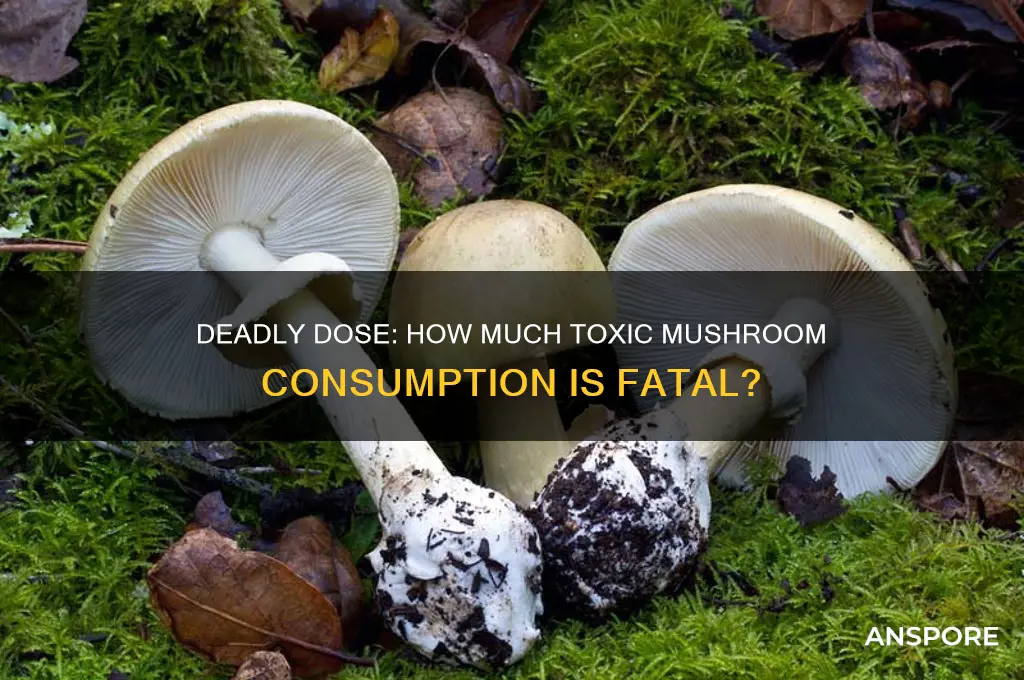
Exploring the question of how much toxic mushroom one can consume before it becomes fatal is a critical yet perilous topic. Toxic mushrooms contain potent toxins like amatoxins, orellanine, or muscarine, which can cause severe symptoms ranging from gastrointestinal distress to organ failure. The lethal dose varies widely depending on the species, the individual's weight, and their overall health. For instance, as little as half a Death Cap mushroom (*Amanita phalloides*) can be deadly for an adult, while other species may require larger quantities to induce fatal poisoning. However, experimenting with toxic mushrooms is extremely dangerous and not recommended, as symptoms may not appear immediately, and there is no safe threshold for consumption. Immediate medical attention is crucial if ingestion is suspected, as prompt treatment can significantly improve survival rates.
Explore related products
What You'll Learn

Lethal Dose Variations by Species
The lethal dose of toxic mushrooms varies dramatically across species, making broad generalizations dangerous. For instance, the Death Cap (*Amanita phalla*) contains amatoxins, and as little as 30 grams (about one mushroom) can be fatal for an adult. In contrast, the Destroying Angel (*Amanita bisporigera*) is even more potent, with a single cap potentially delivering a lethal dose. Conversely, the hallucinogenic Psilocybe species, while not typically deadly, can cause severe psychological distress if consumed in large quantities—usually over 100 grams of fresh mushrooms. This disparity underscores the importance of species-specific knowledge when assessing risk.
Children and pets are at higher risk due to their smaller body mass. For example, a 50-pound child could suffer fatal poisoning from just 10 grams of the Death Cap, while a 10-pound dog might succumb to half that amount. This vulnerability highlights the need for vigilance in environments where toxic mushrooms grow. If ingestion is suspected, immediate medical attention is critical, as symptoms may not appear for 6–24 hours, delaying treatment can be fatal.
Not all toxic mushrooms act the same way. The False Morel (*Gyromitra esculenta*) contains gyromitrin, which converts to monomethylhydrazine in the body, causing severe gastrointestinal and neurological symptoms. A lethal dose is roughly 10–20 milligrams per kilogram of body weight, meaning an adult could be poisoned by consuming 50–100 grams. In comparison, the Galerina marginata, often mistaken for edible mushrooms, contains the same amatoxins as the Death Cap but in smaller concentrations, requiring a larger quantity to be lethal.
Practical tips for safety include avoiding wild mushroom foraging without expert guidance and teaching children and pet owners to recognize common toxic species. If in doubt, consult a mycologist or poison control center. Remember, cooking or drying does not neutralize most mushroom toxins, so proper identification is paramount. Understanding these lethal dose variations by species can save lives and dispel myths about mushroom toxicity.
Can Mushrooms Be Detected at Airports? Security Screening Insights
You may want to see also

Symptoms of Mushroom Poisoning Timeline
The onset of mushroom poisoning symptoms varies widely depending on the species ingested, but a typical timeline can be divided into distinct phases. Immediate symptoms, occurring within 15 minutes to 2 hours, often include gastrointestinal distress such as nausea, vomiting, diarrhea, and abdominal pain. These are common with mushrooms like the *Clitocybe dealbata* (sweating mushroom), which contains muscarine, a toxin that acts rapidly on the body’s cholinergic receptors. This phase is crucial for intervention, as prompt medical attention can mitigate severe outcomes.
Delayed symptoms, appearing 6 to 24 hours after ingestion, are more sinister and indicate poisoning by mushrooms containing amatoxins, such as the *Amanita phalloides* (death cap). These symptoms include dehydration from persistent vomiting and diarrhea, followed by a deceptive "quiet phase" where the individual may feel temporarily better. However, this is a false reprieve, as liver and kidney damage progresses silently. By 24 to 72 hours, late-stage symptoms emerge, including jaundice, seizures, and coma, often leading to organ failure and death without aggressive treatment like liver transplantation.
Children and the elderly are particularly vulnerable due to their lower body mass and weaker immune systems. For instance, a child ingesting even a small fragment of a death cap mushroom (as little as 10–15 grams) can experience life-threatening symptoms within hours. Adults may tolerate slightly larger amounts, but the threshold for toxicity remains low, typically around 30–50 grams of fresh mushroom. The variability in response underscores the importance of immediate medical intervention, regardless of the amount consumed.
Practical tips for suspected poisoning include saving a sample of the mushroom for identification and contacting poison control or emergency services immediately. Inducing vomiting is not recommended unless advised by a professional, as it can worsen certain types of poisoning. Activated charcoal may be administered in a hospital setting to reduce toxin absorption. Understanding this timeline is critical for survival, as early treatment significantly improves outcomes, especially in cases of amatoxin poisoning, where the mortality rate can exceed 50% without intervention.
Mushrooms and Female Pleasure: Unlocking Orgasmic Potential Naturally
You may want to see also

Common Deadly Mushroom Types Overview
The amount of toxic mushroom one can consume before dying varies drastically by species, with some requiring as little as half a cap to induce fatal poisoning. Among the most notorious is the Death Cap (*Amanita phalloides*), responsible for 90% of mushroom-related fatalities. Ingesting just 50 grams (roughly one mushroom) can be lethal for an adult due to its potent hepatotoxins, which cause liver failure within 24–48 hours. Children are at higher risk, as even smaller quantities can prove deadly. Symptoms like vomiting and diarrhea appear 6–24 hours post-ingestion, often followed by a deceptive "recovery" phase before organ collapse.
Contrastingly, the Destroying Angel (*Amanita bisporigera*) contains amatoxins similar to the Death Cap but acts faster, with symptoms appearing within 5–24 hours. A single mushroom contains enough toxin to kill an adult, making it one of the most lethal fungi in North America. Unlike the Death Cap, its symptoms progress rapidly to kidney and liver failure without the delayed "recovery" phase. Its pristine white appearance often misleads foragers into mistaking it for edible varieties like the button mushroom, underscoring the importance of expert identification.
The Fool’s Mushroom (*Amanita verna*) is another deceptively innocuous species, resembling edible mushrooms like the Meadow Mushroom. Its toxins target the liver and kidneys, with as little as 10–20 grams (half a cap) sufficient to cause death in adults. Symptoms emerge 6–24 hours after ingestion, beginning with gastrointestinal distress before escalating to organ failure. Its rarity in certain regions does not diminish its danger, as a single misidentification can be fatal.
For a different mechanism of toxicity, consider the Galerina marginata, often found on decaying wood. Its amatoxins mirror those of the Death Cap, but its smaller size means multiple mushrooms are typically consumed to reach a lethal dose (approximately 10–20 caps). However, its unassuming brown appearance and habitat make it a hidden threat, especially for novice foragers. Symptoms appear within 6–12 hours, progressing to liver failure if untreated.
Practical precautions are paramount: avoid consuming wild mushrooms without expert verification, and educate children about the dangers of ingesting unknown fungi. If poisoning is suspected, seek immediate medical attention, bringing a sample of the mushroom for identification. While antidotes like silibinin exist for amatoxin poisoning, their efficacy depends on prompt administration. Understanding these deadly species and their toxic thresholds is not just academic—it’s a matter of survival.
Freezing Fresh Portabella Mushrooms: A Complete Guide to Preservation
You may want to see also
Explore related products

Factors Affecting Toxicity Levels in Mushrooms
The amount of toxic mushroom one can consume before facing fatal consequences varies dramatically based on species, individual health, and environmental factors. For instance, the Death Cap (*Amanita phalloides*) contains amatoxins, and as little as 50 grams (about half a mushroom) can be lethal for an adult. In contrast, the hallucinogenic Psilocybe species are less physically toxic, but their psychoactive compounds can cause severe psychological distress in sensitive individuals. Understanding these differences is crucial for both foragers and medical professionals.
Species and Toxin Concentration: Not all toxic mushrooms are created equal. The toxicity of a mushroom depends heavily on the type and concentration of its toxins. For example, the Destroying Angel (*Amanita bisporigera*) contains the same amatoxins as the Death Cap but in higher concentrations, making even smaller quantities deadly. Conversely, the False Morel (*Gyromitra esculenta*) contains gyromitrin, which converts to a toxic compound in the body, but thorough cooking can reduce its toxicity significantly. Always identify the species before assuming its danger level.
Individual Factors: Age, weight, and overall health play a critical role in how the body processes mushroom toxins. Children and the elderly are more susceptible to poisoning due to their lower body mass and weaker immune systems. For instance, a child might suffer severe symptoms from ingesting just 10 grams of a toxic mushroom, while an adult might require twice that amount to experience similar effects. Pre-existing liver or kidney conditions can also exacerbate the toxicity, as these organs are often targeted by mushroom poisons.
Preparation and Consumption Method: How a mushroom is prepared can alter its toxicity. Cooking, drying, or boiling can break down certain toxins, such as those in the False Morel, making them safer to eat. However, this is not a universal rule; some toxins, like the amatoxins in the Death Cap, remain stable even after cooking. Additionally, consuming alcohol alongside toxic mushrooms can accelerate the absorption of toxins, increasing the risk of severe poisoning. Always research specific preparation methods for suspected toxic species.
Environmental Conditions: The environment in which a mushroom grows can influence its toxin levels. Factors like soil quality, moisture, and temperature affect the concentration of toxins in mushrooms. For example, the Death Cap tends to accumulate higher levels of amatoxins in nutrient-rich soils. Wild mushrooms growing near polluted areas may also contain harmful chemicals, compounding their toxicity. When foraging, consider the habitat and potential contaminants to assess risk accurately.
Practical Tips for Safety: To minimize the risk of poisoning, follow these guidelines: 1) Never consume a wild mushroom unless you are 100% certain of its identification. 2) Consult a mycologist or use a reliable field guide. 3) Start with a small portion if trying a new species, even if it’s considered edible. 4) Seek immediate medical attention if poisoning is suspected, bringing a sample of the mushroom for identification. Remember, when in doubt, throw it out—the consequences of misidentification can be irreversible.
Mushroom and Okra Combo: A Delicious and Nutritious Pairing?
You may want to see also

Emergency Treatment for Mushroom Poisoning Cases
The amount of toxic mushroom one can consume before facing fatal consequences varies widely depending on the species and individual tolerance. For instance, as little as half a Death Cap (*Amanita phalloides*) mushroom contains enough amatoxins to be lethal for an adult. Conversely, some toxic mushrooms cause severe gastrointestinal distress but are rarely fatal unless consumed in large quantities. Understanding the specific toxin involved is crucial for emergency treatment, as it dictates the urgency and approach to care.
In cases of suspected mushroom poisoning, immediate action is paramount. The first step is to call emergency services or a poison control center, providing details about the mushroom consumed, if known. While waiting for medical help, induce vomiting only if advised by a professional, as some toxins can cause further harm if aspirated. Activated charcoal may be administered by medical personnel to bind toxins in the stomach, but this should never be attempted at home without guidance. For children or the elderly, time is especially critical, as their smaller body mass and slower metabolism can accelerate toxin absorption.
Treatment protocols vary based on the toxin type. Amatoxin poisoning, for example, often requires hospitalization for supportive care, including intravenous fluids, electrolyte monitoring, and, in severe cases, liver transplantation. Muscarinic toxins, found in mushrooms like *Clitocybe dealbata*, may necessitate atropine administration to counteract symptoms like sweating, salivation, and bronchial secretions. Gastrointestinal irritants, such as those in *Chlorophyllum molybdites*, typically resolve with symptomatic treatment, but dehydration from vomiting and diarrhea must be managed aggressively, particularly in young children and the elderly.
Prevention remains the most effective strategy. Educating oneself about local mushroom species and avoiding consumption of wild mushrooms unless positively identified by an expert can eliminate risks. For foragers, carrying a reliable field guide and consulting mycologists can be lifesaving. In emergency situations, however, swift recognition of symptoms—such as abdominal pain, confusion, or jaundice—coupled with immediate medical intervention, can mean the difference between recovery and tragedy.
Can You Eat Baby Portabella Mushroom Stems? A Tasty Guide
You may want to see also
Frequently asked questions
The lethal dose varies by mushroom species and individual tolerance. For example, as little as half a Death Cap mushroom (*Amanita phalloides*) can be fatal to an adult. Always avoid consuming wild mushrooms unless identified by an expert.
No, even a small bite of certain toxic mushrooms, like the Destroying Angel (*Amanita bisporigera*), can cause severe poisoning or death. Never assume any amount is safe without proper identification.
Symptoms can appear within 30 minutes to 24 hours, depending on the mushroom type. Delayed symptoms (6–24 hours) are common with highly toxic species like the Death Cap, making them especially dangerous.
No, cooking does not neutralize most mushroom toxins. Toxins like amatoxins (found in Death Caps) remain deadly even after preparation. Always avoid consuming unidentified mushrooms.











































