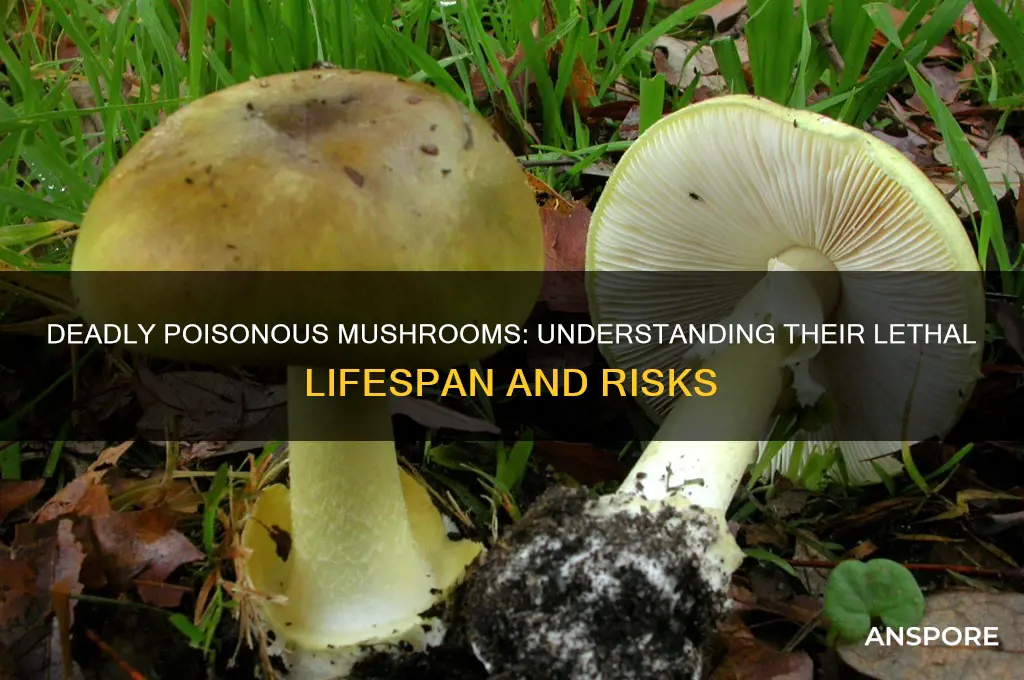
The question of how long it takes for poison mushrooms to die off or decompose is a complex one, influenced by various factors such as mushroom species, environmental conditions, and the presence of decomposers. Poisonous mushrooms, like other fungi, play a crucial role in ecosystems by breaking down organic matter, but their toxic properties can pose risks to humans and animals. The decomposition process typically involves the breakdown of the mushroom's cellular structure by bacteria, fungi, and other microorganisms, which can take anywhere from a few days to several weeks, depending on factors like temperature, humidity, and the availability of nutrients. Understanding the lifespan and decomposition of poison mushrooms is essential for both ecological research and public safety, as it helps in identifying potential hazards and mitigating risks associated with accidental ingestion.
Explore related products
What You'll Learn
- Symptoms of Poisoning: Nausea, vomiting, cramps, diarrhea, hallucinations, organ failure, and potential death
- Toxicity Levels: Amount consumed, mushroom species, and individual tolerance affect severity
- Time to Onset: Symptoms appear 6–24 hours post-ingestion, depending on mushroom type
- Medical Treatment: Immediate care, gastric lavage, activated charcoal, and supportive therapy are crucial
- Fatality Timeline: Death can occur within 24–72 hours without prompt medical intervention

Symptoms of Poisoning: Nausea, vomiting, cramps, diarrhea, hallucinations, organ failure, and potential death
Consuming poisonous mushrooms can lead to severe and potentially life-threatening symptoms, often progressing rapidly depending on the type of mushroom ingested. The onset of symptoms typically begins within 6 to 24 hours after consumption, though some toxic species may cause delayed reactions. The initial symptoms usually include nausea and vomiting, which are the body’s immediate attempts to expel the toxin. These symptoms are often accompanied by abdominal cramps and diarrhea, as the gastrointestinal system reacts to the poison. It is crucial to seek medical attention immediately if these symptoms occur after consuming wild mushrooms, as they can escalate quickly.
As the poisoning progresses, more severe symptoms may develop, including hallucinations in cases of ingestion of hallucinogenic or psychoactive mushrooms. These hallucinations can be distressing and disorienting, often leading to confusion and panic. However, even more dangerous are the toxins found in species like the Death Cap (*Amanita phalloides*) or Destroying Angel (*Amanita bisporigera*), which can cause organ failure. These toxins specifically target the liver and kidneys, leading to symptoms such as jaundice, dark urine, and a significant drop in blood pressure. Organ failure is a critical condition that requires immediate medical intervention, as it can lead to potential death within 24 to 72 hours if left untreated.
The timeline of death from poisonous mushrooms varies depending on the species and the amount consumed. For instance, toxins like amatoxins, found in the Death Cap, can cause fatal liver failure within 5 to 7 days if not treated promptly. In contrast, mushrooms containing orellanine, such as the Fool’s Mushroom (*Amanita verna*), may cause delayed kidney failure, with symptoms appearing after 3 to 4 days and potentially leading to death within 1 to 2 weeks. Early treatment, including gastric decontamination, activated charcoal, and supportive care, can significantly improve survival rates, but the window for effective intervention is narrow.
It is essential to recognize that not all poisonous mushrooms cause immediate symptoms, and some may mimic the appearance of edible varieties. For example, the Galerina mushroom, often mistaken for edible species, contains amatoxins and can cause severe poisoning. If there is any doubt about the safety of a mushroom, it should not be consumed. In cases of suspected poisoning, contacting a poison control center or healthcare provider immediately is vital. Providing details such as the time of ingestion, symptoms experienced, and, if possible, a sample of the mushroom can aid in diagnosis and treatment.
Preventing mushroom poisoning begins with proper identification and avoidance of wild mushrooms unless one is an experienced forager. Educating oneself about common toxic species in the region and their look-alikes can save lives. If poisoning occurs, the focus should be on managing symptoms and preventing complications. While some cases may resolve with minimal intervention, others require intensive medical treatment, including liver transplants in severe amatoxin poisoning. Awareness and swift action are key to reducing the risk of potential death from poisonous mushrooms.
Perfectly Grilled Portobello Mushrooms: Timing Tips for Juicy Results
You may want to see also

Toxicity Levels: Amount consumed, mushroom species, and individual tolerance affect severity
The toxicity levels of poisonous mushrooms can vary widely, and several factors play a critical role in determining the severity of poisoning. Amount consumed is a primary factor; ingesting a small piece of a highly toxic mushroom may cause mild symptoms, while consuming a larger quantity can lead to severe, life-threatening conditions. For instance, mushrooms like the Death Cap (*Amanita phalloides*) contain potent toxins that can cause liver and kidney failure, with symptoms often delayed by 6–24 hours. Even a single mushroom of this species can be fatal if not treated promptly. Conversely, less toxic species may require a larger amount to produce significant harm, but this does not diminish the risk, as misidentification can easily lead to accidental poisoning.
Mushroom species is another critical determinant of toxicity levels. Different mushrooms contain distinct toxins, each affecting the body in unique ways. For example, the toxins in the Death Cap and Destroying Angel (*Amanita ocreata*) target the liver, while the toxins in the False Morel (*Gyromitra esculenta*) affect the nervous system and can cause seizures. Some mushrooms, like the Inky Cap (*Coprinus atramentarius*), cause toxicity only when consumed with alcohol, leading to symptoms like nausea, vomiting, and rapid heartbeat. Understanding the specific toxins present in a mushroom species is essential for predicting the onset, severity, and type of symptoms, as well as the appropriate medical response.
Individual tolerance also significantly influences how a person reacts to mushroom poisoning. Factors such as age, weight, overall health, and pre-existing medical conditions can affect the body's ability to process and eliminate toxins. Children and the elderly are generally more susceptible to severe poisoning due to their lower body mass and weaker immune systems. Additionally, individuals with compromised liver or kidney function may experience more severe symptoms, as these organs are often the primary targets of mushroom toxins. Even genetic differences in metabolism can play a role, as some people may break down toxins more slowly or quickly than others, altering the severity and duration of symptoms.
The interplay of these factors makes mushroom poisoning highly unpredictable. For instance, a healthy adult might consume a small amount of a moderately toxic mushroom and experience only mild gastrointestinal symptoms, while a child ingesting the same amount could face life-threatening complications. Similarly, two people consuming the same species and quantity of mushroom may exhibit vastly different reactions due to variations in tolerance. This complexity underscores the importance of immediate medical attention in any suspected case of mushroom poisoning, as early intervention can mitigate the effects of toxins and improve outcomes.
In summary, the toxicity levels of poisonous mushrooms are influenced by the amount consumed, mushroom species, and individual tolerance. These factors collectively determine the severity of symptoms and the potential for fatal outcomes. Accurate identification of the mushroom species involved is crucial for effective treatment, as different toxins require specific antidotes or supportive care. Public awareness about the risks of wild mushroom consumption and the ability to recognize common toxic species can help reduce the incidence of poisoning. When in doubt, it is always safer to avoid consuming wild mushrooms altogether and consult experts or medical professionals promptly if exposure occurs.
Dehydrating Oyster Mushrooms: Optimal Time for Perfect Preservation
You may want to see also

Time to Onset: Symptoms appear 6–24 hours post-ingestion, depending on mushroom type
The time it takes for symptoms to appear after ingesting poisonous mushrooms can vary significantly, typically ranging from 6 to 24 hours post-ingestion, depending on the type of mushroom involved. This delay is due to the time required for the toxins to be absorbed by the digestive system and to exert their effects on the body. For instance, mushrooms containing amatoxins, such as the Death Cap (*Amanita phalloides*), often have a longer latency period, with symptoms appearing anywhere from 6 to 12 hours after consumption. This delayed onset can be particularly dangerous, as it may lead individuals to underestimate the severity of the poisoning.
In contrast, mushrooms containing muscarine or psilocybin may cause symptoms to appear more rapidly, often within 1 to 6 hours. Muscarine-containing mushrooms, like certain species of *Clitocybe*, can induce symptoms such as sweating, salivation, and gastrointestinal distress within a few hours. Psilocybin mushrooms, while not typically lethal, can cause hallucinations and altered mental states within a similar timeframe. Understanding these variations in onset time is crucial for identifying the type of poisoning and seeking appropriate medical intervention.
The 6–24 hour window is a critical period for monitoring individuals who may have ingested poisonous mushrooms. During this time, symptoms such as nausea, vomiting, abdominal pain, diarrhea, and dehydration may manifest. In cases of severe poisoning, particularly with amatoxin-containing mushrooms, symptoms may initially subside after 24–48 hours, giving a false sense of recovery. However, this is often followed by a second, more severe phase of liver and kidney failure, which can be fatal if untreated. Recognizing the initial symptoms within the 6–24 hour onset period is essential for prompt medical treatment.
It is important to note that the exact time to onset can also be influenced by factors such as the amount of mushroom ingested, the individual's overall health, and whether the mushrooms were consumed with food or on an empty stomach. For example, eating a large quantity of toxic mushrooms on an empty stomach may accelerate the onset of symptoms, while consuming them with a meal could delay it slightly. Regardless of these variables, the 6–24 hour range remains a general guideline for most cases of mushroom poisoning.
If poisoning is suspected, immediate medical attention is crucial, even if symptoms have not yet appeared. Contacting a poison control center or healthcare provider can provide guidance on next steps, which may include inducing vomiting, administering activated charcoal, or seeking emergency care. The latency period of 6–24 hours underscores the importance of acting quickly, as delayed treatment can lead to severe complications or death, especially with highly toxic mushroom species. Always err on the side of caution and avoid consuming wild mushrooms unless they have been positively identified by an expert.
Perfectly Cooked Morel Mushrooms: Butter Sautéing Time Guide
You may want to see also
Explore related products

Medical Treatment: Immediate care, gastric lavage, activated charcoal, and supportive therapy are crucial
When dealing with poisoning from poisonous mushrooms, immediate medical care is paramount to prevent severe complications or fatalities. Time is of the essence, as the toxins in certain mushrooms can rapidly cause organ damage. Upon suspicion of ingestion, the affected individual should be rushed to the nearest emergency department. Healthcare providers will first stabilize the patient, ensuring airway, breathing, and circulation are intact. Initial assessments may include blood tests, imaging, and toxicology screenings to identify the type and extent of poisoning. Quick intervention significantly improves the prognosis, as delays can lead to irreversible damage or death within hours to days, depending on the mushroom species and amount consumed.
Gastric lavage, also known as stomach pumping, is a critical procedure performed in the early stages of treatment. This process involves flushing the stomach with a saline solution to remove any remaining mushroom fragments and toxins. It is most effective when done within 1-2 hours of ingestion but can still be beneficial up to 6 hours afterward. Gastric lavage reduces the absorption of toxins into the bloodstream, minimizing their systemic effects. However, it is not suitable for all cases, especially if the patient is experiencing seizures or altered consciousness, as it may pose a risk of aspiration.
Activated charcoal is another essential component of immediate treatment. Administered orally, activated charcoal binds to toxins in the gastrointestinal tract, preventing their absorption into the bloodstream. It is most effective when given within the first hour of ingestion but can still offer benefits up to 4-6 hours afterward. The typical dose for adults is 50-100 grams, while children receive weight-adjusted amounts. Activated charcoal is often used in conjunction with gastric lavage or as a standalone treatment if lavage is not feasible. However, it is ineffective against certain mushroom toxins, such as amatoxins found in the Death Cap mushroom, which require specific antidotes.
Supportive therapy is crucial in managing the symptoms and complications of mushroom poisoning. This includes intravenous fluids to maintain hydration and electrolyte balance, medications to control nausea, vomiting, and seizures, and, in severe cases, dialysis or liver transplantation for organ failure. Continuous monitoring of vital signs, liver and kidney function, and coagulation parameters is essential to detect and address complications early. Supportive care may extend over several days or weeks, depending on the severity of poisoning. For instance, amatoxin poisoning can lead to liver failure within 3-5 days, requiring intensive care and, in some cases, emergency liver transplantation to prevent death.
In conclusion, the medical treatment for poisonous mushroom ingestion hinges on immediate care, gastric lavage, activated charcoal, and supportive therapy. These interventions are time-sensitive and must be initiated as soon as possible to mitigate toxin absorption and manage complications. While the time to death from mushroom poisoning varies depending on the species and amount consumed, prompt and comprehensive treatment can significantly improve survival rates. Public awareness about the dangers of wild mushroom consumption and the importance of seeking immediate medical attention cannot be overstated.
Perfect Air Fryer Stuffed Mushrooms: Quick Cooking Time Guide
You may want to see also

Fatality Timeline: Death can occur within 24–72 hours without prompt medical intervention
The fatality timeline associated with poisoning from certain toxic mushrooms, particularly those containing amatoxins (such as the Death Cap, *Amanita phalloides*), is critically dependent on the speed of medical intervention. Death can occur within 24–72 hours without prompt treatment, making immediate action essential. The toxins in these mushrooms cause severe liver and kidney damage, leading to organ failure if left untreated. Symptoms may not appear for 6–24 hours after ingestion, creating a false sense of security. During this asymptomatic phase, the toxins are already causing irreversible harm, underscoring the urgency of seeking medical help as soon as ingestion is suspected.
Within the first 24 hours, symptoms such as vomiting, diarrhea, abdominal pain, and dehydration typically manifest. These are often mistaken for food poisoning, delaying diagnosis. However, this stage is crucial for survival. Administering activated charcoal to absorb remaining toxins, rehydration, and supportive care can stabilize the patient temporarily. Without intervention, the toxins continue to accumulate in the liver, leading to hepatotoxicity. By the 36–48-hour mark, liver enzymes spike dramatically, and symptoms worsen to include jaundice, confusion, and seizures. At this point, the risk of liver failure becomes imminent, and the patient’s condition deteriorates rapidly.
Between 48–72 hours, the fatality risk peaks. Acute liver failure sets in, causing coagulation disorders, kidney dysfunction, and multi-organ failure. Without a liver transplant or aggressive medical intervention, such as the administration of silibinin (a liver-protective compound) or N-acetylcysteine, death is almost inevitable. The body’s inability to filter toxins and maintain vital functions leads to a cascade of systemic failures. Even with treatment, the mortality rate remains high, emphasizing the importance of early detection and intervention.
It is imperative to seek medical help immediately if mushroom poisoning is suspected, even before symptoms appear. Providing a sample of the ingested mushroom to healthcare providers can aid in identification and treatment. Delaying care by even a few hours can drastically reduce survival chances. Public awareness about the dangers of wild mushroom consumption and the fatality timeline is crucial, as misidentification of toxic species is a common cause of poisoning. Remember: time is of the essence, and acting swiftly can mean the difference between life and death.
Perfect Matsutake Mushroom Cooking Time: Tips for Optimal Flavor
You may want to see also
Frequently asked questions
The time it takes to die from mushroom poisoning varies depending on the species. Symptoms can appear within 20 minutes to 24 hours, and death can occur within hours to several days, depending on the toxin and the amount consumed.
Early signs include nausea, vomiting, diarrhea, abdominal pain, and dizziness. Severe cases may progress to organ failure, seizures, or coma, which are life-threatening and require immediate medical attention.
Yes, survival is possible if treatment is sought immediately. Prompt medical intervention, including supportive care, activated charcoal, and, in some cases, specific antidotes, can significantly improve outcomes.
No, there are no mushrooms that cause instant death. However, some, like the Death Cap (*Amanita phalloides*), contain toxins that can lead to fatal liver and kidney failure within days if untreated.
The toxins from poisonous mushrooms can remain in the body for several days, causing ongoing damage. The duration depends on the toxin type, the amount ingested, and the individual's health and treatment received.