
Drug testing for psychedelic mushrooms, which contain psychoactive compounds like psilocybin and psilocin, involves specific methods to detect their presence in biological samples such as urine, blood, or hair. Unlike common drugs, psilocybin is not typically included in standard drug screenings, requiring specialized tests like gas chromatography-mass spectrometry (GC-MS) or liquid chromatography-tandem mass spectrometry (LC-MS/MS) for accurate detection. These tests can identify metabolites of psilocybin, which are usually detectable in urine for up to 24 hours after ingestion, though this window can vary based on dosage, metabolism, and frequency of use. Hair testing may extend detection times to weeks or months, making it useful for long-term monitoring. Understanding these methods is crucial for forensic, medical, or workplace testing purposes, as well as for research into the effects and prevalence of psychedelic mushroom use.
Explore related products
What You'll Learn
- Sample Collection Methods: Urine, hair, blood, or saliva—each has pros, cons, and detection windows for psilocybin
- Testing Kits Overview: At-home vs. lab tests; accuracy, cost, and ease of use compared
- Psilocybin Detection Window: How long mushrooms stay detectable in the body by sample type
- False Positive Risks: Common substances or medications that may trigger incorrect test results
- Legal and Ethical Considerations: Privacy laws, workplace policies, and consent in drug testing

Sample Collection Methods: Urine, hair, blood, or saliva—each has pros, cons, and detection windows for psilocybin
Urine Testing is the most common method for detecting psilocybin due to its non-invasiveness and cost-effectiveness. Psilocybin and its metabolite, psilocin, are typically detectable in urine within 2-24 hours after ingestion and can remain present for up to 3 days, depending on dosage and individual metabolism. The primary advantage of urine testing is its ability to provide relatively quick results with minimal discomfort to the individual. However, it has a limited detection window compared to other methods, making it less suitable for identifying long-past use. Additionally, urine samples can be tampered with, requiring strict collection protocols to ensure accuracy.
Hair Testing offers the longest detection window for psilocybin, potentially identifying use up to 90 days after ingestion. Psilocybin metabolites become embedded in hair strands as they grow, providing a historical record of drug use. This method is highly resistant to tampering and is ideal for detecting chronic or past use. However, hair testing has significant drawbacks. It cannot pinpoint recent use due to the time it takes for drugs to incorporate into hair (typically 7-10 days). Additionally, external factors like hair treatments or environmental contaminants can affect results. Hair testing is also more expensive and time-consuming than other methods.
Blood Testing is highly invasive but provides precise detection of psilocybin within a short window, typically 6-24 hours after ingestion. This method is most effective for identifying recent or active intoxication, as psilocybin clears the bloodstream rapidly. Blood tests are considered highly accurate and are often used in forensic or medical settings. However, the short detection window limits their utility for detecting past use. The invasiveness of blood collection also makes it less practical for routine or workplace testing.
Saliva Testing is gaining popularity due to its ease of collection and non-invasive nature. Psilocybin can be detected in saliva within minutes of ingestion and remains present for up to 24 hours. This method is particularly useful for on-the-spot testing, such as in roadside or workplace screenings. Saliva testing is less prone to tampering compared to urine and provides a balance between detection window and convenience. However, its relatively short detection period and lower sensitivity compared to urine or blood make it less reliable for identifying infrequent or past use.
Each sample collection method has distinct advantages and limitations, making the choice dependent on the specific testing goals. Urine and saliva are ideal for quick, non-invasive screening, while hair testing is best for long-term detection. Blood testing, though invasive, offers precise short-term results. Understanding these differences ensures the selection of the most appropriate method for detecting psilocybin use in various contexts.
Mushrooms: Brain Damage or Brain Boost?
You may want to see also

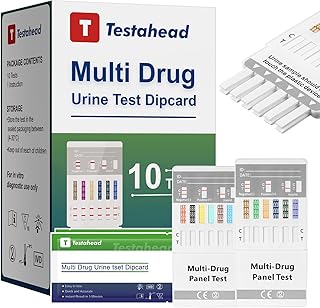
Testing Kits Overview: At-home vs. lab tests; accuracy, cost, and ease of use compared
When it comes to testing for psychedelic mushrooms, individuals have two primary options: at-home testing kits or laboratory tests. Each method has its advantages and drawbacks in terms of accuracy, cost, and ease of use. At-home testing kits are designed for convenience, allowing users to test substances in the privacy of their own homes. These kits typically use immunoassay technology, which detects the presence of specific compounds, such as psilocybin or psilocin, the active ingredients in psychedelic mushrooms. While at-home kits are generally affordable, ranging from $10 to $50, their accuracy can vary. False positives or negatives are possible, especially if the kit is not used correctly or if the sample is contaminated. However, for preliminary screening, they offer a quick and accessible solution.
Laboratory tests, on the other hand, provide a higher level of accuracy and reliability. These tests are conducted by trained professionals using advanced techniques like gas chromatography-mass spectrometry (GC-MS) or high-performance liquid chromatography (HPLC). These methods can precisely identify and quantify the compounds present in a sample, minimizing the risk of errors. Lab tests are ideal for confirming the presence of psychedelic mushrooms or verifying the results of an at-home test. However, this accuracy comes at a higher cost, typically ranging from $100 to $300, depending on the facility and the complexity of the analysis. Additionally, lab tests require sending a sample to a facility, which can take several days to a week for results, making them less convenient for immediate needs.
Ease of use is a significant factor when comparing at-home and lab tests. At-home kits are designed with simplicity in mind, often requiring minimal steps such as adding a sample to a test strip or solution and waiting for a color change or visual indicator. Instructions are usually straightforward, making them accessible even to those with no prior experience. In contrast, lab tests involve more complex procedures, including sample preparation and submission, which may require following specific guidelines to ensure accurate results. While lab tests are not difficult to initiate, the process is less hands-on for the user and demands patience while awaiting results.
Cost is another critical consideration. At-home testing kits are significantly more affordable, making them an attractive option for individuals on a budget or those who need to test multiple samples. Their low cost also reduces the financial risk if a mistake is made during testing. Lab tests, while more expensive, are a worthwhile investment for situations requiring definitive results, such as legal cases, research, or medical purposes. For casual users or those exploring harm reduction, at-home kits may suffice, but for critical applications, the higher cost of lab testing is justified by its precision.
In summary, the choice between at-home and lab testing kits for psychedelic mushrooms depends on the user’s priorities. At-home kits offer affordability, convenience, and quick results but may sacrifice some accuracy. Lab tests provide superior reliability and detailed analysis but are more expensive and time-consuming. For most individuals, at-home kits are a practical solution for initial screening, while lab tests are reserved for scenarios where certainty is paramount. Understanding these differences ensures users can make informed decisions based on their specific needs and circumstances.
Are Chicken and Mushroom Pot Noodles a Healthy Choice?
You may want to see also

Psilocybin Detection Window: How long mushrooms stay detectable in the body by sample type
Psilocybin, the primary psychoactive compound in psychedelic mushrooms, is metabolized by the body relatively quickly, but its detection window can vary depending on the type of drug test used. Understanding how long psilocybin remains detectable in different bodily samples is crucial for both testing purposes and personal awareness. The detection window is influenced by factors such as dosage, frequency of use, metabolism, and the sensitivity of the testing method. Below is a detailed breakdown of psilocybin detection windows by sample type.
Urine Testing: Urine tests are the most common method for detecting psilocybin use due to their non-invasiveness and cost-effectiveness. Psilocybin and its metabolites, such as psilocin, are typically detectable in urine for 24 to 48 hours after ingestion. However, in heavy or chronic users, traces may persist for up to 3 days. The detection window can be shorter because psilocybin is rapidly metabolized and excreted. It’s important to note that standard drug tests often do not screen for psilocybin, so specialized tests are required for accurate detection.
Blood Testing: Psilocybin can be detected in blood for a shorter duration compared to urine. Typically, it is detectable within 1 to 3 hours after ingestion and remains in the bloodstream for up to 12 hours. Blood tests are less commonly used for routine drug screening due to their invasive nature and the short detection window. However, they are highly accurate during this period and are often used in forensic or medical settings.
Saliva Testing: Saliva tests offer a non-invasive alternative for detecting recent psilocybin use. The compound is usually detectable in oral fluid for 1 to 3 hours after consumption, with the window rarely exceeding 24 hours. Saliva tests are less common for psilocybin detection but can be useful for identifying very recent use. The short detection window makes them less practical for extended monitoring.
Hair Testing: Hair follicle tests have the longest detection window for psilocybin, as drug metabolites become embedded in hair strands as they grow. Psilocybin can be detected in hair for up to 90 days after use, depending on the length of the hair sample. However, hair tests are less commonly used for psilocybin due to their higher cost and the fact that they do not detect recent use as effectively as other methods. Hair testing is more often employed for detecting long-term or chronic substance use.
Factors Affecting Detection Windows: Several factors can influence how long psilocybin remains detectable in the body. These include the individual’s metabolism, hydration levels, body mass, and the potency of the mushrooms consumed. Additionally, the sensitivity and specificity of the testing method play a significant role. For example, more advanced techniques like liquid chromatography-mass spectrometry (LC-MS) can detect lower concentrations of psilocybin and extend the detection window compared to standard immunoassay tests.
In summary, the psilocybin detection window varies significantly by sample type, with urine tests offering the most practical option for detecting recent use. Blood and saliva tests are useful for identifying very recent consumption, while hair tests provide a historical overview of use. Understanding these detection windows is essential for accurate drug testing and informed decision-making regarding psilocybin use.
Mastering Oyster Mushroom Spore Collection: A Step-by-Step Guide
You may want to see also
Explore related products

False Positive Risks: Common substances or medications that may trigger incorrect test results
When conducting drug tests for psychedelic mushrooms, which primarily detect the presence of psilocybin or psilocin, it’s crucial to be aware of substances or medications that can trigger false positive results. False positives occur when a test incorrectly identifies a legal or unrelated substance as the target drug. One common culprit is sertraline (Zoloft), a selective serotonin reuptake inhibitor (SSRI) used to treat depression and anxiety. Sertraline has been reported to cause false positives for psilocybin in urine tests due to its chemical structure and interaction with immunoassay-based testing methods. If a patient is taking sertraline, confirmatory tests like gas chromatography-mass spectrometry (GC-MS) should be used to avoid misinterpretation.
Another substance known to cause false positives is diphenhydramine, an antihistamine found in over-the-counter allergy and sleep medications like Benadryl. Diphenhydramine can cross-react with certain drug test panels, leading to incorrect results for psilocybin. Similarly, quetiapine (Seroquel), an antipsychotic medication, has been associated with false positives in drug screenings due to its metabolic byproducts. Patients taking these medications should inform testing personnel to ensure accurate interpretation of results.
Antidepressants and antipsychotics in general pose a risk for false positives in psychedelic mushroom tests. Medications like fluoxetine (Prozac), bupropion (Wellbutrin), and trazodone have been documented to interfere with immunoassay tests, potentially leading to incorrect identification of psilocybin. Additionally, over-the-counter supplements such as St. John’s Wort, which affects serotonin levels, may also trigger false positives due to their interaction with the body’s neurotransmitter systems.
Cold and flu medications containing dextromethorphan (DXM) are another potential source of false positives. DXM, found in cough syrups like Robitussin, can cross-react with drug test panels, especially if the test is not specific to psilocybin. Similarly, antibiotics such as amoxicillin or erythromycin have been anecdotally linked to false positives in drug screenings, though the mechanism is not fully understood. It’s essential to review a patient’s full medication list before interpreting test results.
Finally, food contaminants or natural substances can occasionally cause false positives. For example, consuming hemp seeds or CBD products may lead to false positives for THC, which could complicate the interpretation of a psychedelic mushroom test if the panel includes multiple substances. While not directly related to psilocybin, such cross-reactions highlight the importance of using confirmatory testing methods like GC-MS or liquid chromatography-tandem mass spectrometry (LC-MS/MS) to ensure accuracy and avoid false accusations. Always cross-reference initial test results with a patient’s medical history and medication profile to minimize errors.
Mushrooms' Role in Absorbing Ammonia and Nitrates: A Natural Solution
You may want to see also

Legal and Ethical Considerations: Privacy laws, workplace policies, and consent in drug testing
When implementing drug testing for psychedelic mushrooms, it is crucial to navigate the complex landscape of legal and ethical considerations, particularly concerning privacy laws, workplace policies, and consent. Privacy laws vary significantly by jurisdiction, and organizations must ensure compliance with regulations such as the General Data Protection Regulation (GDPR) in Europe or the Health Insurance Portability and Accountability Act (HIPAA) in the United States. These laws dictate how personal health information, including drug test results, can be collected, stored, and shared. Employers must establish clear protocols to safeguard employee privacy, ensuring that drug test results are treated as confidential medical data and accessed only by authorized personnel. Failure to comply with privacy laws can result in severe legal penalties and damage to the organization's reputation.
Workplace policies play a pivotal role in the ethical implementation of drug testing for psychedelic mushrooms. Employers should develop transparent policies that clearly outline the purpose of testing, the substances being screened for, and the consequences of positive results. Policies must be consistently applied to all employees to avoid allegations of discrimination. Additionally, workplaces should consider the legality of psychedelic substances in their jurisdiction, as some regions have decriminalized or legalized certain psychedelics for medical or recreational use. Policies should reflect these legal nuances to ensure fairness and avoid potential legal challenges. It is also advisable to involve legal counsel in drafting these policies to ensure they align with both local laws and organizational values.
Consent is another critical ethical consideration in drug testing. Employees must provide informed consent before undergoing any drug test, which requires clear communication about the reasons for testing, the methods used, and how the results will be handled. Coerced or uninformed consent undermines the ethical integrity of the process and may lead to legal disputes. In certain contexts, such as pre-employment screening, consent may be implied as a condition of hiring, but this must be explicitly stated in job offers or contracts. For existing employees, consent should be sought separately, and they should have the right to refuse testing, though this may have consequences as outlined in workplace policies.
The intersection of privacy laws and workplace policies also raises questions about the scope of drug testing. For instance, testing for psychedelic mushrooms in a workplace setting may be justifiable in safety-sensitive industries, such as transportation or healthcare, where impairment could pose significant risks. However, in less critical roles, the justification for testing becomes less clear, potentially infringing on employees' privacy rights. Employers must balance the need for a safe work environment with respect for individual autonomy, ensuring that drug testing is proportionate and necessary. Regular reviews of testing policies, in consultation with employees or their representatives, can help maintain this balance.
Finally, ethical considerations extend to the treatment of employees who test positive for psychedelic mushrooms. Rather than defaulting to punitive measures, such as termination, employers should explore supportive options, particularly if the use is related to mental health or medical conditions. Providing access to counseling, rehabilitation programs, or employee assistance services aligns with ethical principles of care and fairness. This approach not only supports employees but also fosters a positive workplace culture that values well-being over punishment. By addressing drug testing with sensitivity and respect, organizations can uphold both legal compliance and ethical standards.
Mushrooms: Essential or Optional?
You may want to see also
Frequently asked questions
Common methods include urine tests, blood tests, and hair follicle tests. Urine tests are the most frequently used due to their non-invasiveness and ability to detect psilocybin and psilocin, the active compounds in psychedelic mushrooms, for up to 24-48 hours after use.
Psilocybin and psilocin are typically detectable in urine for 24-48 hours, in blood for up to 24 hours, and in hair follicles for up to 90 days. Detection times can vary based on factors like dosage, metabolism, and frequency of use.
Yes, there are at-home drug tests designed to detect psilocybin and psilocin in urine. However, these tests may not be as accurate as laboratory-based tests, and false negatives or positives can occur.
Standard drug test panels (e.g., 5-panel or 10-panel tests) typically do not screen for psilocybin or psilocin. Specialized tests are required to detect these compounds, as they are not commonly included in routine drug screenings.
![[5 pack] Prime Screen 14 Panel Urine Drug Test Cup - Instant Testing Marijuana (THC),OPI,AMP, BAR, BUP, BZO, COC, mAMP, MDMA, MTD, OXY, PCP, PPX, TCA](https://m.media-amazon.com/images/I/71cI114sLUL._AC_UL320_.jpg)

![Prime Screen-12 Panel Multi Drug Urine Test Compact Cup (THC 50, AMP,BAR,BUP,BZO,COC,mAMP/MET,MDMA,MOP/OPI,MTD,OXY,PCP) C-Cup-[1 Pack]](https://m.media-amazon.com/images/I/714z5mLCPkL._AC_UL320_.jpg)
![Prime Screen Multi-Drug Urine Test Cup 16 Panel Kit (AMP,BAR,BUP,BZO,COC,mAMP,MDMA,MOP/OPI,MTD,OXY,PCP,THC, ETG, FTY, TRA, K2) -[1 Pack]-CDOA-9165EFTK](https://m.media-amazon.com/images/I/718HvC-tp-L._AC_UL320_.jpg)


![Easy@Home 5 Panel Urine Drug Test Kit [5 Pack] - THC/Marijuana, Cocaine, OPI/Opiates, AMP, BZO All Drugs Testing Strips in One Kit - at Home Use Screening Test with Results in 5 Mins #EDOAP-754](https://m.media-amazon.com/images/I/81pqr85M3-L._AC_UL320_.jpg)
![Prime Screen [5 Pack] 6 Panel Urine Drug Test Kit (THC-Marijuana, BZO-Benzos, MET-Meth, OPI, AMP, COC), WDOA-264](https://m.media-amazon.com/images/I/71hU5zzuEaL._AC_UL320_.jpg)
![[1 Test Cup] 14-Panel EZCHECK® Multi-Drug Urine Test Cup – at-Home Instant Testing for 14 Substances - Fast Result in 5 mins - FSA/HSA Eligible](https://m.media-amazon.com/images/I/71Geu5JRvZL._AC_UL320_.jpg)
![Prime Screen-12 Panel Multi Drug Urine Test Compact Cup (AMP,BAR,BUP,BZO,COC,mAMP/MET,MDMA,MOP/OPI,MTD,OXY,PCP,THC) C-Cup-[2 Pack]- CDOA-6125](https://m.media-amazon.com/images/I/81wHyqSLmsL._AC_UL320_.jpg)



![Prime Screen [5 Pack] 12 Panel Urine Drug Test Kit (AMP, BAR, BUP, Benzos BZO, COC, mAMP, MDMA, MOP, MTD, OXY, PCP, Marijuana THC) - WDOA-6125](https://m.media-amazon.com/images/I/51jbz+-PFBL._AC_UL320_.jpg)
![Prime Screen 14 Panel Urine Drug Test Cup Instant Testing Marijuana (THC),OPI,AMP, BAR, BUP, BZO, COC, mAMP, MDMA, MTD, OXY, PCP, PPX, TCA [1 Pack]](https://m.media-amazon.com/images/I/7176xYFYqTL._AC_UL320_.jpg)

![Prime Screen THC & Nicotine (Cotinine) Combo Test Kit-Detects THC (Weed) and Nicotine Metabolite Cotinine (COT) for Vaping, Smoking, and Tobacco Use [10 Pack]](https://m.media-amazon.com/images/I/71T-AuwV7WL._AC_UL320_.jpg)
![[5 Pack] Prime Screen 12 Panel Urine Test (AMP,BAR,BZO,COC,mAMP,MDMA,MOP/OPI 300,MTD,OXY,PCP,TCA,THC) - WDOA-7125](https://m.media-amazon.com/images/I/71Hy719lOfL._AC_UL320_.jpg)

![[5 Pack] Prime Screen Multi Drug Urine Test Cup -6 Panel (BZO,COC,mAMP,OPI, OXY,THC) C-CUP-TDOA-564](https://m.media-amazon.com/images/I/71ZZPH0MbUL._AC_UL320_.jpg)
![Prime Screen [5 Pack] 5 Panel Urine Drug Test Kit - Testing Instantly for 5 Different Drugs AMP, COC, MET (Meth), OPI, THC (Marijuana) - WDOA-254](https://m.media-amazon.com/images/I/71FsDMfvdFL._AC_UL320_.jpg)





















