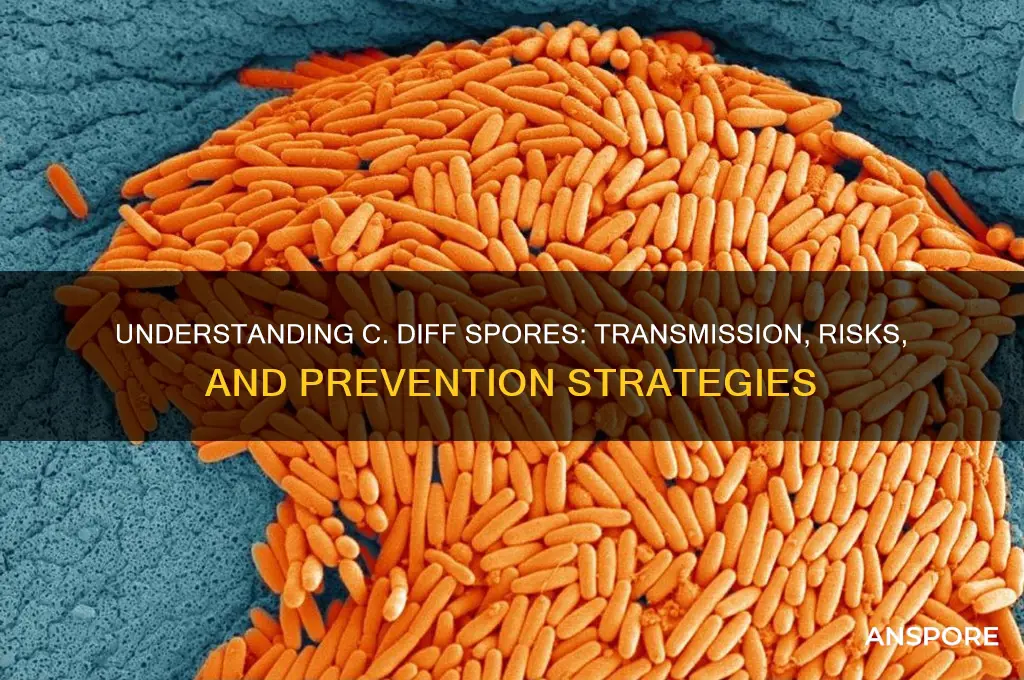
*Clostridioides difficile*, commonly known as C. diff, is a bacterium that can cause severe intestinal infections, particularly in individuals with compromised immune systems or those who have recently undergone antibiotic treatment. One of the most concerning aspects of C. diff is its ability to produce highly resilient spores, which can survive for extended periods in various environments, including hospital surfaces and medical equipment. These spores are a key factor in the transmission and persistence of C. diff infections, as they can remain dormant until they encounter favorable conditions within a host's gastrointestinal tract. Understanding the nature of C. diff spores, their resistance mechanisms, and their role in disease spread is crucial for developing effective prevention and treatment strategies to combat this significant public health threat.
| Characteristics | Values |
|---|---|
| Definition | C. diff spores are dormant, highly resistant forms of Clostridioides difficile bacteria. |
| Shape | Oval or spherical. |
| Size | Approximately 0.5 to 2.0 micrometers in diameter. |
| Resistance | Highly resistant to heat, drying, antibiotics, and disinfectants. |
| Survival | Can survive for months to years in the environment. |
| Germination | Require specific conditions (e.g., bile salts, nutrients) to germinate into active bacteria. |
| Transmission | Spread via fecal-oral route, often through contaminated surfaces or hands. |
| Infection Risk | Primarily infect individuals with disrupted gut microbiota (e.g., after antibiotic use). |
| Disease | Cause C. difficile infection (CDI), leading to diarrhea, colitis, or pseudomembranous colitis. |
| Detection | Detected through stool tests (e.g., toxin assays, PCR, or culture). |
| Disinfection | Require spore-killing agents like chlorine bleach (10% solution) for effective disinfection. |
| Prevention | Hand hygiene, environmental cleaning, and judicious antibiotic use. |
| Treatment | Treated with specific antibiotics (e.g., vancomycin, fidaxomicin) and fecal microbiota transplantation (FMT) in severe cases. |
| Public Health Impact | Leading cause of healthcare-associated infections worldwide. |
What You'll Learn
- Transmission Methods: How C. diff spores spread via fecal-oral route, contaminated surfaces, and healthcare settings
- Survival Duration: C. diff spores can persist in environments for months, resisting standard cleaning agents
- Risk Factors: Antibiotic use, hospitalization, weakened immunity, and age increase susceptibility to C. diff infection
- Detection Techniques: PCR, toxin assays, and stool culture methods identify C. diff spores in patients
- Prevention Strategies: Hand hygiene, isolation precautions, and environmental disinfection reduce spore transmission effectively

Transmission Methods: How C. diff spores spread via fecal-oral route, contaminated surfaces, and healthcare settings
C. diff spores are remarkably resilient, capable of surviving on surfaces for months, making them a persistent threat in various environments. These spores primarily spread through the fecal-oral route, a pathway that underscores the importance of hygiene in preventing infection. When an individual infected with *Clostridioides difficile* (C. diff) has a bowel movement, the spores are shed in the feces. If proper hand hygiene is not practiced, these spores can easily transfer to hands and then to the mouth, either directly or via contaminated objects. This route is particularly concerning in settings where personal care is frequent, such as households and long-term care facilities.
Contaminated surfaces act as silent carriers of C. diff spores, amplifying their spread beyond direct person-to-person contact. Common touchpoints like doorknobs, bedrails, and bathroom fixtures can harbor spores, especially in healthcare settings where cleaning protocols may not always eliminate them. Unlike vegetative bacteria, C. diff spores are resistant to many standard disinfectants, including alcohol-based hand sanitizers. Instead, surfaces must be cleaned with spore-killing agents like chlorine bleach solutions (1:10 dilution of household bleach) to effectively reduce contamination. Failure to do so can lead to repeated exposure, even in environments that appear clean.
Healthcare settings are hotspots for C. diff transmission due to the convergence of vulnerable patients, frequent procedures, and high spore prevalence. Patients on antibiotics are particularly at risk, as these medications disrupt gut flora, allowing C. diff to flourish. Healthcare workers can inadvertently spread spores between patients if they do not adhere to strict hand hygiene protocols, such as washing with soap and water followed by glove changes between patient interactions. Additionally, medical equipment and devices that are not properly sterilized can become vectors for transmission. Hospitals must implement robust infection control measures, including isolating infected patients and dedicating staff to their care, to minimize spread.
Preventing C. diff transmission requires a multi-faceted approach tailored to the specific risks of each setting. In households, caregivers should wear gloves when assisting infected individuals and wash hands thoroughly with soap and water after removal. Surfaces should be cleaned daily with bleach-based solutions, focusing on high-touch areas. In healthcare, adherence to contact precautions is non-negotiable, and staff should be trained to recognize the risks of antibiotic overuse. Patients and families must also be educated on the importance of hand hygiene and the role of spores in persistent infections. By addressing each transmission route—fecal-oral, contaminated surfaces, and healthcare practices—the spread of C. diff can be significantly mitigated.
Can Black Mold Spores Penetrate Tape? Uncovering the Truth
You may want to see also

Survival Duration: C. diff spores can persist in environments for months, resisting standard cleaning agents
C. diff spores are notorious for their resilience, capable of surviving on surfaces for months, even in the face of routine cleaning efforts. This tenacity poses a significant challenge in healthcare settings, where the spores can silently persist on bed rails, doorknobs, and medical equipment, waiting to infect vulnerable patients. Unlike many pathogens that succumb quickly to disinfectants, C. diff spores require specialized cleaning agents and meticulous protocols to ensure their eradication.
Consider the typical hospital environment: a bustling hub of activity where surfaces are frequently touched but not always thoroughly disinfected. Standard cleaning agents, such as those containing quaternary ammonium compounds, are ineffective against C. diff spores. These spores have a tough outer layer that protects them from desiccation, heat, and chemicals, allowing them to remain viable long after their bacterial counterparts have perished. For instance, studies have shown that C. diff spores can survive on surfaces for up to five months, even in dry conditions.
To combat this persistence, healthcare facilities must adopt a two-pronged approach. First, use EPA-approved sporocidal disinfectants, such as those containing chlorine bleach (at a concentration of 1,000–5,000 ppm) or hydrogen peroxide. These agents are proven to destroy C. diff spores effectively. Second, implement rigorous cleaning protocols that focus on high-touch surfaces and patient care areas. For example, after a patient with C. diff is discharged, the room should undergo terminal cleaning with a sporocidal agent, followed by thorough drying to ensure maximum efficacy.
The implications of C. diff spore survival extend beyond hospitals. Long-term care facilities, outpatient clinics, and even homes can become reservoirs for these spores if proper cleaning measures are not taken. For caregivers and family members, this means adopting hospital-grade disinfection practices, particularly when caring for individuals at high risk of infection, such as the elderly or immunocompromised. Practical tips include wearing gloves during cleaning, using disposable cloths to avoid cross-contamination, and ensuring adequate contact time for disinfectants (typically 10 minutes for bleach solutions).
In summary, the survival duration of C. diff spores demands a proactive and informed response. By understanding their resistance to standard cleaning agents and implementing targeted disinfection strategies, we can significantly reduce the risk of transmission. This is not merely a matter of hygiene but a critical component of infection prevention, safeguarding both patients and communities from the devastating effects of C. diff infections.
Simplify Your Spore Creations: Removing the Complexity Meter Easily
You may want to see also

Risk Factors: Antibiotic use, hospitalization, weakened immunity, and age increase susceptibility to C. diff infection
Antibiotics, while lifesaving, disrupt the delicate balance of gut flora, creating fertile ground for *Clostridioides difficile* (C. diff) spores to flourish. Broad-spectrum antibiotics like clindamycin, fluoroquinolones, and cephalosporins are particularly notorious for decimating beneficial bacteria, leaving the gut vulnerable. Even a single course of antibiotics can increase C. diff risk by 7-10 times, with prolonged or repeated use amplifying this danger. For instance, a 10-day course of amoxicillin-clavulanate elevates risk significantly compared to shorter regimens. To mitigate this, healthcare providers should prescribe antibiotics judiciously, opting for narrow-spectrum options when possible and considering probiotic co-therapy to restore gut equilibrium.
Hospitals, paradoxically, are hotspots for C. diff transmission due to high concentrations of vulnerable patients and persistent spore contamination. Extended hospital stays, invasive procedures, and frequent antibiotic use create a perfect storm for infection. Studies show that patients hospitalized for over two weeks face a 3-fold increased risk compared to shorter stays. Environmental factors play a critical role: C. diff spores can survive on surfaces for months, resisting standard cleaning agents. Practical measures include rigorous hand hygiene with soap and water (not just alcohol-based sanitizers, which are ineffective against spores), isolating infected patients, and using bleach-based disinfectants for surface cleaning.
A weakened immune system, whether from conditions like HIV, cancer, or immunosuppressive medications, diminishes the body’s ability to combat C. diff spores. For example, organ transplant recipients on corticosteroids or chemotherapy patients experience a 2-4 times higher risk of infection. Similarly, individuals with inflammatory bowel disease (IBD) face heightened susceptibility due to gut inflammation and frequent antibiotic exposure. To reduce risk, immunocompromised individuals should avoid unnecessary antibiotics, maintain good hygiene, and promptly report diarrhea or gastrointestinal symptoms to their healthcare provider for early testing and treatment.
Age is a non-negotiable risk factor, with individuals over 65 facing a 10-20 times higher risk of C. diff infection compared to younger adults. Aging weakens the immune system, reduces stomach acid production (a natural barrier to pathogens), and increases the likelihood of hospitalization and antibiotic use. Nursing home residents are particularly vulnerable due to communal living and high antibiotic prescription rates. Preventive strategies include annual flu and pneumonia vaccinations to reduce infection-related antibiotic use, regular handwashing, and ensuring healthcare facilities follow strict infection control protocols. For older adults, even mild diarrhea warrants medical attention to rule out C. diff.
Quaternary Ammonium Compounds: Effective Against Spores or Limited Disinfection?
You may want to see also

Detection Techniques: PCR, toxin assays, and stool culture methods identify C. diff spores in patients
Clostridioides difficile (C. diff) spores are a persistent threat in healthcare settings, capable of surviving for months on surfaces and resisting routine disinfection. Detecting these spores in patients is critical for timely intervention, as they can lead to severe infections, particularly in immunocompromised individuals or those on prolonged antibiotic therapy. Three primary techniques—PCR, toxin assays, and stool culture methods—each offer unique advantages and limitations in identifying C. diff spores, making them essential tools in clinical diagnostics.
PCR (Polymerase Chain Reaction) stands out for its speed and sensitivity, amplifying specific DNA sequences to detect C. diff spores within hours. This method is particularly useful in acute care settings where rapid results are crucial. For instance, PCR can identify the presence of C. diff in stool samples with a sensitivity of up to 95%, often outperforming other methods in early-stage infections. However, PCR’s ability to detect spores specifically, rather than just the organism’s DNA, depends on the primer design. Laboratories must use primers targeting genes unique to toxigenic strains, such as *tcdB*, to ensure accurate identification. A key caution is that PCR may yield false positives if the sample contains non-viable spores or DNA remnants, necessitating clinical correlation.
Toxin assays, on the other hand, focus on detecting toxins A and B, which are directly responsible for C. diff-associated diarrhea. These assays are available in enzyme immunoassay (EIA) formats, offering results within 1–2 hours. While toxin assays are less sensitive than PCR, they are highly specific for active infection, as the presence of toxins indicates viable, toxin-producing organisms. A limitation is their inability to detect toxin-negative strains, which account for 5–10% of C. diff cases. For optimal use, toxin assays should be paired with PCR or culture methods, especially in patients with high clinical suspicion but negative initial results.
Stool culture methods remain the gold standard for confirming C. diff spore viability. This technique involves culturing stool samples on selective media, such as cycloserine-cefoxitin-fructose agar (CCFA), followed by identification through anaerobic incubation and toxin testing. While stool culture is highly specific, it is time-consuming, requiring 48–72 hours for results. Its primary advantage is the ability to isolate and characterize the organism, including antibiotic susceptibility testing, which is invaluable for treatment planning. However, stool culture is less sensitive than PCR, particularly for low-burden infections, and requires specialized laboratory expertise.
In practice, a tiered approach often yields the best outcomes. For example, PCR can serve as an initial screening tool due to its rapid turnaround, followed by toxin assays to confirm active toxin production. Stool culture may be reserved for complex cases, such as recurrent infections or epidemiological investigations. Clinicians should also consider patient factors, such as recent antibiotic exposure or severity of symptoms, when selecting the most appropriate method. For instance, in a 70-year-old patient with severe diarrhea following a course of broad-spectrum antibiotics, PCR and toxin assays should be prioritized for immediate diagnosis, while stool culture may be deferred unless recurrence is suspected.
Ultimately, the choice of detection technique depends on the clinical context, laboratory capabilities, and urgency of results. Each method—PCR, toxin assays, and stool culture—complements the others, providing a comprehensive toolkit for identifying C. diff spores and guiding effective patient management. By understanding their strengths and limitations, healthcare providers can optimize diagnostic accuracy and improve outcomes for patients at risk of C. diff infection.
Surviving the Flames: Can Spores Endure Wildfires and Heat?
You may want to see also

Prevention Strategies: Hand hygiene, isolation precautions, and environmental disinfection reduce spore transmission effectively
Hand hygiene stands as the first line of defense against *C. diff* spore transmission. Unlike routine handwashing, which targets transient flora, combating *C. diff* requires alcohol-based hand sanitizers with at least 60% alcohol content, proven to disrupt spore viability. However, alcohol’s efficacy wanes against spores, making soap-and-water handwashing critical post-patient contact. This dual approach—alcohol for general hygiene, soap for spore removal—is non-negotiable in healthcare settings. For instance, a 2015 study in *Infection Control & Hospital Epidemiology* demonstrated that alcohol alone reduced *C. diff* spores by only 30%, while soap-and-water washing achieved a 90% reduction.
Isolation precautions act as a containment barrier, limiting spore spread in healthcare environments. Contact precautions, including gloves and gowns, are mandatory for patients with *C. diff* infection (CDI). Dedicating equipment to individual patients further minimizes cross-contamination. For example, a 2017 *Journal of Hospital Infection* study found that facilities implementing strict isolation protocols reduced CDI rates by 40%. Notably, these measures must extend beyond the patient’s room; spores can persist on healthcare workers’ attire, underscoring the need for meticulous donning and doffing procedures.
Environmental disinfection targets the silent reservoir of *C. diff* spores on surfaces. Standard cleaning agents often fail against spores, necessitating EPA-registered disinfectants with sporicidal activity, such as chlorine-based solutions (1,000–5,000 ppm) or accelerated hydrogen peroxide. Daily disinfection of high-touch surfaces—bed rails, doorknobs, and toilets—is critical, with extended contact times (e.g., 10 minutes for bleach) to ensure spore eradication. A 2019 *American Journal of Infection Control* study revealed that enhanced environmental cleaning reduced surface spore counts by 80%, correlating with a 35% drop in CDI cases.
Integrating these strategies requires a systemic approach, not isolated efforts. Hand hygiene compliance must be monitored via audits, with feedback loops to improve adherence. Isolation protocols demand staff training to prevent breaches, such as reusing stethoscopes between patients. Environmental teams should employ fluorescent markers to validate cleaning efficacy, ensuring no surface is overlooked. Collectively, these measures form a synergistic defense, as evidenced by a 2020 *Lancet Infectious Diseases* meta-analysis, which attributed a 50% reduction in CDI rates to multifaceted prevention programs. Without this triad—hand hygiene, isolation, disinfection—spore transmission remains an insidious threat in healthcare settings.
Is Buying Shroom Spores Legal? Understanding the Laws and Risks
You may want to see also
Frequently asked questions
C. diff spores are the dormant, highly resistant form of the bacterium Clostridioides difficile. They are produced by the bacteria as a survival mechanism and can persist in the environment for long periods, even withstanding harsh conditions like heat, dryness, and many disinfectants.
C. diff spores are primarily transmitted through the fecal-oral route. They can be spread by touching contaminated surfaces or objects and then touching the mouth, or by ingesting food or water contaminated with the spores. Healthcare settings are common places for transmission due to the presence of vulnerable patients and frequent use of antibiotics.
C. diff spores themselves do not cause infection; they must first germinate into the active, vegetative form of the bacteria. This typically occurs in the colon when the normal gut flora is disrupted, often due to antibiotic use, allowing C. diff to multiply and produce toxins that cause illness.
C. diff spores can survive in the environment for weeks to months, depending on conditions. They are highly resilient and can remain viable on surfaces like countertops, bedrails, and medical equipment, posing a risk of infection if not properly cleaned and disinfected.
C. diff spores require specialized cleaning and disinfection methods. Using EPA-registered spore-killing disinfectants with active ingredients like chlorine bleach (sodium hypochlorite) is recommended. Surfaces should be thoroughly cleaned to remove organic matter before disinfection, as spores are more resistant when protected by debris.







