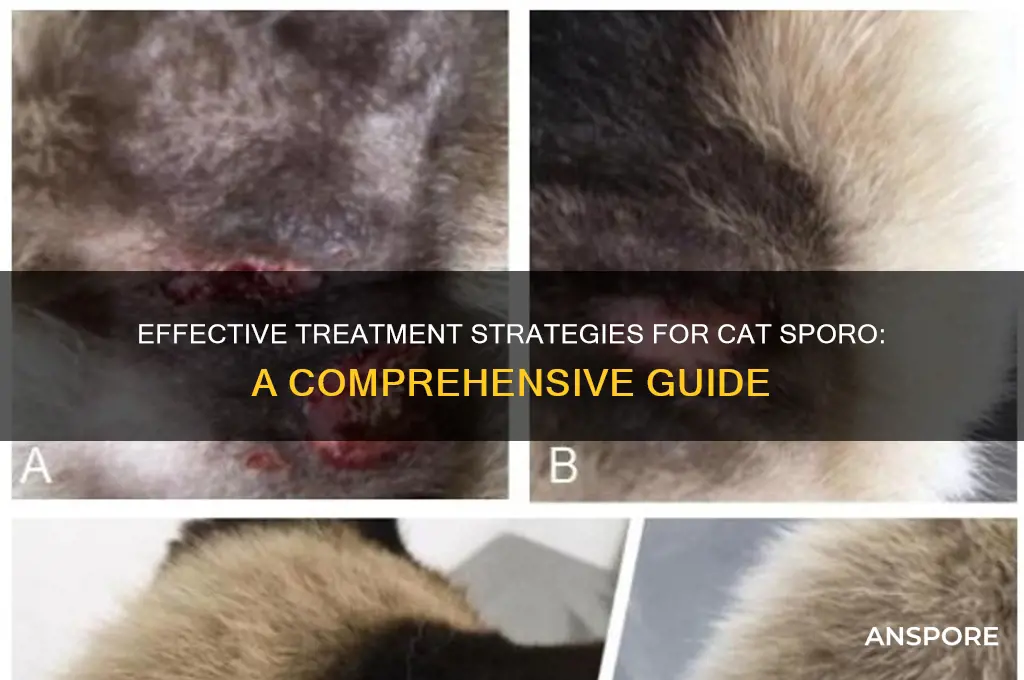
Treating cat sporo, or sporotrichosis, a fungal infection caused by *Sporothrix* species, requires a targeted approach to manage symptoms and prevent spread. Early diagnosis is crucial, as the infection can manifest as skin lesions, lymphatic involvement, or systemic disease, depending on the cat's immune response. Treatment typically involves antifungal medications such as itraconazole or potassium iodide, administered under veterinary supervision for several weeks to months. Supportive care, including wound management and environmental disinfection, is essential to reduce fungal load and prevent transmission to humans or other animals. Regular monitoring and adherence to the prescribed regimen are vital for successful recovery.
| Characteristics | Values |
|---|---|
| Disease Name | Sporotrichosis (Cat Sporo) |
| Causative Agent | Fungus Sporothrix schenckii |
| Transmission | Through contact with infected soil, plants, or bites/scratches from cats |
| Symptoms in Cats | Skin lesions, abscesses, fever, weight loss, lethargy |
| Diagnosis | Fungal culture, biopsy, PCR testing |
| Treatment for Cats | Antifungal medications (e.g., itraconazole, fluconazole) for 3-6 months |
| Treatment Duration | Typically 3-6 months, depending on severity |
| Preventive Measures | Avoid contact with infected soil/plants, treat infected cats promptly |
| Human Risk | Zoonotic (can spread to humans), especially through cat scratches/bites |
| Human Treatment | Antifungal medications (e.g., itraconazole, terbinafine) |
| Environmental Decontamination | Clean and disinfect areas where infected cats have been |
| Prognosis | Good with early and consistent treatment, poor if untreated |
| Vaccination | No vaccine available for cats or humans |
| Monitoring | Regular veterinary check-ups to monitor treatment progress |
| Isolation | Infected cats should be isolated to prevent transmission |
What You'll Learn
- Symptoms Identification: Recognize diarrhea, vomiting, lethargy, dehydration, and weight loss in infected cats
- Veterinary Diagnosis: Fecal tests confirm *Cryptosporidium*; consult a vet for accurate testing
- Hydration Management: Provide clean water, electrolytes, and IV fluids if severely dehydrated
- Medications & Treatment: Use antiparasitic drugs like nitazoxanide under vet guidance; manage symptoms
- Environmental Sanitation: Clean litter boxes, disinfect surfaces, and isolate infected cats to prevent spread

Symptoms Identification: Recognize diarrhea, vomiting, lethargy, dehydration, and weight loss in infected cats
Diarrhea in cats infected with sporotrichosis often presents as frequent, loose stools that may contain blood or mucus. This symptom can be mistaken for other gastrointestinal issues, but its persistence—lasting days or weeks—coupled with a history of potential exposure to infected soil or organic matter, should raise suspicion. Monitor stool consistency and frequency, noting any changes in color or odor. If diarrhea persists beyond 48 hours, consult a veterinarian, as prolonged episodes can lead to dehydration and electrolyte imbalances, exacerbating the cat’s condition.
Vomiting is another red flag, particularly when it occurs repeatedly or is accompanied by bile or undigested food. Unlike occasional hairball-related vomiting, sporotrichosis-induced vomiting tends to be forceful and may leave the cat visibly distressed. Keep a record of vomiting episodes, including their timing and content, to provide your vet with a clear picture. Persistent vomiting warrants immediate attention, as it can lead to rapid dehydration and nutrient depletion, especially in younger or older cats with weaker immune systems.
Lethargy in infected cats manifests as unusual inactivity, reluctance to move, or a lack of interest in play or interaction. This symptom often overlaps with other signs like fever or pain, making it a critical indicator of systemic illness. Observe your cat’s energy levels throughout the day, noting any deviations from their normal behavior. For instance, a typically active cat suddenly spending hours lying in one spot may be experiencing discomfort or weakness related to the infection.
Dehydration is a silent but dangerous consequence of diarrhea and vomiting, characterized by dry gums, sunken eyes, and reduced skin elasticity. To test for dehydration, gently pinch the skin on the back of your cat’s neck; if it doesn’t snap back quickly, dehydration is likely. Encourage water intake by providing fresh water sources and, if necessary, offering low-sodium chicken broth to entice drinking. Severe dehydration requires veterinary intervention, such as subcutaneous fluid therapy, to restore hydration levels promptly.
Weight loss in infected cats may be gradual or sudden, depending on the severity of the infection and the cat’s overall health. Regularly weigh your cat at home using a pet scale, noting any loss of more than 5% of their body weight. Combine this data with observations of appetite changes—whether they’re eating less or avoiding food altogether. Unexplained weight loss, especially in conjunction with other symptoms, signals the need for a thorough veterinary examination to diagnose and treat the underlying cause.
Mastering Hill Climbs in Spore Hero: Tips and Tricks
You may want to see also

Veterinary Diagnosis: Fecal tests confirm *Cryptosporidium*; consult a vet for accurate testing
Fecal tests are the cornerstone of diagnosing *Cryptosporidium* in cats, a parasite that can cause severe gastrointestinal distress, especially in kittens and immunocompromised felines. These tests detect oocysts, the egg-like stage of the parasite, shed in the stool. While at-home test kits may seem convenient, they often lack the sensitivity and specificity required for accurate detection. Consulting a veterinarian ensures the use of advanced techniques like fecal flotation or PCR testing, which can identify even low levels of infection. Early and precise diagnosis is critical, as *Cryptosporidium* can mimic other conditions, such as giardiasis or viral enteritis, leading to inappropriate treatment if misdiagnosed.
Once *Cryptosporidium* is confirmed, treatment focuses on managing symptoms and supporting the cat’s immune system, as there is no universally effective cure for this parasite. Vets may prescribe medications like nitazoxanide or tylosin, though their efficacy varies. For kittens under six months, extra caution is necessary, as they are more susceptible to dehydration and malnutrition due to diarrhea. Subcutaneous fluids and electrolyte supplementation are often administered to maintain hydration. Additionally, a high-calorie, easily digestible diet can help counteract weight loss and nutrient deficiencies.
A comparative analysis of treatment approaches reveals that environmental management is equally important as medical intervention. *Cryptosporidium* oocysts are highly resilient, surviving for weeks in the environment. Thorough disinfection of living areas with diluted bleach (1:10 ratio) is essential to prevent reinfection. Litter boxes, bedding, and toys should be cleaned daily, and infected cats should be isolated from healthy ones. While this may seem labor-intensive, it’s a critical step in breaking the cycle of transmission.
Persuasively, pet owners must understand that treating *Cryptosporidium* requires patience and persistence. Symptoms may persist for weeks, even with treatment, and relapses are common. Regular follow-up fecal tests are necessary to monitor oocyst shedding and assess treatment efficacy. Owners should also be prepared for the possibility of long-term management, especially in immunocompromised cats, where eradication may not be feasible. Open communication with the vet is key to tailoring a treatment plan that balances the cat’s health and the owner’s capabilities.
In conclusion, accurate veterinary diagnosis through fecal testing is the first step in addressing *Cryptosporidium* in cats. Treatment combines symptom management, immune support, and rigorous environmental disinfection. While challenging, a structured approach—guided by professional expertise—can significantly improve outcomes for affected felines.
A Beginner's Guide to Purchasing Spores from Spore Depot
You may want to see also

Hydration Management: Provide clean water, electrolytes, and IV fluids if severely dehydrated
Dehydration is a critical concern in cats with sporotrichosis, as the infection can lead to fever, lethargy, and reduced appetite, all of which contribute to fluid loss. Ensuring proper hydration is not just a supportive measure—it’s a cornerstone of treatment. Clean, fresh water should always be accessible, but this alone may not suffice for severely affected cats. Electrolyte imbalances often accompany dehydration, making replenishment a two-pronged task: restoring fluids and rebalancing essential minerals like sodium and potassium. In severe cases, intravenous (IV) fluids become indispensable, bypassing oral limitations to deliver rapid, life-sustaining hydration directly into the bloodstream.
Administering electrolytes to a cat requires precision and care. Commercial pediatric electrolyte solutions (e.g., Pedialyte) can be diluted 50/50 with water and offered in small, frequent amounts—typically 1–2 teaspoons every 1–2 hours for a 10-pound cat. Avoid solutions with artificial sweeteners like xylitol, which are toxic to cats. For kittens or older cats, consult a veterinarian for age-specific dosages, as their needs differ significantly. Electrolyte pastes, available at pet supply stores, can also be used, but monitor for gastrointestinal upset, as some cats tolerate these products poorly. Always pair electrolyte supplementation with encouragement to drink water, as electrolytes alone do not hydrate.
IV fluid therapy is reserved for cats with severe dehydration, characterized by symptoms like sunken eyes, dry gums, or prolonged skin tenting. This intervention is strictly veterinary-administered, as it requires precise calculation of fluid rates based on the cat’s weight, hydration status, and underlying health conditions. Typically, a cat receives 60–100 ml/kg of fluids over 24 hours, delivered via a catheter placed in a vein or under the skin (subcutaneously). IV fluids not only correct dehydration but also support organ function by maintaining blood pressure and aiding toxin elimination. Hospitalization may be necessary for continuous monitoring during this phase.
Practical tips for home hydration management include warming water slightly (to room temperature) to make it more appealing, using shallow bowls to prevent whisker fatigue, and placing multiple water stations throughout the house. For cats resistant to drinking, wet food can contribute to fluid intake, though it should not replace water entirely. Humidifiers can also ease respiratory discomfort in cats with sporotrichosis, indirectly encouraging hydration by reducing fever-related fluid loss. Above all, monitor urine output and gum moisture daily—signs of improvement include increased urination and moist, pink gums, while persistent dryness warrants immediate veterinary attention.
Comparatively, while oral rehydration is effective for mild to moderate cases, it pales against the immediacy of IV fluids in critical scenarios. The key takeaway is this: hydration management is not one-size-fits-all. Tailor the approach to the cat’s condition, balancing accessibility with urgency. Clean water forms the foundation, electrolytes address imbalances, and IV fluids serve as the last line of defense. Each step, when executed thoughtfully, transforms hydration from a passive measure into an active, life-preserving strategy in the fight against sporotrichosis.
Outdoor Mushroom Cultivation: A Step-by-Step Guide to Growing from Spores
You may want to see also

Medications & Treatment: Use antiparasitic drugs like nitazoxanide under vet guidance; manage symptoms
Antiparasitic medications are the cornerstone of treating cat sporotrichosis, a fungal infection often contracted through soil or plant material. Nitazoxanide, a broad-spectrum antiparasitic drug, has shown promise in managing this condition, but its use requires careful veterinary oversight. Unlike traditional antifungal treatments, nitazoxanide targets the metabolic pathways of the Sporothrix fungus, disrupting its ability to thrive in the host. This mechanism makes it a valuable option, especially in cases where conventional therapies fall short. However, its efficacy and safety in cats are still under study, emphasizing the need for professional guidance before administration.
Administering nitazoxanide to cats involves precise dosing tailored to the animal’s weight and severity of infection. Typically, veterinarians prescribe 25–50 mg/kg of body weight, given orally twice daily. For a 5-kg cat, this translates to approximately 125–250 mg per dose. It’s crucial to follow the vet’s instructions meticulously, as underdosing may prolong treatment, while overdosing can lead to gastrointestinal side effects like diarrhea or vomiting. The medication is often compounded into a liquid or flavored suspension to improve palatability, as cats can be notoriously finicky about pills.
While nitazoxanide addresses the root cause, managing symptoms is equally vital for the cat’s comfort and recovery. Lesions, a common symptom of sporotrichosis, should be kept clean and dry to prevent secondary bacterial infections. Warm compresses can soothe inflamed areas, and topical antibiotics may be applied under veterinary direction. Cats with systemic symptoms, such as fever or lethargy, may benefit from supportive care like fluid therapy or appetite stimulants. Monitoring the cat’s progress through regular check-ups ensures the treatment plan remains effective and adjustments can be made as needed.
The decision to use nitazoxanide should be weighed against potential risks and alternatives. Pregnant or nursing cats, as well as kittens under six months, may require modified dosing or alternative treatments due to limited safety data. Additionally, drug interactions with other medications must be considered, particularly if the cat is on long-term therapies. Compared to traditional antifungals like itraconazole, nitazoxanide offers a potentially shorter treatment duration but lacks the extensive research backing of older drugs. This comparative analysis highlights the importance of individualized treatment plans crafted by a veterinarian.
In conclusion, treating cat sporotrichosis with nitazoxanide is a targeted approach that requires precision and vigilance. From accurate dosing to symptom management, every step plays a critical role in ensuring a successful outcome. While this medication shows promise, it is not a one-size-fits-all solution, and its use must be guided by professional expertise. By combining antiparasitic therapy with supportive care, cat owners can effectively combat this infection and restore their pet’s health. Always consult a veterinarian to tailor the treatment to your cat’s specific needs.
C. Diff Spores on Clothes: Survival Duration and Prevention Tips
You may want to see also

Environmental Sanitation: Clean litter boxes, disinfect surfaces, and isolate infected cats to prevent spread
Spores of *Sporothrix schenckii*, the fungus causing sporotrichosis in cats, are remarkably resilient, surviving for months in the environment. This tenacity underscores the critical role of environmental sanitation in breaking the chain of infection. A single contaminated litter box or scratched surface can become a reservoir, silently spreading the fungus to other pets or humans. Thus, meticulous cleaning and disinfection are not optional—they are essential.
Begin with the litter box, the epicenter of potential contamination. Replace all litter immediately, as spores cling to substrates. Use a 1:10 dilution of household bleach (approximately 1 cup bleach per gallon of water) to scrub the box thoroughly, ensuring all surfaces are saturated. Allow it to sit for 10 minutes before rinsing and drying completely. For multi-cat households, consider using disposable litter boxes during the treatment period to minimize cross-contamination. Repeat this process daily until the infected cat has completed at least two weeks of antifungal therapy, as spores continue to shed during treatment.
Surfaces in the cat’s environment—floors, furniture, and scratching posts—require equal attention. Vacuum daily to remove loose spores, disposing of the vacuum bag immediately afterward to prevent recontamination. Follow vacuuming with disinfection using the same bleach solution, paying special attention to areas where the cat scratches or rests. For wooden or delicate surfaces, a 70% isopropyl alcohol solution can be used as an alternative, though it may require more frequent application. Discard or thoroughly clean any fabric items, such as bedding or toys, that cannot be disinfected effectively.
Isolation of the infected cat is a non-negotiable measure to prevent spread. Confine the cat to a single room with minimal furnishings, ideally with a washable floor. Limit handling and wear gloves when cleaning or administering medication, as spores can adhere to skin and clothing. If multiple cats share the household, ensure the infected cat remains separated until fungal cultures confirm clearance, typically after 3–4 weeks of treatment. This isolation not only protects other pets but also reduces environmental contamination, making cleanup more manageable.
The rigor of these sanitation practices may seem daunting, but their impact is profound. A study in veterinary dermatology found that households implementing strict environmental disinfection protocols reduced the risk of secondary infections by 85%. Consistency is key—sporadic cleaning leaves gaps for spores to persist. By treating the environment as an extension of the cat’s treatment plan, caregivers can transform a potentially hazardous space into a safe haven, accelerating recovery and safeguarding all inhabitants.
Unveiling the Fascinating Methods of Morel Mushroom Spore Dispersal
You may want to see also
Frequently asked questions
Cat sporo, or sporotrichosis, is a fungal infection caused by the Sporothrix fungus. Symptoms include skin lesions, abscesses, fever, and weight loss. If you notice any of these signs, consult your veterinarian for a proper diagnosis.
Treatment typically involves antifungal medications prescribed by a veterinarian, such as itraconazole or potassium iodide. The duration of treatment can range from several weeks to months, depending on the severity of the infection.
Yes, sporotrichosis is zoonotic, meaning it can spread from animals to humans through direct contact with infected wounds or spores. It can also spread to other pets. Practice good hygiene and avoid touching lesions to minimize transmission risk.