Mushrooms, while often celebrated for their culinary and medicinal uses, can also harbor deadly toxins that act swiftly and silently. Certain species, such as the Death Cap (*Amanita phalloides*) and the Destroying Angel (*Amanita bisporigera*), contain potent toxins like amatoxins, which can cause severe liver and kidney damage within hours of ingestion. Symptoms may initially appear mild, such as nausea, vomiting, and diarrhea, but can rapidly progress to organ failure and death within 24 to 48 hours if left untreated. The speed at which these toxins act, combined with the difficulty in distinguishing toxic mushrooms from edible ones, makes accidental poisoning a grave and immediate threat. Understanding the risks and seeking prompt medical attention is crucial, as time is of the essence in preventing a fatal outcome.
| Characteristics | Values |
|---|---|
| Time to Onset of Symptoms | 6-24 hours after ingestion (varies by species) |
| Deadliest Species | Death Cap (Amanita phalloides), Destroying Angel (Amanita bisporigera), Fool's Mushroom (Amanita verna) |
| Toxic Compounds | Amatoxins (cyclic octapeptides), Orellanine, Muscarine, Ibotenic Acid |
| Fatal Dose | As little as 30g (1 oz) of Death Cap mushrooms for an adult |
| Symptoms | Early: Gastrointestinal (vomiting, diarrhea, abdominal pain); Late: Liver and kidney failure, coma, death |
| Time to Death | 5-10 days after ingestion without treatment; survival possible with early medical intervention |
| Treatment | Gastric lavage, activated charcoal, supportive care, liver transplant in severe cases |
| Survival Rate | 10-50% without treatment; up to 90% with prompt medical care |
| Misidentification Risk | High; toxic species often resemble edible mushrooms (e.g., Death Cap vs. Paddy Straw Mushroom) |
| Geographic Distribution | Toxic species found worldwide, with higher risk in temperate regions |
Explore related products
What You'll Learn
- Deadly Mushroom Species: Identify which mushrooms are most toxic and can cause rapid death
- Symptoms of Poisoning: Recognize early signs of mushroom toxicity before it’s too late
- Time to Fatality: Understand how quickly symptoms escalate to death after ingestion
- Treatment Options: Learn immediate steps to take if poisoned by a deadly mushroom
- Prevention Tips: Avoid accidental poisoning with safe foraging and identification practices

Deadly Mushroom Species: Identify which mushrooms are most toxic and can cause rapid death
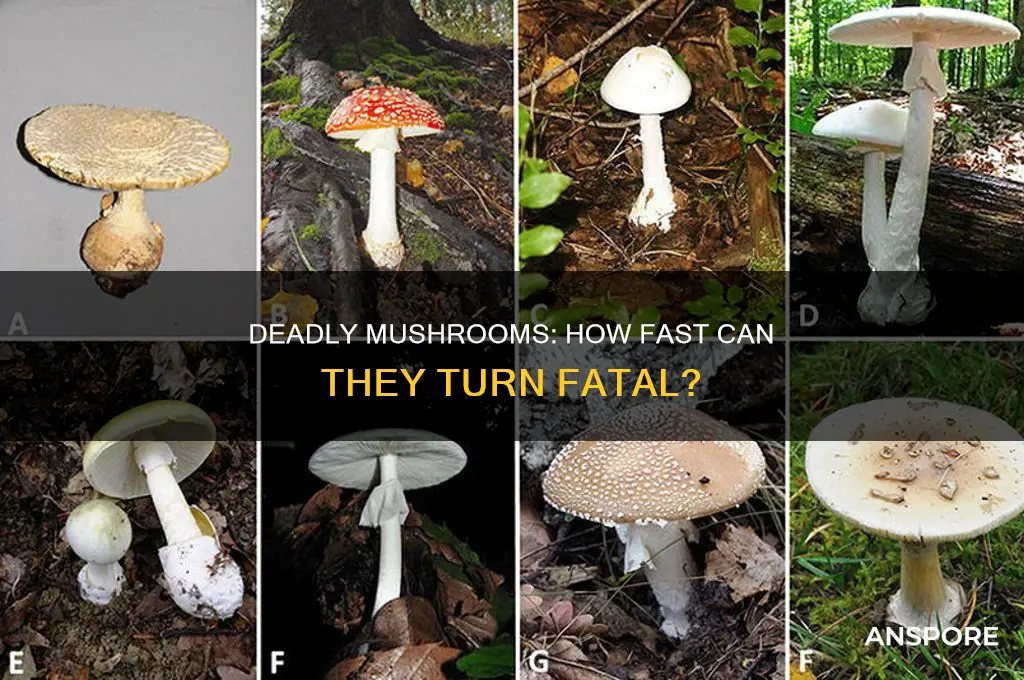
Mushrooms, often celebrated for their culinary and medicinal properties, harbor a darker side: some species are lethally toxic. Among the most notorious is the Death Cap (*Amanita phalloides*), responsible for the majority of fatal mushroom poisonings worldwide. Its toxins, primarily alpha-amanitin, cause severe liver and kidney damage, often leading to death within 5–10 days if left untreated. A single Death Cap contains enough toxin to kill an adult, and its innocuous appearance—resembling edible varieties like the Paddy Straw mushroom—makes it particularly dangerous.
Another deadly species is the Destroying Angel (*Amanita bisporigera* and *A. ocreata*), often mistaken for button mushrooms or meadow mushrooms. Its amatoxins, similar to those in the Death Cap, cause gastrointestinal symptoms within 6–24 hours, followed by organ failure. Unlike some toxins that act within hours, amatoxins’ delayed onset can lull victims into a false sense of security, delaying critical treatment. Children are especially vulnerable due to their lower body mass, with ingestion of even a small fragment proving fatal.
The Fool’s Mushroom (*Amanita verna*) and Conical Galerina (*Galerina marginata*) are equally treacherous. The Fool’s Mushroom, often found in European woodlands, contains the same amatoxins as its cousins, while *Galerina marginata* produces deadly amanitin-like compounds. Both are small, unassuming, and easily overlooked, yet a single cap can deliver a lethal dose. Foragers must avoid damp, woody habitats where *Galerina* thrives, particularly in North America and Europe.
To protect yourself, follow these critical steps: never consume wild mushrooms without expert identification, even if they resemble edible species. Carry a detailed field guide or consult a mycologist. If ingestion occurs, seek immediate medical attention, bringing a sample for identification. Time is critical—symptoms may not appear for hours, but treatment (activated charcoal, supportive care, and, in severe cases, liver transplants) must begin swiftly to prevent irreversible damage.
In summary, the deadliest mushrooms—Death Cap, Destroying Angel, Fool’s Mushroom, and Conical Galerina—share a deceptive simplicity and potent toxins. Their rapid lethality underscores the importance of caution in foraging. Knowledge, vigilance, and respect for these organisms are your best defenses against their silent, deadly threat.
Creating a Thriving Mushroom Biome: Tips and Techniques for Success
You may want to see also

Symptoms of Poisoning: Recognize early signs of mushroom toxicity before it’s too late
Mushroom poisoning can escalate from mild discomfort to life-threatening organ failure within hours, depending on the species ingested. The deadliest, like the Death Cap (*Amanita phalloides*), contain amatoxins that cause irreversible liver damage, often with a deceptive delay of 6–24 hours before symptoms appear. Recognizing early signs is critical, as prompt medical intervention can mean the difference between recovery and fatality.
Initial Symptoms: The Silent Alarm
The first signs of mushroom toxicity often mimic common gastrointestinal issues, making them easy to dismiss. Nausea, vomiting, diarrhea, and abdominal pain typically appear 6–12 hours after ingestion, depending on the toxin and dose. For instance, a single Death Cap contains enough amatoxins to kill an adult, but symptoms may not manifest until the toxins have already begun damaging the liver. Unlike food poisoning, these symptoms persist and worsen, often accompanied by dehydration and electrolyte imbalances, particularly in children or the elderly, who are more susceptible due to lower body mass.
Progressive Indicators: When to Act Urgently
As toxins infiltrate the bloodstream, systemic symptoms emerge. Jaundice (yellowing of the skin or eyes), confusion, and seizures signal liver or kidney failure, typically 24–48 hours post-ingestion. In severe cases, like with the Destroying Angel (*Amanita bisporigera*), symptoms progress rapidly, leading to coma or death within 72 hours without treatment. Monitoring urine output is crucial; dark urine or absence of urination indicates acute kidney injury, a red flag requiring immediate hospitalization.
High-Risk Groups and Practical Tips
Children under 12 and adults over 65 face higher risks due to slower toxin metabolism and weaker immune responses. Foraging without expertise is the leading cause of poisoning, as toxic species often resemble edible varieties (e.g., the Death Cap vs. the Paddy Straw mushroom). If ingestion is suspected, preserve a sample of the mushroom for identification and induce vomiting only if advised by poison control. Activated charcoal may reduce toxin absorption if administered within 1–2 hours, but it’s no substitute for professional care.
Takeaway: Time Is Tissue
Early recognition of symptoms—persistent gastrointestinal distress, neurological changes, or jaundice—coupled with swift action, can prevent fatal outcomes. Treatment includes gastric lavage, intravenous fluids, and, in severe cases, liver transplants. Remember: mushroom toxins act fast, but so can you. Always verify mushroom identity with a mycologist, and when in doubt, throw it out. Your caution today could save a life tomorrow.
Can Dog Poop Grow Mushrooms? Unveiling the Surprising Truth
You may want to see also

Time to Fatality: Understand how quickly symptoms escalate to death after ingestion
The time it takes for mushrooms to become lethal varies dramatically depending on the species ingested. For instance, the Death Cap (*Amanita phalloides*) contains amatoxins that can cause fatal liver failure, but symptoms may not appear for 6–24 hours after consumption. This delay often leads to misdiagnosis, as initial signs like nausea and vomiting resemble food poisoning. By the time organ damage becomes apparent, irreversible harm may have occurred, with death possible within 5–7 days without intervention.
Contrast this with the Destroying Angel (*Amanita bisporigera*), whose toxins act faster due to higher amatoxin concentrations. Symptoms can emerge within 5–10 hours, progressing to severe dehydration, kidney failure, and death within 2–3 days. Dosage matters: a single Death Cap or Destroying Angel can be fatal to an adult, while children are at higher risk due to their lower body mass. Immediate medical attention, including activated charcoal administration and liver support, is critical to improving survival odds.
Not all toxic mushrooms operate on this timeline. The Galerina genus, often mistaken for edible mushrooms, contains toxins similar to the Death Cap but in smaller quantities. Symptoms may take 12–48 hours to appear, with fatality occurring within 5–10 days. Conversely, hallucinogenic mushrooms like *Psilocybe* species rarely cause death directly, though psychological distress or accidents during intoxication can lead to indirect fatalities. Understanding these timelines underscores the importance of accurate identification and swift action.
Practical tips for minimizing risk include avoiding wild mushroom foraging without expert guidance, carrying a reliable field guide, and seeking medical help immediately if ingestion is suspected. Hospitals can administer antidotes like silibinin or perform liver transplants in severe cases, but time is of the essence. The adage "there are old mushroom hunters, and there are bold mushroom hunters, but there are no old, bold mushroom hunters" rings true—caution saves lives.
Is Cream of Mushroom Soup Vegan? Exploring Plant-Based Options
You may want to see also
Explore related products
$7.62 $14.95

Treatment Options: Learn immediate steps to take if poisoned by a deadly mushroom
Time is of the essence when dealing with mushroom poisoning. The speed at which symptoms appear and worsen depends on the species ingested, but some toxins can act within 30 minutes to 2 hours, causing severe organ damage or failure. For instance, the Death Cap (*Amanita phalloides*) contains amatoxins that can lead to liver and kidney failure within 24–48 hours if untreated. Recognizing the urgency, immediate action is critical to prevent irreversible harm or death.
Step 1: Call Emergency Services or Poison Control. Do not wait for symptoms to appear. Provide details about the mushroom if possible—take a photo or describe its appearance. For children or pets, act even faster; their smaller bodies metabolize toxins more rapidly. In the U.S., call the Poison Help Line at 1-800-222-1222. In the UK, contact NHS 111 or 999 in severe cases. Immediate medical guidance can save lives.
Step 2: Induce Vomiting (If Advised). For some poisonings, vomiting can help expel toxins before absorption. However, this should only be done if recommended by a professional, as it can be harmful in certain cases (e.g., if the mushroom causes neurological symptoms). For adults, a dose of syrup of ipecac (if available) may be suggested, but follow expert instructions precisely. For children, never induce vomiting without medical approval.
Step 3: Preserve a Sample of the Mushroom. If safe to do so, collect a sample of the mushroom in a paper bag (not plastic, as it can accelerate decay). This aids identification and treatment. Avoid touching your face or eyes while handling it, and wash hands thoroughly afterward. Even a small fragment can be invaluable for toxicologists.
Step 4: Monitor Symptoms and Administer First Aid. While waiting for help, monitor vital signs like breathing, heart rate, and consciousness. If the person becomes unresponsive, administer CPR if trained to do so. For gastrointestinal symptoms (e.g., diarrhea or vomiting), keep the person hydrated with small sips of water, but avoid food or medications unless instructed by a professional.
Caution: Avoid Folk Remedies. Myths like "cooking mushrooms neutralizes toxins" or "animals can test toxicity" are dangerous. No home test or remedy reliably identifies or treats poisoning. Rely solely on medical advice. Delaying professional care to try unproven methods can be fatal.
In conclusion, swift, informed action is the cornerstone of survival in mushroom poisoning. From immediate contact with experts to careful preservation of evidence, every step matters. While some toxins act rapidly, prompt treatment can mitigate damage and improve outcomes. Always prioritize professional guidance over guesswork in these life-threatening situations.
Baking with Mushrooms: Can You Add Them to Cookies?
You may want to see also

Prevention Tips: Avoid accidental poisoning with safe foraging and identification practices
Mushroom poisoning can be swift and deadly, with symptoms appearing as quickly as 20 minutes after ingestion in severe cases. The toxicity of certain species, like the Death Cap (*Amanita phalloides*), can lead to liver failure within 48 hours, often proving fatal without immediate medical intervention. Understanding the risks underscores the importance of safe foraging practices to prevent accidental poisoning.
Step 1: Educate Yourself Before Foraging
Never rely on folklore or superficial traits like color or gills to identify mushrooms. Many toxic species resemble edible ones, such as the Jack-O’-Lantern mushroom (*Omphalotus olearius*), which mimics chanterelles but causes severe gastrointestinal distress. Invest in a reputable field guide or consult a mycologist. Attend local foraging workshops to learn hands-on identification techniques, focusing on key features like spore color, bruising reactions, and habitat.
Step 2: Follow the “100% Certainty Rule”
If you’re not absolutely sure of a mushroom’s identity, leave it alone. Even experienced foragers discard questionable finds. Avoid collecting mushrooms near polluted areas, as they absorb toxins from soil. For example, mushrooms growing along roadsides may contain high levels of heavy metals, making them unsafe despite correct identification.
Step 3: Practice Safe Handling and Preparation
Always carry collected mushrooms in a breathable container like a paper bag to preserve their features for identification. Never mix species in the same container, as toxins can transfer. When preparing mushrooms, cook them thoroughly—some toxins are destroyed by heat. For instance, raw *Tricholoma equestre* can cause rhabdomyolysis, but cooking reduces this risk significantly.
Cautionary Notes and Final Thoughts
Children and pets are particularly vulnerable to mushroom poisoning due to their smaller body mass and tendency to explore. Teach children never to touch or taste wild mushrooms, and keep pets on a leash in wooded areas. If poisoning is suspected, contact a poison control center immediately, bringing a sample of the mushroom for identification. Time is critical—symptoms like vomiting, diarrhea, or confusion require urgent medical attention. Safe foraging isn’t about taking risks; it’s about respecting nature’s complexity and prioritizing caution at every step.
Winter Care for Mushroom Logs: Outdoor Survival Tips and Best Practices
You may want to see also
Frequently asked questions
The time it takes for poisonous mushrooms to cause fatal symptoms varies depending on the species. Some toxic mushrooms, like the Death Cap (*Amanita phalloides*), can cause severe liver and kidney damage within 24–48 hours after ingestion, leading to death in 5–10 days without medical intervention.
No, there are no mushrooms that cause instant death. However, some highly toxic species, such as the Destroying Angel (*Amanita bisporigera*), can cause rapid and severe symptoms like organ failure, which can be fatal within days if not treated promptly.
Symptoms can appear anywhere from 20 minutes to 24 hours after ingestion, depending on the type of toxin. For example, mushrooms containing amatoxins (like the Death Cap) may delay symptoms for 6–12 hours, while those with muscarine (like certain *Clitocybe* species) can cause symptoms within 15–30 minutes.











































