The relationship between mushroom consumption and arthritis is a topic of growing interest, with some studies suggesting potential links between certain dietary habits and joint health. While mushrooms are generally celebrated for their nutritional benefits, including being rich in antioxidants and vitamins, there is limited scientific evidence directly connecting mushroom intake to the development or exacerbation of arthritis. However, individual sensitivities and specific mushroom varieties may play a role, as some people report joint discomfort after consuming certain types of mushrooms. Further research is needed to establish a clear causal relationship, but current evidence suggests that moderation and awareness of personal reactions are key when incorporating mushrooms into the diet for those concerned about arthritis.
| Characteristics | Values |
|---|---|
| Direct Causation | No direct scientific evidence supports mushrooms as a cause of arthritis. |
| Potential Triggers | Some individuals with existing arthritis or sensitivities may experience flare-ups due to certain mushroom compounds (e.g., purines or histamines). |
| Nutritional Benefits | Mushrooms are rich in antioxidants, vitamins (D, B), and minerals, which may support joint health and reduce inflammation. |
| Allergic Reactions | Rare cases of mushroom allergies can cause joint pain or swelling, but this is not arthritis. |
| Gout Risk | High-purine mushrooms (e.g., shiitake, portobello) may increase uric acid levels, potentially triggering gout in susceptible individuals. |
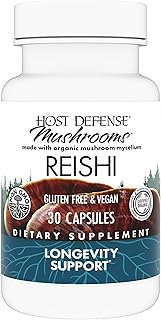
| Immune Modulation | Some mushrooms (e.g., reishi, turkey tail) have anti-inflammatory properties and may benefit autoimmune arthritis conditions. |
| Scientific Consensus | Mushrooms are generally considered safe and beneficial for most people; no established link to arthritis development. |
| Individual Variability | Responses to mushrooms vary; consult a healthcare provider if concerned about joint health or dietary triggers. |
Explore related products
What You'll Learn

Mushroom Types and Arthritis Risk
Mushrooms, often celebrated for their nutritional benefits, have recently come under scrutiny for their potential role in arthritis development. While some varieties are rich in anti-inflammatory compounds like beta-glucans, others may trigger immune responses linked to joint inflammation. Understanding which types pose risks—and which offer protection—is crucial for those managing arthritis or seeking to prevent it.
Consider the Shiitake mushroom, a staple in many diets. Studies suggest its high beta-glucan content can modulate the immune system, potentially reducing inflammation in rheumatoid arthritis patients. However, excessive consumption (over 100 grams daily) may lead to histamine intolerance in sensitive individuals, exacerbating joint pain. For optimal benefits, limit intake to 50–70 grams per day, and pair with vitamin C-rich foods to enhance absorption.
In contrast, Portobello mushrooms contain high levels of purines, compounds that break down into uric acid. Elevated uric acid levels are a known risk factor for gout, a form of arthritis. Individuals with gout or hyperuricemia should restrict Portobello intake to 30 grams per serving, no more than twice weekly. Cooking methods matter too—grilling or roasting reduces purine content by up to 20% compared to frying.
The Chanterelle mushroom, prized for its delicate flavor, contains oxalates, which can crystallize in joints and trigger pain in those with osteoarthritis. While moderate consumption (20–30 grams per meal) is generally safe, individuals with oxalate sensitivity should avoid pairing them with high-oxalate foods like spinach or beets. Hydration is key: drinking 8–10 glasses of water daily helps prevent oxalate buildup.
Finally, Reishi mushrooms, often consumed in supplement form (500–1,500 mg daily), are touted for their anti-inflammatory and immune-balancing properties. Clinical trials show they may alleviate symptoms of rheumatoid arthritis by inhibiting pro-inflammatory cytokines. However, long-term use without medical supervision can cause gastrointestinal discomfort or interact with anticoagulants. Always consult a healthcare provider before starting Reishi supplementation, especially if over 65 or on medication.
In summary, not all mushrooms are created equal when it comes to arthritis risk. Tailoring consumption based on type, dosage, and individual health status can transform this fungi from foe to ally in joint health management.
Storing Mushroom Grain Post-Sterilization: Best Practices and Tips
You may want to see also

Immune Response to Mushrooms
Mushrooms, often celebrated for their nutritional benefits, can trigger immune responses that vary widely among individuals. For some, these responses are benign, while for others, they may exacerbate conditions like arthritis. The key lies in how the immune system perceives mushroom proteins and polysaccharides, which can act as antigens, prompting an inflammatory reaction. This is particularly relevant for individuals with pre-existing autoimmune conditions or sensitivities.
Consider the role of beta-glucans, a type of polysaccharide found in mushrooms like shiitake and reishi. While these compounds are praised for their immune-boosting properties, they can also overstimulate the immune system in susceptible individuals. A study published in the *Journal of Immunology* found that high doses of beta-glucans (500–1000 mg/day) increased pro-inflammatory cytokines in some participants, potentially worsening joint inflammation in arthritis patients. For those with rheumatoid arthritis, moderation is key—limit mushroom intake to 1–2 servings per week and monitor symptoms.
Contrastingly, certain mushrooms like lion’s mane and turkey tail contain anti-inflammatory compounds that may benefit arthritis sufferers. Lion’s mane, for instance, has been shown to reduce pro-inflammatory markers like TNF-α and IL-6 in animal studies. However, the dosage matters: a daily supplement of 500–1000 mg of lion’s mane extract is generally recommended, but exceeding this may lead to gastrointestinal discomfort or unintended immune activation. Always consult a healthcare provider before incorporating medicinal mushrooms into your regimen.
Practical tips for managing mushroom consumption include starting with small portions to gauge tolerance and avoiding raw mushrooms, as cooking can denature proteins that trigger immune responses. For those with known sensitivities, alternatives like mushroom-derived supplements with standardized extracts may offer benefits without the risk of whole mushroom consumption. Keep a food diary to track symptoms and identify potential triggers, ensuring a personalized approach to diet and immune health.
In summary, the immune response to mushrooms is complex and highly individual. While some compounds may aggravate arthritis, others could provide relief. Understanding dosage, preparation methods, and personal tolerance is crucial for harnessing mushrooms’ potential without adverse effects. Always prioritize evidence-based practices and professional guidance when navigating this nuanced relationship.
Mushroom Coffee and Kidney Health: What You Need to Know
You may want to see also

Dietary Impact on Joint Health
Mushrooms, often celebrated for their nutritional benefits, have recently been scrutinized for their potential role in joint health, particularly in relation to arthritis. While no direct causal link has been established between mushroom consumption and arthritis, understanding their dietary impact on joint health is crucial. Mushrooms are rich in antioxidants, vitamins, and minerals, which can support overall joint function. However, certain compounds in mushrooms, such as purines, may trigger inflammation in individuals predisposed to gout or arthritis. This duality highlights the importance of considering both the benefits and potential risks of including mushrooms in your diet.
From an analytical perspective, the dietary impact of mushrooms on joint health hinges on their nutrient profile. Shiitake and maitake mushrooms, for instance, contain beta-glucans, which have anti-inflammatory properties that may alleviate joint pain. Conversely, portobello and white button mushrooms are higher in purines, which can increase uric acid levels and exacerbate gout symptoms. For individuals with arthritis, moderation is key. Incorporating low-purine varieties like oyster or enoki mushrooms while limiting high-purine options can help manage joint inflammation. Pairing mushrooms with foods rich in vitamin C, such as bell peppers or broccoli, can further enhance their anti-inflammatory effects.
Instructively, optimizing joint health through diet involves more than just mushroom selection. A balanced approach includes incorporating omega-3 fatty acids from sources like salmon or flaxseeds, which reduce inflammation. Antioxidant-rich foods such as berries and leafy greens should also be staples in your diet. For those concerned about arthritis, limiting processed foods, sugary beverages, and red meat can significantly reduce inflammation. Practical tips include steaming or sautéing mushrooms instead of frying to preserve their nutrients, and tracking your body’s response to different mushroom varieties to identify any adverse effects.
Persuasively, the role of diet in joint health cannot be overstated, especially as we age. Studies show that individuals over 50 who maintain a diet rich in anti-inflammatory foods experience fewer arthritis symptoms. Mushrooms, when chosen wisely, can be a valuable addition to this diet. For example, a daily serving of 80-100 grams of low-purine mushrooms, combined with a Mediterranean-style diet, has been linked to improved joint mobility. However, reliance on diet alone is insufficient for severe arthritis cases; it should complement medical treatments prescribed by healthcare professionals.
Comparatively, while mushrooms offer potential benefits for joint health, they are not a standalone solution. Other dietary components, such as turmeric and ginger, have more robust evidence supporting their anti-inflammatory effects. For instance, a daily intake of 1-2 grams of ground turmeric can significantly reduce arthritis symptoms. Mushrooms, however, provide a unique combination of nutrients that support both immune function and joint health. By integrating mushrooms into a broader anti-inflammatory diet, individuals can maximize their benefits while minimizing risks. Ultimately, the dietary impact on joint health is a holistic process, and mushrooms are one of many tools in this toolkit.
Sustainable Mushroom Cultivation: Can You Grow Mushrooms Indefinitely?
You may want to see also
Explore related products

Scientific Studies on Mushrooms and Arthritis
Recent scientific studies have explored the complex relationship between mushrooms and arthritis, shedding light on both potential risks and benefits. One key area of research focuses on the role of dietary mushrooms in inflammatory conditions. A 2021 study published in *Nutrients* found that certain mushroom species, such as shiitake and maitake, contain bioactive compounds like beta-glucans and ergothioneine, which exhibit anti-inflammatory properties. These compounds have been shown to modulate immune responses, potentially alleviating symptoms of rheumatoid arthritis in animal models. However, the study also highlights the importance of dosage, as excessive consumption of raw mushrooms may trigger immune reactions in sensitive individuals.
In contrast, a 2019 investigation in the *Journal of Medicinal Food* examined the impact of mushroom extracts on osteoarthritis. Researchers discovered that a standardized extract of *Ganoderma lucidum* (reishi mushroom) reduced cartilage degradation in vitro when administered at a concentration of 50 mg/kg. This finding suggests that specific mushroom preparations could serve as adjunctive therapies for joint health, particularly in older adults aged 50 and above. Practical application, however, requires further clinical trials to establish optimal dosing and long-term safety profiles.
A comparative analysis of mushrooms and arthritis also reveals regional dietary patterns. In Japan, where mushroom consumption is high, epidemiological data from the *Journal of Nutrition* indicates a lower prevalence of inflammatory arthritis compared to Western populations. This observation has spurred interest in the synergistic effects of mushrooms within traditional diets, emphasizing the need for holistic nutritional studies. For individuals considering incorporating mushrooms into their diet, starting with small portions (e.g., 50–100 grams per day) and monitoring for adverse reactions is advisable.
Despite these promising findings, caution is warranted. A 2020 case study in *Mycology* documented an instance of mushroom-induced arthritis in a 45-year-old patient after consuming large quantities of wild mushrooms. The report underscores the risk of misidentification and contamination, particularly with species like *Amanita muscaria*, which can trigger autoimmune responses. To mitigate risks, consumers should source mushrooms from reputable suppliers and avoid foraging without expert guidance.
In conclusion, while scientific studies suggest that certain mushrooms may offer anti-inflammatory benefits for arthritis, their effects are highly species- and dose-dependent. Practical takeaways include prioritizing cooked over raw mushrooms, consulting healthcare providers before using mushroom supplements, and integrating them as part of a balanced diet rather than standalone remedies. Ongoing research will further clarify their role in arthritis management, bridging the gap between traditional knowledge and modern medicine.
Can You Eat Button Mushrooms Raw? A Complete Guide
You may want to see also

Potential Allergic Reactions and Joint Pain
Mushrooms, while celebrated for their nutritional benefits, can trigger allergic reactions in some individuals, manifesting as joint pain or exacerbating arthritis-like symptoms. These reactions are often linked to proteins in mushrooms that the immune system misidentifies as threats, releasing histamines and inflammatory compounds. Unlike typical food allergies that cause immediate symptoms, mushroom-related joint pain may emerge hours or days later, making the connection less obvious. For those with pre-existing arthritis, this delayed response can complicate symptom management, as the pain mimics a flare-up rather than an allergic reaction.
Identifying a mushroom allergy requires vigilance, particularly for older adults and individuals with autoimmune conditions, who are more susceptible. Symptoms may include swelling, stiffness, or aching in the joints, often accompanied by skin rashes, digestive discomfort, or respiratory issues. If joint pain occurs after consuming mushrooms—whether raw, cooked, or in supplements—a food diary can help track patterns. Consulting an allergist for skin prick tests or blood tests (like IgE antibody measurements) can confirm the allergy, though these tests are not always definitive for mushroom sensitivities.
For those at risk, moderation and preparation methods matter. Cooking mushrooms thoroughly can denature some allergenic proteins, potentially reducing reactivity compared to raw consumption. However, individuals with severe allergies should avoid mushrooms entirely, including hidden sources like mushroom-based broths or supplements. Reading labels carefully and inquiring about ingredients when dining out are essential precautions. For mild reactions, over-the-counter antihistamines (e.g., 25–50 mg of diphenhydramine) can alleviate symptoms, but persistent joint pain warrants medical evaluation to rule out other causes.
Comparatively, mushroom-induced joint pain differs from arthritis in its reversibility—symptoms typically subside within days of eliminating mushrooms from the diet. Arthritis, however, is chronic and progressive. Yet, for those with conditions like rheumatoid arthritis, mushroom allergies can act as a trigger, worsening inflammation. This interplay highlights the importance of personalized dietary management. While mushrooms are not a direct cause of arthritis, their allergenic potential underscores the need for awareness, especially in vulnerable populations.
Practically, individuals concerned about mushroom allergies should start with small portions to gauge tolerance and avoid varieties like shiitake or portobello, which are more commonly associated with reactions. Incorporating anti-inflammatory foods (e.g., turmeric, ginger) into the diet can also mitigate joint discomfort. For those diagnosed with a mushroom allergy, exploring alternative umami-rich foods like fermented soy products or seaweed can satisfy culinary cravings without risk. Ultimately, understanding the link between mushrooms and joint pain empowers informed dietary choices, balancing health benefits with potential risks.
Can Store-Bought Mushrooms Be Eaten Raw? Safety Tips Revealed
You may want to see also
Frequently asked questions
There is no scientific evidence to suggest that eating mushrooms directly causes arthritis. Mushrooms are generally considered a healthy food and are rich in nutrients like vitamins, minerals, and antioxidants.
Some people may have sensitivities or allergies to specific mushrooms, which could potentially trigger inflammation or joint discomfort. However, this is rare and not a direct cause of arthritis.
Mushroom supplements, such as reishi or chaga, are often used for their anti-inflammatory properties and may benefit some individuals with arthritis. However, consult a healthcare provider before using them, as individual reactions can vary.
Consuming wild mushrooms, especially if improperly identified or toxic, can cause severe health issues, but there is no established link between wild mushrooms and arthritis. Always ensure mushrooms are safe and edible before consumption.