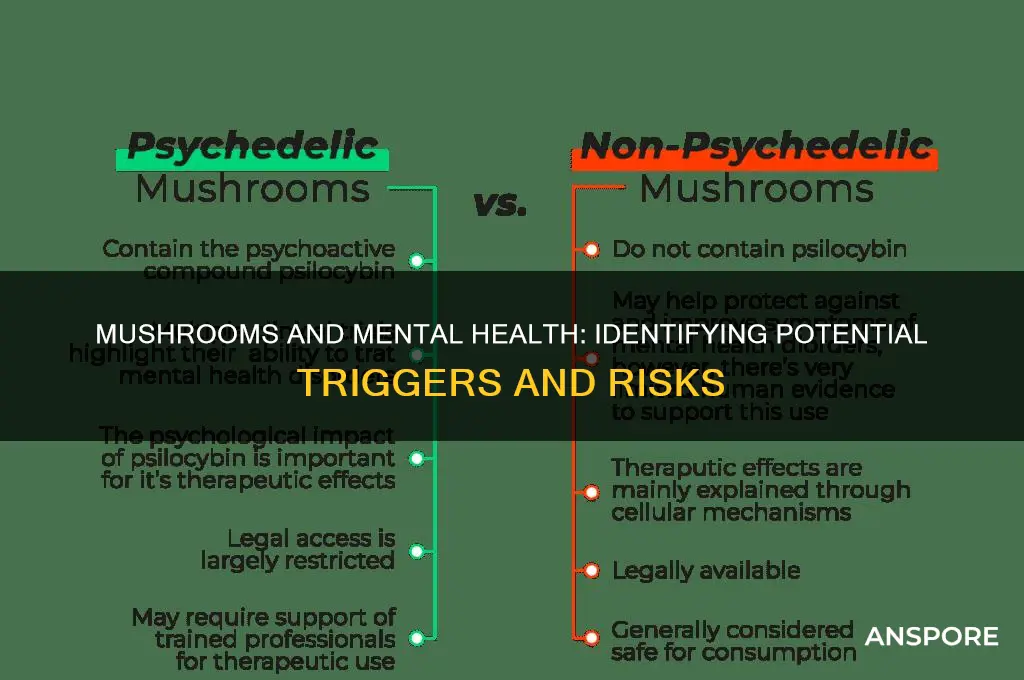
Determining whether the use of mushrooms, particularly psilocybin-containing varieties, has triggered or exacerbated a mental illness can be complex and requires careful consideration. While psilocybin has shown therapeutic potential in controlled settings for conditions like depression and anxiety, its recreational or unsupervised use can lead to unpredictable outcomes, especially in individuals predisposed to mental health issues. Key indicators to monitor include sudden or severe changes in mood, perception, or behavior, such as persistent paranoia, hallucinations, or disorganized thinking, which may suggest the onset of conditions like psychosis or schizophrenia. Additionally, a personal or family history of mental illness increases the risk of adverse reactions. Consulting a mental health professional is crucial for accurate assessment and guidance, as they can differentiate between temporary psychedelic effects and symptoms of a developing mental health disorder.
Explore related products
What You'll Learn
- Onset of Symptoms: Sudden or delayed mental health changes after mushroom use
- Pre-existing Conditions: How prior mental health issues may increase risk
- Dosage and Type: Impact of mushroom potency and species on mental effects
- Psychotic Episodes: Hallucinations or paranoia persisting post-consumption
- Long-term Effects: Persistent anxiety, depression, or psychosis after mushroom use

Onset of Symptoms: Sudden or delayed mental health changes after mushroom use
The onset of mental health symptoms after using mushrooms can vary significantly, making it crucial to distinguish between immediate reactions and delayed effects. Sudden onset typically occurs within hours of ingestion, often during or shortly after the psychedelic experience. Users may experience acute anxiety, paranoia, or hallucinations that feel overwhelming and dissociative. These symptoms are usually transient, resolving as the drug’s effects wear off. However, in some cases, the intensity of the experience can trigger latent mental health conditions, such as schizophrenia or bipolar disorder, in individuals who are genetically predisposed. If symptoms like persistent psychosis, severe mood swings, or disorganized thinking emerge abruptly and continue beyond the drug’s duration, it may indicate a triggered mental illness rather than a temporary reaction.
Delayed onset of mental health changes is more insidious and challenging to link directly to mushroom use. Symptoms may appear days, weeks, or even months after consumption. This can include persistent anxiety, depression, or cognitive disturbances like difficulty concentrating or memory issues. Delayed onset is often associated with hallucinogen persisting perception disorder (HPPD), where flashbacks or visual disturbances recur long after the drug has left the system. Additionally, individuals may develop symptoms of post-traumatic stress disorder (PTSD) if the psychedelic experience was traumatic or emotionally destabilizing. It’s important to monitor for gradual changes in behavior, mood, or perception, as these may signal an underlying mental health issue exacerbated by mushroom use.
In both sudden and delayed cases, the context of the experience plays a critical role. A "bad trip" characterized by fear, confusion, or loss of control can precipitate immediate or long-term psychological distress. Conversely, a seemingly positive experience may still unmask vulnerabilities in individuals with a family history of mental illness. Tracking the timeline of symptom onset relative to mushroom use is essential for assessment. Sudden symptoms often require immediate intervention, while delayed symptoms may necessitate long-term psychiatric care or therapy.
To determine if mushroom use has triggered a mental illness, professional evaluation is indispensable. Mental health professionals can differentiate between drug-induced psychosis, HPPD, or PTSD and primary psychiatric disorders. They may use diagnostic tools like the DSM-5 criteria or conduct a thorough psychiatric history to identify predisposing factors. Self-monitoring is also valuable; keeping a journal of symptoms, their intensity, and their duration can provide critical insights during evaluation. Early recognition and treatment are key to managing potential long-term consequences.
Finally, prevention and education are vital in mitigating risks. Individuals with a personal or family history of mental illness should approach psychedelics with caution, as they are at higher risk of adverse outcomes. Setting, mindset, and dosage also influence the experience, with controlled environments and informed use reducing the likelihood of triggering mental health issues. Understanding the potential for both sudden and delayed onset of symptoms empowers users to make informed decisions and seek help when needed.
Mushrooms: Fruits or Fungi?
You may want to see also

Pre-existing Conditions: How prior mental health issues may increase risk
Individuals with pre-existing mental health conditions may face heightened risks when using psychedelic mushrooms, as these substances can interact with underlying vulnerabilities in complex ways. Conditions such as schizophrenia, bipolar disorder, severe anxiety, or major depressive disorder can predispose individuals to adverse psychological reactions. Psilocybin, the active compound in mushrooms, affects serotonin receptors in the brain, which are often already dysregulated in these disorders. This interaction can amplify symptoms or trigger latent issues, making it difficult to discern whether the mushroom use exacerbated an existing condition or created a new one. Understanding this risk is crucial for anyone with a history of mental health challenges considering psychedelic use.
For those with schizophrenia or schizoaffective disorder, mushrooms can pose a particularly significant risk. These conditions involve abnormalities in perception and thought processes, and psilocybin’s hallucinogenic effects can mimic or intensify psychotic symptoms, such as hallucinations or paranoia. Even individuals with a family history of psychosis may be at increased risk, as mushrooms could potentially unmask a genetic predisposition. Similarly, individuals with bipolar disorder may experience mood destabilization, leading to manic or depressive episodes that are harder to manage after psychedelic use. These outcomes highlight the importance of screening for pre-existing conditions before experimenting with mushrooms.
Anxiety and depressive disorders also warrant careful consideration. While some studies suggest psilocybin may alleviate symptoms in controlled therapeutic settings, self-administration without professional oversight can have the opposite effect. Individuals with generalized anxiety disorder or PTSD, for instance, may experience overwhelming fear or re-traumatization during a psychedelic experience. Similarly, those with treatment-resistant depression might face prolonged emotional distress if the trip does not provide the hoped-for relief. The unpredictability of mushroom effects means that even individuals with well-managed conditions could encounter unexpected psychological challenges.
Personality traits and disorders, such as borderline personality disorder or high neuroticism, can further elevate risk. These traits often involve emotional instability or difficulty processing intense experiences, which mushrooms can exacerbate. A challenging trip could lead to prolonged feelings of depersonalization, existential distress, or a persistent alteration in self-perception. Such outcomes are more likely in individuals already struggling with emotional regulation or identity issues, underscoring the need for caution in this population.
Ultimately, the presence of pre-existing mental health conditions should prompt a thorough risk assessment before using mushrooms. Consulting with a mental health professional can help individuals understand their specific vulnerabilities and make informed decisions. Self-awareness and honesty about one’s mental health history are essential, as the line between a transformative experience and a triggering event can be thin. For those with prior conditions, the potential risks of mushroom use often outweigh the potential benefits, particularly outside of a controlled therapeutic environment.
Mushrooms: The Kingdom Between Plant and Animal
You may want to see also

Dosage and Type: Impact of mushroom potency and species on mental effects
The relationship between mushroom dosage, species, and their impact on mental health is a critical aspect to consider when evaluating whether psychedelic experiences might have triggered or exacerbated a mental illness. Dosage plays a pivotal role in determining the intensity and nature of the psychedelic experience. Psilocybin mushrooms, the most commonly used psychedelic fungi, contain varying concentrations of psilocybin and psilocin, the active compounds responsible for their effects. A low dose (typically 0.5–1 gram of dried mushrooms) may produce mild sensory enhancements and euphoria, while a high dose (2–5 grams or more) can lead to profound alterations in perception, ego dissolution, and intense emotional experiences. Higher doses are more likely to induce anxiety, paranoia, or psychotic-like symptoms, particularly in individuals predisposed to mental health conditions. These extreme experiences, often referred to as "bad trips," can sometimes mimic or trigger symptoms of mental illness, such as schizophrenia or bipolar disorder, especially if the individual is genetically vulnerable or has a personal or family history of such conditions.
The species of mushroom consumed is another crucial factor, as different species contain varying levels of psilocybin and other alkaloids, which can influence the nature and intensity of the experience. For example, *Psilocybe cubensis* is one of the most common species and is generally considered milder compared to *Psilocybe azurescens*, which is significantly more potent due to its higher psilocybin content. Consuming a potent species without awareness of its strength can lead to an overwhelming experience, increasing the risk of psychological distress. Additionally, misidentification of mushroom species can be dangerous, as some toxic mushrooms (e.g., *Galerina marginata*) resemble psychedelic varieties and can cause severe physical and mental health complications, including delirium or organ failure, which may be mistaken for a mental health crisis.
The interaction between dosage and individual sensitivity further complicates the picture. Factors such as body weight, metabolism, and prior experience with psychedelics influence how a person responds to a given dose. Individuals with a history of mental health issues, particularly psychotic disorders, are at higher risk of adverse reactions even at moderate doses. For example, a person with a predisposition to schizophrenia might experience a psychotic episode after consuming mushrooms, which could be misinterpreted as a spontaneous onset of the disorder rather than a drug-induced reaction. Similarly, individuals with anxiety or PTSD may find that mushrooms amplify their symptoms, leading to prolonged distress.
Understanding the long-term impact of mushroom use on mental health requires consideration of both dosage and frequency. While a single high-dose experience can sometimes lead to persistent changes in perception or mood, repeated use of high doses may increase the risk of developing psychiatric symptoms. The concept of "Hallucinogen Persisting Perception Disorder (HPPD)" highlights how intense psychedelic experiences can leave lasting visual or perceptual disturbances, which may contribute to anxiety or depression. However, it is important to distinguish between transient effects of the drug and the onset of a mental illness, as the former typically resolve over time without intervention.
In conclusion, dosage and mushroom species are key determinants of the mental effects experienced during and after psychedelic use. Higher doses and more potent species increase the likelihood of intense or adverse psychological reactions, particularly in vulnerable individuals. When assessing whether mushrooms have triggered a mental illness, it is essential to consider the specific circumstances of use, including the dose, species, and the individual’s mental health history. This information can help differentiate between a temporary drug-induced state and a potential underlying psychiatric condition, guiding appropriate intervention and support.
Beyond Burger: Mushrooms or Not?
You may want to see also
Explore related products

Psychotic Episodes: Hallucinations or paranoia persisting post-consumption
Psychotic episodes characterized by persistent hallucinations or paranoia after consuming mushrooms can be a significant indicator of a potential mental health issue triggered by psychedelic use. Unlike the transient effects typically experienced during a mushroom trip, these symptoms continue well beyond the drug’s active period, often lasting days, weeks, or even months. If you or someone you know is experiencing ongoing hallucinations (seeing, hearing, or feeling things that aren’t there) or paranoia (unfounded and intense fear or suspicion), it is crucial to consider whether these symptoms are linked to mushroom use. These persistent psychotic symptoms may resemble conditions like schizophrenia or schizoaffective disorder, particularly in individuals with a genetic predisposition or underlying vulnerability to mental illness.
One key factor in determining whether mushrooms have triggered a psychotic episode is the timeline of symptom onset. If hallucinations or paranoia emerge shortly after consumption and persist long after the drug has left the system, this suggests a potential causal relationship. It’s important to differentiate these symptoms from the acute effects of mushrooms, which usually subside within 6 to 12 hours. Persistent symptoms may indicate a drug-induced psychosis or the exacerbation of an underlying mental health condition. Seeking professional evaluation is essential, as early intervention can prevent long-term complications and improve outcomes.
Another critical aspect to consider is the presence of risk factors that increase susceptibility to mushroom-induced psychosis. Individuals with a personal or family history of mental illness, particularly psychotic disorders, are at higher risk. Additionally, factors such as high doses of mushrooms, frequent use, or consumption in a stressful or unsupportive environment can contribute to the development of persistent symptoms. If you have any of these risk factors and are experiencing ongoing hallucinations or paranoia, it is imperative to consult a mental health professional who can assess the situation and provide appropriate treatment.
Treatment for psychotic episodes triggered by mushrooms typically involves a combination of medication and therapy. Antipsychotic medications may be prescribed to manage hallucinations and paranoia, while psychotherapy, such as cognitive-behavioral therapy (CBT), can help individuals cope with distressing symptoms and address underlying psychological issues. In some cases, hospitalization may be necessary to ensure safety and stabilize symptoms. It’s also important to avoid further psychedelic use, as continued consumption can worsen symptoms and prolong recovery.
Prevention plays a vital role in minimizing the risk of mushroom-induced psychosis. Educating oneself about the potential risks of psychedelic use, especially for those with a history of mental health issues, is crucial. If you choose to use mushrooms, doing so in a controlled, supportive environment with a trusted individual can reduce the likelihood of adverse effects. However, for those who have already experienced persistent psychotic symptoms, focusing on treatment and recovery should be the priority. Recognizing the signs early and seeking help can make a significant difference in managing and overcoming these challenges.
Mushroom Genders: A Surprising Diversity in Nature
You may want to see also

Long-term Effects: Persistent anxiety, depression, or psychosis after mushroom use
While psychedelic mushrooms have been touted for their potential therapeutic benefits, it’s crucial to acknowledge that for some individuals, their use can lead to long-term mental health challenges. Persistent anxiety, depression, or psychosis after mushroom use is a serious concern that requires careful attention. These effects may not manifest immediately but can emerge days, weeks, or even months after consumption, often catching users off guard. Recognizing the signs early is essential for seeking appropriate intervention and preventing further deterioration of mental health.
One of the most alarming long-term effects is the development or exacerbation of persistent anxiety. Users may experience chronic feelings of unease, panic attacks, or an overwhelming sense of dread that interferes with daily functioning. This anxiety can be triggered by memories of the psychedelic experience, also known as "flashbacks," or it may arise without an apparent cause. Individuals may find themselves avoiding social situations, struggling with sleep, or constantly feeling on edge. If these symptoms persist and are directly linked to mushroom use, it’s critical to consult a mental health professional for evaluation and support.
Depression is another significant long-term effect that can follow mushroom use. Users may notice a persistent low mood, loss of interest in previously enjoyed activities, fatigue, or feelings of hopelessness. In some cases, this depression can be severe, leading to suicidal thoughts or behaviors. The onset may be gradual, making it difficult to attribute directly to mushroom use, but a thorough assessment of mental health history and substance use is essential. Treatment may involve therapy, medication, or both, tailored to the individual’s needs.
Psychosis is perhaps the most severe long-term effect, characterized by a disconnection from reality. Symptoms can include hallucinations, delusions, disorganized thinking, and impaired judgment. For some, a single psychedelic experience can trigger latent psychotic disorders, particularly in individuals with a genetic predisposition or pre-existing mental health conditions. Persistent psychosis after mushroom use may require long-term psychiatric care, including antipsychotic medications and therapy. Early detection is crucial, as untreated psychosis can lead to significant impairment in personal and professional life.
It’s important to note that not everyone who uses mushrooms will experience these long-term effects, but certain factors increase the risk. These include a personal or family history of mental illness, high doses of mushrooms, frequent use, or consuming mushrooms in an unsafe or unsupportive environment. If you or someone you know is experiencing persistent anxiety, depression, or psychosis after mushroom use, it’s vital to seek professional help promptly. Mental health professionals can provide a comprehensive assessment, determine the root cause of the symptoms, and develop a treatment plan to address both the immediate and long-term effects of psychedelic use.
Mushroom Hunting: Best Places to Forage
You may want to see also
Frequently asked questions
While mushrooms (psilocybin) can trigger latent mental health issues, they do not directly cause mental illness in individuals without predisposing factors. However, those with a family history of mental illness or underlying vulnerabilities may experience psychosis, anxiety, or mood disorders after use.
If symptoms like paranoia, hallucinations, or severe anxiety appear shortly after mushroom use and persist, it may be related. Consult a mental health professional for an accurate assessment, as symptoms could also stem from pre-existing conditions or other triggers.
For most people, occasional use does not lead to long-term mental health issues. However, heavy or frequent use, especially in vulnerable individuals, can increase the risk of persistent psychosis, flashbacks, or mood disorders.
Seek immediate medical or psychiatric help. A professional can evaluate symptoms, provide treatment, and determine if the issue is mushroom-related or requires ongoing mental health care. Avoid further substance use during this time.