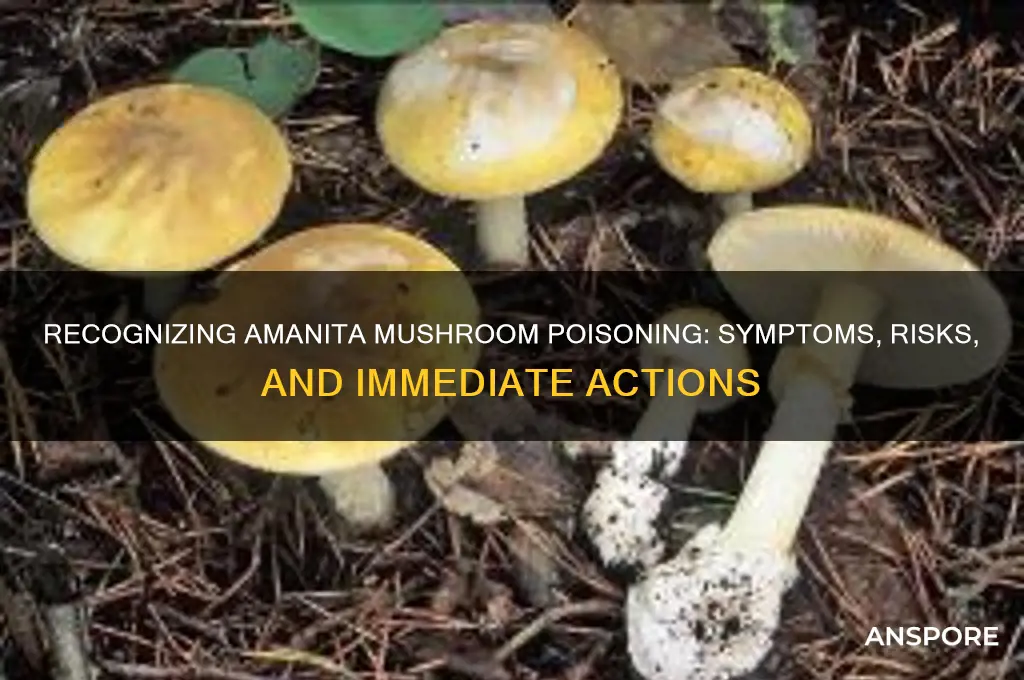
Amanita mushroom poisoning is a serious and potentially life-threatening condition caused by ingesting certain species of Amanita mushrooms, which contain toxins like amatoxins and orellanine. Symptoms typically appear within 6 to 24 hours after consumption and can range from mild gastrointestinal distress, such as nausea, vomiting, and diarrhea, to severe complications like liver and kidney failure. Early signs may be deceptive, as some species initially cause few symptoms, leading to a false sense of safety. If you suspect ingestion of an Amanita mushroom, seek immediate medical attention, as prompt treatment, including supportive care and, in severe cases, liver transplantation, can be crucial for survival. Accurate identification of the mushroom and awareness of symptoms are key to timely intervention.
| Characteristics | Values |
|---|---|
| Symptoms Onset | Typically 6-24 hours after ingestion, but can be as early as 2 hours. |
| Gastrointestinal Symptoms | Severe nausea, vomiting, diarrhea, abdominal pain, and cramps. |
| Dehydration | Rapid fluid loss due to vomiting and diarrhea. |
| Neurological Symptoms | Dizziness, confusion, drowsiness, or hallucinations in severe cases. |
| Liver Damage | Jaundice (yellowing of skin/eyes), dark urine, and elevated liver enzymes. |
| Kidney Damage | Reduced urine output, swelling, and kidney failure in severe cases. |
| Cardiovascular Symptoms | Low blood pressure, rapid heartbeat, or shock in extreme cases. |
| Long-Term Effects | Potential for liver or kidney failure, requiring transplant or dialysis. |
| Fatality Risk | High without prompt medical treatment; mortality rates up to 10-15%. |
| Diagnosis | Based on symptoms, recent mushroom ingestion, and liver function tests. |
| Treatment | Gastric lavage, activated charcoal, IV fluids, and liver support therapy. |
| Prevention | Avoid consuming wild mushrooms unless identified by an expert mycologist. |
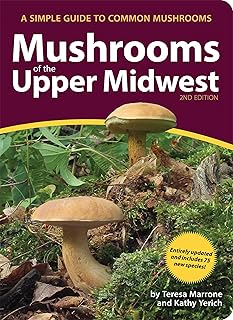
Explore related products
$17.52 $19.99
What You'll Learn
- Early Symptoms: Nausea, vomiting, diarrhea, abdominal pain, and dehydration appear within 6-24 hours after ingestion
- Neurological Signs: Confusion, dizziness, drowsiness, or hallucinations may indicate central nervous system involvement
- Delayed Symptoms: Severe cases show liver/kidney failure, jaundice, or seizures after 24-48 hours
- Amanitin Toxins: Alpha-amanitin damages liver cells, causing acute hepatitis and potential organ failure
- Treatment Steps: Immediate medical care, gastric decontamination, activated charcoal, and supportive therapy are crucial

Early Symptoms: Nausea, vomiting, diarrhea, abdominal pain, and dehydration appear within 6-24 hours after ingestion
The first signs of Amanita mushroom poisoning often mimic a stomach bug, but the timing and intensity should raise red flags. Within 6 to 24 hours of ingestion, nausea typically strikes, followed by relentless vomiting and diarrhea. This isn’t your average queasiness—it’s persistent, severe, and accompanied by sharp abdominal pain. Dehydration quickly sets in as the body loses fluids, leaving victims weak and disoriented. If you’ve recently consumed foraged mushrooms and experience these symptoms, don’t brush it off as food poisoning; it could be a life-threatening toxin at work.
Consider the scenario: a family forages mushrooms in the woods, misidentifying a deadly Amanita as an edible variety. After cooking and consuming them, the parents and children begin feeling unwell within 12 hours. The youngest, a 6-year-old, becomes severely dehydrated due to repeated vomiting and diarrhea. This rapid onset of gastrointestinal distress is a hallmark of Amanita poisoning, particularly from species like the Death Cap (*Amanita phalloides*). The toxins, known as amatoxins, target the liver and kidneys, but the initial symptoms are all in the gut. Immediate action is crucial; delaying treatment can lead to organ failure.
To manage these early symptoms, focus on hydration and monitoring. Oral rehydration solutions (ORS) can help replace lost fluids and electrolytes, but only if the person can keep liquids down. Avoid over-the-counter anti-diarrheal medications, as they can slow toxin elimination. Instead, seek medical attention immediately. Hospitals can administer activated charcoal to bind remaining toxins in the stomach and provide intravenous fluids to combat dehydration. For children or elderly individuals, who are more susceptible to rapid fluid loss, this step is non-negotiable.
Comparing Amanita poisoning to other mushroom toxicities highlights its unique danger. While some mushrooms cause immediate symptoms (within 1-2 hours), Amanita’s delayed onset can lull victims into a false sense of security. For instance, *Clitocybe* species cause diarrhea within 15-30 minutes of ingestion, but the symptoms are short-lived. Amanita’s 6-24 hour window allows toxins to circulate, causing irreversible damage if untreated. This distinction underscores why recognizing early gastrointestinal symptoms is critical—it’s the body’s last warning before the toxins wreak havoc on vital organs.
In practical terms, prevention is the best defense. Never consume wild mushrooms unless identified by a certified mycologist. Even experienced foragers make mistakes, and Amanita species often resemble edible varieties like the Paddy Straw mushroom (*Agaricus campestris*). If exposure occurs, document the mushroom’s appearance (take a photo) and save a sample for identification. This information aids medical professionals in tailoring treatment. Remember, early symptoms are your cue to act—ignore them at your peril.
Deadly Harvest: Poisonous Mushroom Fatalities and Prevention Tips
You may want to see also

Neurological Signs: Confusion, dizziness, drowsiness, or hallucinations may indicate central nervous system involvement
Confusion, dizziness, and sudden drowsiness aren’t just signs of a long day—they could signal Amanita mushroom poisoning, a condition where the central nervous system is under attack. These neurological symptoms often emerge within 6 to 24 hours after ingestion, depending on the dose and the specific Amanita species involved. For instance, the *Amanita muscaria* (fly agaric) typically causes milder symptoms compared to the deadly *Amanita phalloides* (death cap), but both can disrupt brain function. If you or someone you know experiences these symptoms after consuming wild mushrooms, immediate medical attention is critical.
Dizziness and confusion are early red flags, often mistaken for dehydration or fatigue. However, in the context of mushroom poisoning, they indicate neurotoxic compounds like ibotenic acid or muscimol interfering with neurotransmitter function. Hallucinations, though less common, are particularly alarming, as they suggest a higher toxin load or prolonged exposure. Children and elderly individuals are more susceptible due to their lower body weight and slower metabolic rates, respectively. If symptoms appear in these age groups, treat it as a medical emergency, even if the mushroom consumed was only partially toxic.
To differentiate Amanita poisoning from other causes, consider the timeline and context. Neurological symptoms typically follow gastrointestinal distress (nausea, vomiting, diarrhea), which occurs within 6–12 hours of ingestion. If confusion or drowsiness arises shortly after these initial signs, Amanita toxicity is highly probable. Keep a sample of the mushroom or take a clear photo for identification—this aids diagnosis and treatment. Avoid inducing vomiting unless directed by poison control, as it may worsen neurological symptoms in some cases.
Practical tip: If you suspect poisoning, call your local poison control center immediately. In the U.S., dial 1-800-222-1222. While waiting for help, monitor the person’s breathing and consciousness level. If hallucinations or severe confusion occur, keep the individual in a calm, safe environment to prevent injury. Remember, early intervention can mitigate long-term neurological damage or fatal outcomes.
In summary, neurological signs like confusion, dizziness, and hallucinations are not to be ignored. They are the body’s alarm system signaling Amanita’s toxins have reached the brain. Quick recognition, paired with immediate action, can save lives. When in doubt, assume the worst and seek help—mushroom poisoning is no place for hesitation.
Safely Eliminating Toxic Mushrooms: A Comprehensive Removal Guide
You may want to see also

Delayed Symptoms: Severe cases show liver/kidney failure, jaundice, or seizures after 24-48 hours
Amanita mushroom poisoning doesn’t always announce itself immediately. While some symptoms like nausea and vomiting can appear within hours, the most severe and life-threatening effects often lurk in the shadows, emerging after a deceptive lull. This delayed onset, typically 24 to 48 hours post-ingestion, is a hallmark of amatoxin poisoning, the culprit behind the deadliest Amanita species. During this window, the toxins silently infiltrate the liver and kidneys, wreaking havoc on these vital organs.
Imagine a ticking time bomb. The initial gastrointestinal symptoms might subside, lulling you into a false sense of recovery. But beneath the surface, amatoxins are binding to liver cells, disrupting their function and triggering a cascade of damage. This can lead to acute liver failure, a condition where the liver can no longer perform its essential tasks of filtering toxins and producing proteins. Similarly, kidney function may deteriorate, leading to a dangerous buildup of waste products in the bloodstream.
Jaundice, a telltale sign of liver distress, may manifest as a yellowing of the skin and eyes. This occurs when the liver fails to process bilirubin, a byproduct of red blood cell breakdown. Seizures, another alarming symptom, can arise from the brain’s exposure to toxins accumulating due to liver and kidney failure. These delayed symptoms are not merely inconveniences; they are red flags signaling a medical emergency.
If you suspect Amanita poisoning, even if initial symptoms seem mild, seek immediate medical attention. Time is of the essence. Treatment focuses on supportive care, including intravenous fluids, medications to protect the liver, and, in severe cases, liver transplantation. Remember, the absence of immediate symptoms doesn’t mean you’re out of the woods. The delayed onset of liver and kidney failure, jaundice, or seizures is a silent but deadly threat that demands vigilance and swift action.
Are Fairy Ink Cap Mushrooms Poisonous? Facts and Safety Tips
You may want to see also
Explore related products

Amanitin Toxins: Alpha-amanitin damages liver cells, causing acute hepatitis and potential organ failure
Alpha-amanitin, a potent toxin found in certain Amanita mushroom species, is a silent assassin targeting the liver with ruthless efficiency. Ingesting even a small amount—as little as 0.1 mg per kilogram of body weight—can trigger a cascade of cellular destruction. This toxin mimics the structure of a crucial enzyme involved in protein synthesis, infiltrating liver cells and halting their ability to produce essential proteins. Without these proteins, liver cells begin to die, leading to acute hepatitis, a severe inflammation of the liver.
Understanding the mechanism of alpha-amanitin’s attack underscores the urgency of recognizing symptoms and seeking immediate medical attention.
The insidious nature of alpha-amanitin poisoning lies in its delayed onset. Symptoms often appear 6 to 24 hours after ingestion, starting with gastrointestinal distress—nausea, vomiting, diarrhea, and abdominal pain. These initial signs are easily mistaken for food poisoning or a stomach virus, leading to a dangerous delay in diagnosis. As the toxin continues its assault on the liver, more severe symptoms emerge, including jaundice (yellowing of the skin and eyes), dark urine, and light-colored stools. In advanced cases, liver failure can occur within 3 to 5 days, manifesting as confusion, drowsiness, and even coma. Recognizing this progression is critical, as early intervention with treatments like activated charcoal, gastric lavage, and supportive care can significantly improve outcomes.
Comparing alpha-amanitin poisoning to other forms of mushroom toxicity highlights its severity. While some mushrooms cause immediate gastrointestinal symptoms or hallucinations, alpha-amanitin’s damage is systemic and potentially fatal. Unlike psilocybin mushrooms, which are psychoactive but rarely life-threatening, Amanita species containing alpha-amanitin require immediate medical attention. The toxin’s ability to cause irreversible liver damage sets it apart, making accurate identification of Amanita mushrooms and prompt treatment paramount. For foragers and mushroom enthusiasts, this distinction is a matter of life and death.
To protect yourself, adopt a zero-tolerance policy for wild mushroom consumption unless you are an experienced mycologist. Even experts occasionally misidentify mushrooms, so when in doubt, throw it out. If you suspect ingestion of an Amanita mushroom, act swiftly. Call poison control or seek emergency medical care immediately, bringing a sample of the mushroom for identification if possible. Time is of the essence, as early treatment can mitigate the toxin’s effects and prevent organ failure. Remember, alpha-amanitin’s silent onset and devastating impact make it a toxin to be feared and respected.
Mushroom Poisoning Timeline: Understanding Symptoms and Recovery Days
You may want to see also

Treatment Steps: Immediate medical care, gastric decontamination, activated charcoal, and supportive therapy are crucial
Amanita mushroom poisoning is a medical emergency that demands swift action. Every minute counts, as the toxins can rapidly spread through the body, causing severe damage to vital organs. Immediate medical care is non-negotiable. Call emergency services or rush to the nearest hospital without delay. Do not wait for symptoms to worsen; early intervention significantly improves outcomes.
Upon arrival at the hospital, gastric decontamination is often the first line of treatment. This process aims to remove any remaining mushroom material from the stomach to prevent further toxin absorption. Healthcare providers may induce vomiting or perform gastric lavage (stomach pumping) if ingestion occurred within the past hour. For children or individuals unable to cooperate, a nasogastric tube might be used. This step is crucial but must be performed under professional supervision to avoid complications like aspiration pneumonia.
Activated charcoal is another critical component of treatment, typically administered after gastric decontamination. This odorless, tasteless powder binds to toxins in the gastrointestinal tract, preventing their absorption into the bloodstream. The standard dose for adults is 50–100 grams, while children receive 25–50 grams, depending on age and weight. It’s most effective when given within 1–2 hours of ingestion but can still offer benefits up to 4 hours post-exposure. Be aware that charcoal can interfere with the absorption of other medications, so inform your healthcare provider about any recent drug intake.
Beyond these interventions, supportive therapy is essential to stabilize the patient and manage symptoms. Intravenous fluids are often administered to maintain hydration and support kidney function, as amanita toxins can cause severe dehydration and renal failure. Electrolyte imbalances are monitored and corrected, particularly potassium and magnesium levels. In cases of liver or kidney damage, dialysis or transplantation may be necessary. Pain management, oxygen therapy, and medications to control blood pressure are tailored to the patient’s condition. For severe cases, admission to an intensive care unit is standard to ensure continuous monitoring and rapid response to complications.
Practical tips for caregivers include keeping the patient calm and still to minimize toxin circulation, avoiding home remedies (like milk or syrup) that can delay proper treatment, and bringing a sample of the mushroom (if available) to aid identification. Time is the most critical factor, so act decisively and follow medical guidance closely. With prompt and comprehensive care, recovery from amanita poisoning is possible, but the window for effective treatment is narrow—make every second count.
Are Brown Garden Mushrooms Poisonous to Dogs? What You Need to Know
You may want to see also
Frequently asked questions
Early symptoms include nausea, vomiting, abdominal pain, and diarrhea, typically appearing 6–24 hours after ingestion.
Amanita poisoning often involves severe gastrointestinal symptoms followed by a temporary improvement, then liver and kidney failure, which is a hallmark of its toxicity.
Amanita mushrooms often have a cap with white gills, a bulbous base, and a ring (partial veil) on the stem, but identification should be left to experts as some species resemble edible mushrooms.
Seek immediate medical attention. Call poison control or go to the emergency room, bringing a sample of the mushroom if possible.
Yes, it can be fatal if untreated. Treatment should begin as soon as possible, ideally within hours of ingestion, to prevent severe liver damage.