and infection risk |
Explore related products
$12.78 $14.99
What You'll Learn
- Surface Type Impact: Different materials affect spore survival time, from hours to months
- Environmental Factors: Humidity, temperature, and light influence spore longevity on surfaces
- Cleaning Efficacy: Proper disinfection methods reduce spore survival, ensuring surface safety
- Survival Duration: C. diff spores can persist on surfaces for up to 5 months
- Risk Reduction: Frequent cleaning and hand hygiene minimize spore transmission risks

Surface Type Impact: Different materials affect spore survival time, from hours to months
C. difficile spores, notorious for their resilience, exhibit dramatically different survival times depending on the surface they contaminate. This variability isn't random; it's deeply tied to the physical and chemical properties of the material itself.
Consider stainless steel, a common surface in healthcare settings. Its smooth, non-porous nature makes it inhospitable to spore attachment. Studies show C. diff spores can survive here for up to 5 months, a testament to their tenacity but also highlighting the importance of rigorous disinfection protocols. In contrast, porous surfaces like fabric or wood provide crevices and organic matter that spores can cling to, potentially extending their survival time even further.
The lesson is clear: surface type dictates disinfection strategy. For high-touch, non-porous surfaces like doorknobs or bed rails, frequent cleaning with chlorine-based disinfectants (at least 1,000 ppm) is crucial. Porous materials, however, may require disposal or specialized cleaning methods like steam sterilization to ensure complete eradication.
This material-specific approach isn't just theoretical; it's a practical necessity in infection control. A 2018 study found that C. diff spores survived significantly longer on hospital privacy curtains (a porous fabric) compared to plastic surfaces, underscoring the need for tailored cleaning protocols in healthcare environments.
Understanding Isolated Spore Syringes: A Beginner's Guide to Mushroom Cultivation
You may want to see also

Environmental Factors: Humidity, temperature, and light influence spore longevity on surfaces
C. difficile spores are notoriously resilient, capable of surviving on surfaces for weeks to months. However, their longevity isn’t fixed—it’s heavily influenced by environmental factors like humidity, temperature, and light. Understanding these factors is crucial for implementing effective disinfection strategies in healthcare settings and beyond.
Humidity plays a dual role in spore survival. High humidity levels (above 60%) can extend the life of C. diff spores by providing the moisture needed for metabolic activity. In contrast, low humidity environments (below 40%) can desiccate spores, potentially reducing their viability over time. However, desiccation-resistant spores may still persist, making humidity control alone insufficient for eradication. Practical tip: Maintain indoor humidity between 40–60% to minimize spore survival while avoiding conditions that promote mold growth.
Temperature acts as a critical regulator of spore longevity. C. diff spores thrive in moderate temperatures (20–30°C or 68–86°F), which mimic the human body’s environment. At extremes—below 4°C (39°F) or above 50°C (122°F)—spore metabolism slows, reducing their ability to germinate. However, spores can remain dormant and viable even under these conditions, reactivating when temperatures return to optimal levels. Caution: Freezing or refrigerating surfaces won’t kill spores; it merely pauses their activity. For disinfection, use heat (e.g., steam cleaning at 71°C or 160°F) to effectively destroy spores.
Light exposure, particularly ultraviolet (UV) light, is a powerful tool against C. diff spores. UV-C light (200–280 nm) damages spore DNA, rendering them unable to replicate. Studies show that 10–30 minutes of UV-C exposure can reduce spore viability by 99.9%. However, effectiveness depends on intensity, distance, and surface material. For example, porous surfaces may require longer exposure times. Practical application: Incorporate UV-C disinfection devices in high-risk areas like hospital rooms, ensuring all surfaces are directly exposed to the light source.
Combining these factors can enhance disinfection efforts. For instance, using heat in conjunction with low humidity can accelerate spore desiccation, while UV light can target residual spores. However, no single factor guarantees complete eradication. A multi-pronged approach—controlling humidity, applying heat, and utilizing UV light—is essential for minimizing spore survival on surfaces. Takeaway: Environmental manipulation is a strategic weapon against C. diff, but consistency and thoroughness are key to success.
Effective Milky Spore Powder Application: A Guide to Grub Control
You may want to see also

Cleaning Efficacy: Proper disinfection methods reduce spore survival, ensuring surface safety
C. difficile spores can survive on surfaces for months, posing a persistent threat in healthcare settings and beyond. Their resilience to standard cleaning agents underscores the critical need for targeted disinfection methods. Proper cleaning efficacy not only reduces spore survival but also ensures surface safety, breaking the chain of infection.
Effective disinfection begins with selecting the right agent. Sodium hypochlorite (bleach) solutions, specifically 1,000–5,000 ppm (parts per million) of available chlorine, are proven to kill C. diff spores. For example, a 1:10 dilution of household bleach (5–6% sodium hypochlorite) with water achieves the necessary concentration. Apply the solution to surfaces, allowing a 10-minute contact time before wiping. This method is particularly vital in high-risk areas like hospitals, where spores can spread via contaminated equipment or hands.
However, bleach isn’t the only option. Sporicidal disinfectants registered by the EPA, such as those containing accelerated hydrogen peroxide or peracetic acid, are equally effective. These alternatives are useful in settings where bleach’s corrosive nature or odor is a concern. Regardless of the agent, proper application is key. Surfaces must be thoroughly cleaned of organic matter before disinfection, as debris can shield spores from the disinfectant.
A comparative analysis reveals that manual cleaning alone removes only 40–60% of pathogens, leaving spores intact. Automated systems, such as UV-C light or hydrogen peroxide vapor, offer higher efficacy but are supplementary to chemical disinfection. For instance, UV-C light reduces spore counts by 99.9% but requires direct exposure, making it less practical for complex surfaces. Combining methods—manual cleaning followed by targeted disinfection—maximizes spore eradication.
Practical tips enhance cleaning efficacy. Use disposable microfiber cloths or wipes to avoid cross-contamination, and change cleaning solutions frequently to prevent dilution. Train staff on proper techniques, emphasizing contact time and surface coverage. In healthcare, terminal cleaning protocols after C. diff patient discharge are non-negotiable. For home settings, focus on high-touch areas like doorknobs, light switches, and countertops, especially if a household member is infected.
In conclusion, proper disinfection methods are the linchpin of surface safety against C. diff spores. By choosing effective agents, ensuring thorough application, and adopting complementary strategies, we can significantly reduce spore survival. This proactive approach not only protects vulnerable populations but also mitigates the broader risk of infection.
Mastering Spore Syringe Creation: A Step-by-Step DIY Guide
You may want to see also
Explore related products

Survival Duration: C. diff spores can persist on surfaces for up to 5 months
C. diff spores are remarkably resilient, capable of surviving on surfaces for up to 5 months under the right conditions. This longevity is a critical factor in their ability to cause persistent infections, particularly in healthcare settings. Unlike many other pathogens, C. diff spores are resistant to routine cleaning agents, including alcohol-based sanitizers, which are ineffective against them. This resistance underscores the need for targeted disinfection strategies to break the chain of transmission.
To combat the persistence of C. diff spores, healthcare facilities must adopt specific cleaning protocols. Sodium hypochlorite solutions (bleach) with a concentration of 1,000–5,000 ppm are recommended for surface disinfection. For example, a 1:10 dilution of household bleach (5% sodium hypochlorite) in water creates an effective solution. Surfaces should be pre-cleaned to remove organic matter before disinfection, as debris can shield spores from the disinfectant. This two-step process—cleaning followed by disinfection—is essential for reducing spore viability.
The survival duration of C. diff spores highlights the importance of environmental hygiene in infection control. In healthcare settings, high-touch surfaces like bed rails, doorknobs, and light switches are frequent reservoirs for spores. Regular audits of cleaning practices and staff training on proper disinfection techniques can significantly reduce contamination. For instance, using color-coded microfiber cloths for different areas prevents cross-contamination, a simple yet effective measure to minimize spore spread.
Comparatively, the 5-month survival time of C. diff spores dwarfs that of many other pathogens, such as influenza viruses, which typically survive on surfaces for only a few hours to days. This extended viability necessitates a more rigorous approach to surface hygiene, particularly in environments with vulnerable populations, such as hospitals and long-term care facilities. Unlike short-lived pathogens, C. diff requires sustained vigilance and proactive measures to prevent outbreaks.
Practically, individuals can reduce the risk of C. diff transmission by adopting simple habits. At home, regularly disinfect frequently touched surfaces with bleach-based cleaners, especially if someone in the household has had a C. diff infection. Hand hygiene is equally critical; wash hands with soap and water, as alcohol-based hand sanitizers do not kill C. diff spores. These steps, though basic, are powerful tools in preventing the spread of this persistent pathogen.
Mastering Spore Print Storage: Essential Tips for Long-Term Preservation
You may want to see also

Risk Reduction: Frequent cleaning and hand hygiene minimize spore transmission risks
C. difficile spores can survive on surfaces for months, posing a persistent threat in healthcare settings and beyond. Their resilience to standard cleaning agents and environmental conditions makes them a formidable challenge for infection control. However, the risk of transmission is not insurmountable. By implementing rigorous cleaning protocols and emphasizing hand hygiene, the spread of these spores can be significantly reduced.
Analytical Perspective:
The longevity of C. diff spores on surfaces—ranging from weeks to months—highlights the critical need for targeted disinfection strategies. Unlike vegetative bacteria, spores are encased in a protective layer that resists alcohol-based sanitizers, necessitating the use of spore-specific agents like chlorine-based cleaners (e.g., 1,000–5,000 ppm sodium hypochlorite). Studies show that surfaces in high-touch areas, such as bed rails and doorknobs, are frequent reservoirs for spores. A systematic approach to cleaning, focusing on these areas, disrupts the chain of transmission. For instance, a 2019 study in *Infection Control & Hospital Epidemiology* found that daily cleaning with chlorine-based solutions reduced surface contamination by 80% in healthcare facilities.
Instructive Approach:
To minimize spore transmission, follow these steps:
- Clean High-Touch Surfaces Daily: Use EPA-registered disinfectants effective against C. diff spores. Dilute bleach solutions (1:10 ratio of bleach to water) for non-porous surfaces, ensuring contact for at least 10 minutes.
- Adopt a Two-Step Process: Pre-clean surfaces to remove organic matter before applying the disinfectant, as debris can shield spores from the active agent.
- Train Staff and Caregivers: Ensure all personnel understand the importance of using the correct concentration and contact time for disinfectants.
- Monitor Compliance: Implement audits or checklists to verify cleaning protocols are followed consistently.
Persuasive Argument:
Hand hygiene is the cornerstone of infection prevention, yet it is often overlooked in non-healthcare settings. Alcohol-based hand sanitizers, while effective against most pathogens, are ineffective against C. diff spores. Instead, soap and water should be used to physically remove spores from hands. For healthcare workers, this is particularly critical after contact with patients or contaminated surfaces. A study in *The Lancet* demonstrated that proper handwashing reduced C. diff transmission by 40% in long-term care facilities. By prioritizing this simple yet powerful practice, individuals and institutions can dramatically lower the risk of spore dissemination.
Comparative Insight:
While UV-C light and hydrogen peroxide vapor systems are emerging as adjunctive tools for environmental decontamination, they are not a substitute for manual cleaning and hand hygiene. These technologies are costly and time-consuming, making them impractical for routine use in most settings. In contrast, consistent cleaning with chlorine-based agents and proper handwashing offer a cost-effective, scalable solution. For example, a hospital in the UK reduced C. diff infections by 70% after implementing a combination of enhanced cleaning protocols and staff education on hand hygiene.
Practical Tips:
- For Healthcare Settings: Use disposable cleaning cloths to avoid cross-contamination and ensure each surface is wiped with a fresh cloth.
- For Home Care: Designate separate cleaning tools (e.g., mops, brushes) for areas where a C. diff-positive individual resides.
- For All Environments: Encourage the use of gloves during cleaning, followed by handwashing with soap and water to prevent spore transfer to the face or other surfaces.
By integrating frequent cleaning and meticulous hand hygiene into daily routines, the risk of C. diff spore transmission can be minimized, protecting vulnerable populations and reducing the burden of this stubborn pathogen.
Extending Mushroom Spores Lifespan: Fridge Storage Tips and Duration
You may want to see also
Frequently asked questions
C. diff spores can survive on surfaces for weeks to months, depending on environmental conditions such as temperature, humidity, and the type of surface.
Regular household cleaners are not effective against C. diff spores. Only disinfectants containing chlorine bleach (sodium hypochlorite) or sporicidal agents are proven to kill them.
C. diff spores are highly resilient and do not die naturally over time without proper disinfection. They remain viable and infectious until effectively cleaned or treated.