Mushrooms have gained attention for their potential health benefits, including anti-inflammatory and immune-modulating properties, which have led to questions about their role in managing conditions like endometriosis. Endometriosis, a chronic inflammatory disorder characterized by the growth of endometrial-like tissue outside the uterus, often involves significant pain and discomfort. While research on mushrooms specifically for endometriosis is limited, certain varieties like shiitake, maitake, and reishi are known for their anti-inflammatory and antioxidant effects, which could theoretically help alleviate symptoms. Additionally, mushrooms contain compounds like beta-glucans that support immune function, potentially reducing the inflammatory response associated with endometriosis. However, more targeted studies are needed to confirm their efficacy and safety in this context, and individuals should consult healthcare providers before incorporating mushrooms as a complementary approach to their treatment plan.
| Characteristics | Values |
|---|---|
| Anti-inflammatory Properties | Mushrooms like shiitake, maitake, and reishi contain compounds (e.g., beta-glucans, ergothioneine) that may reduce inflammation, potentially alleviating endometriosis symptoms. |
| Antioxidant Activity | Rich in antioxidants, mushrooms can combat oxidative stress, which is linked to endometriosis progression. |
| Immune Modulation | Certain mushrooms (e.g., reishi, turkey tail) may regulate immune function, potentially reducing abnormal tissue growth in endometriosis. |
| Hormonal Balance | Some mushrooms (e.g., chaga) are believed to support hormonal balance, though scientific evidence is limited. |
| Gut Health Support | Mushrooms are prebiotic, promoting a healthy gut microbiome, which may indirectly benefit endometriosis management. |
| Scientific Evidence | Limited direct studies on mushrooms and endometriosis; most benefits are inferred from general health properties. |
| Safety Considerations | Generally safe, but some individuals may have allergies or sensitivities; consult a healthcare provider before use. |
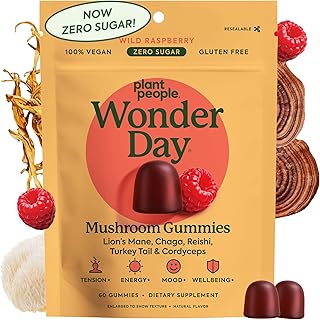
| Recommended Types | Shiitake, maitake, reishi, chaga, lion's mane, and oyster mushrooms are commonly suggested. |
| Preparation Methods | Consumed fresh, cooked, or as supplements (e.g., powders, capsules) for potential benefits. |
| Complementary Approach | Mushrooms should not replace medical treatment but may be used as a complementary dietary addition. |
Explore related products
What You'll Learn

Mushroom's Anti-Inflammatory Effects
Chronic inflammation is a hallmark of endometriosis, fueling pain, tissue damage, and disease progression. Mushrooms, particularly varieties like shiitake, maitake, and reishi, contain bioactive compounds with potent anti-inflammatory properties. Beta-glucans, polysaccharides found in mushroom cell walls, are key players in modulating the immune response and reducing inflammation. Studies suggest these compounds can inhibit pro-inflammatory cytokines like TNF-alpha and IL-6, which are often elevated in endometriosis patients.
Incorporating mushrooms into your diet isn’t just about tossing them into stir-fries. For maximum anti-inflammatory benefit, consider preparation methods that enhance bioavailability. Cooking mushrooms, especially at high heat, can break down cell walls, releasing more beta-glucans. Alternatively, mushroom extracts or supplements, such as reishi or chaga powders, offer concentrated doses. A daily intake of 2-3 grams of mushroom extract or 100-200 grams of fresh mushrooms may support anti-inflammatory efforts, though individual needs vary.
While mushrooms show promise, they aren’t a standalone cure for endometriosis. Their anti-inflammatory effects are best utilized as part of a holistic approach, including dietary changes, stress management, and medical treatment. For instance, pairing mushroom consumption with an anti-inflammatory diet rich in omega-3s, turmeric, and leafy greens can amplify their benefits. However, consult a healthcare provider before starting any supplement regimen, especially if you’re on medication or have underlying conditions.
Finally, not all mushrooms are created equal. Medicinal varieties like turkey tail and cordyceps have distinct anti-inflammatory profiles. Turkey tail, for example, is rich in polysaccharide-K (PSK), which has been studied for its immune-modulating effects. Cordyceps, on the other hand, may reduce inflammation by improving oxygen utilization and reducing oxidative stress. Experimenting with different types can help identify which mushrooms best support your body’s needs in managing endometriosis-related inflammation.
Mushrooms and Digestion: Boosting Bowel Movements Naturally Explained
You may want to see also

Immune System Regulation
Endometriosis, a condition where tissue similar to the uterine lining grows outside the uterus, is often linked to chronic inflammation and immune dysfunction. Mushrooms, particularly medicinal varieties like Reishi, Shiitake, and Maitake, contain bioactive compounds such as beta-glucans and polysaccharides that modulate immune responses. These compounds act as immunoregulators, helping to balance overactive or underactive immune systems, which may alleviate the inflammatory processes associated with endometriosis.
To harness mushrooms' immune-regulating benefits, consider incorporating them into your diet or supplement regimen. For instance, Reishi (Ganoderma lucidum) is known for its ability to downregulate pro-inflammatory cytokines, which are often elevated in endometriosis. A typical dosage is 1–1.5 grams of Reishi extract daily, preferably in divided doses. Shiitake mushrooms, rich in lentinan, can enhance immune function without overstimulation. Aim for 2–3 servings per week, either cooked or in supplement form (500 mg daily). Always consult a healthcare provider before starting any new supplement, especially if you have underlying conditions or are on medication.
A comparative analysis of mushroom types reveals that Turkey Tail (Trametes versicolor) is particularly effective for immune modulation due to its high polysaccharide-K (PSK) content. PSK has been studied for its ability to normalize immune responses, making it a promising candidate for endometriosis management. Unlike Reishi, which is more calming, Turkey Tail provides a balanced immune boost, suitable for those with fluctuating immune activity. A standard dose is 1–2 grams of Turkey Tail extract daily, often consumed as a tea or capsule.
Practical tips for integrating mushrooms into your routine include adding Shiitake to stir-fries, brewing Reishi tea in the evening for its calming effects, or taking mushroom supplements with meals to enhance absorption. For those sensitive to mushrooms, start with small amounts to assess tolerance. Combining mushroom therapy with anti-inflammatory foods like turmeric, ginger, and leafy greens can amplify their immune-regulating effects. Remember, consistency is key—immune modulation is a gradual process, and benefits may take 4–6 weeks to manifest.
In conclusion, mushrooms offer a natural, evidence-based approach to immune system regulation, which may indirectly support endometriosis management by addressing underlying inflammation. By selecting the right mushroom types, adhering to appropriate dosages, and integrating them thoughtfully into your lifestyle, you can potentially mitigate immune-related symptoms of endometriosis. However, mushrooms are not a standalone treatment, and their use should complement, not replace, medical advice and therapies prescribed by a healthcare professional.
Mushrooms' Eco-Friendly Impact: How Fungi Benefit Our Environment
You may want to see also

Hormonal Balance Support
Endometriosis, a condition where tissue similar to the uterine lining grows outside the uterus, is often exacerbated by hormonal imbalances, particularly elevated estrogen levels. Mushrooms, particularly varieties like reishi, lion's mane, and chaga, have been studied for their potential to modulate hormone levels naturally. These fungi contain compounds such as beta-glucans and triterpenes, which may influence the endocrine system by supporting liver function—a key organ in metabolizing hormones. For instance, reishi mushrooms are known to promote estrogen detoxification, potentially reducing the estrogen dominance commonly seen in endometriosis. While research is still emerging, incorporating these mushrooms into a balanced diet could offer a complementary approach to managing hormonal symptoms.
To harness the hormonal benefits of mushrooms, consider integrating them into your daily routine in specific ways. Reishi, often consumed as a tea or tincture, can be taken in doses of 1–1.5 grams per day. Lion's mane, available in capsule or powder form, is typically dosed at 500–1000 mg daily. Chaga, rich in antioxidants, can be brewed as a tea or taken as a supplement, with recommended doses ranging from 1–2 grams daily. For best results, consistency is key—incorporate these mushrooms into your diet over several weeks to observe potential hormonal balancing effects. Always consult a healthcare provider before starting any new supplement, especially if you’re on hormone-related medications.
A comparative analysis of mushroom varieties reveals their unique contributions to hormonal balance. Reishi stands out for its adaptogenic properties, helping the body regulate stress hormones like cortisol, which indirectly impacts estrogen levels. Lion's mane, on the other hand, supports the nervous system, reducing stress-induced hormonal fluctuations. Chaga’s high antioxidant content combats oxidative stress, a factor linked to hormonal imbalances. While no single mushroom is a cure-all, combining these varieties may provide a synergistic effect, addressing multiple facets of hormonal health. For example, pairing reishi with lion's mane could offer both stress reduction and estrogen modulation.
Practical tips for incorporating mushrooms into an endometriosis management plan include experimenting with culinary uses—adding lion's mane to stir-fries or blending chaga powder into smoothies. For those who prefer convenience, supplements are a viable option, but quality matters. Opt for organic, third-party tested products to ensure purity and potency. Additionally, tracking symptoms over time can help determine the effectiveness of mushroom-based interventions. Keep a journal to note changes in menstrual pain, mood, or energy levels, as these can be indicators of hormonal shifts. While mushrooms alone may not resolve endometriosis, they can be a valuable tool in a holistic approach to hormonal balance.
Finding Your Ideal Magic Mushroom Dosage for a Positive Trip Experience
You may want to see also
Explore related products

Antioxidant Properties
Mushrooms, particularly varieties like shiitake, maitake, and reishi, are rich in antioxidants such as ergothioneine, selenium, and polyphenols. These compounds neutralize free radicals, which are implicated in the inflammation and oxidative stress associated with endometriosis. Studies suggest that oxidative stress exacerbates the condition by damaging tissues and promoting abnormal cell growth. Incorporating antioxidant-rich mushrooms into your diet may help mitigate these effects, though their role is supportive rather than curative.
To harness their antioxidant benefits, consider integrating mushrooms into your daily meals. For instance, sauté shiitake mushrooms with garlic and olive oil as a side dish, or add powdered reishi to smoothies for a concentrated dose. Aim for 100–200 grams of fresh mushrooms daily, or 1–2 teaspoons of mushroom powder, depending on the variety. Pairing mushrooms with vitamin C-rich foods like bell peppers or citrus enhances antioxidant absorption, maximizing their impact on reducing inflammation linked to endometriosis.
While mushrooms offer antioxidant support, they should complement, not replace, medical treatments for endometriosis. Consult a healthcare provider before making significant dietary changes, especially if you have allergies or are taking medications. Pregnant or breastfeeding individuals should exercise caution with certain mushroom types, such as reishi, due to limited safety data. Always source mushrooms from reputable suppliers to avoid contamination or misidentification of wild varieties.
Comparatively, mushrooms stand out among antioxidant-rich foods due to their unique compounds like ergothioneine, which is less abundant in fruits and vegetables. Unlike supplements, whole mushrooms provide synergistic benefits from fiber, vitamins, and minerals. However, their antioxidant capacity varies by species and preparation method—cooking can enhance bioavailability but may reduce heat-sensitive compounds. For optimal results, diversify your intake by combining fresh, cooked, and powdered forms in your diet.
Incorporating antioxidant-rich mushrooms into your routine is a practical step toward managing endometriosis symptoms. Start small, such as adding a handful of maitake to stir-fries or brewing reishi tea, and monitor how your body responds. While not a standalone solution, their anti-inflammatory and tissue-protective properties make them a valuable addition to a holistic approach. Pair dietary changes with stress management and regular exercise for a comprehensive strategy to support your body’s natural defenses.
Eggplant and Mushroom Pizza: A Delicious and Unique Topping Combo?
You may want to see also

Potential Pain Relief Benefits
Mushrooms, particularly varieties like Reishi, Chaga, and Lion's Mane, contain bioactive compounds that may alleviate inflammation and modulate pain pathways. For individuals with endometriosis, where chronic pelvic pain is a hallmark symptom, these properties could offer a complementary approach to managing discomfort. Beta-glucans, found abundantly in medicinal mushrooms, have been shown to reduce pro-inflammatory cytokines, potentially easing the systemic inflammation associated with endometriosis-related pain.
To harness these benefits, consider incorporating mushroom extracts or powders into your daily routine. A typical dosage is 1–2 grams of mushroom extract per day, either in capsule form or mixed into beverages like tea or smoothies. For example, Reishi mushroom, known for its analgesic effects, can be consumed as a tincture (30–60 drops daily) or in powdered form (1 teaspoon in warm water). Always start with a lower dose to assess tolerance, especially if you have sensitivities or are taking other medications.
While mushrooms are generally safe, their efficacy in pain relief for endometriosis is not yet fully supported by large-scale clinical trials. However, anecdotal evidence and preliminary studies suggest they may reduce pain intensity and frequency. For instance, Lion's Mane mushroom has been linked to nerve regeneration, which could indirectly benefit those experiencing neuropathic pain from endometriosis. Pairing mushroom supplementation with anti-inflammatory foods like turmeric and omega-3-rich fish may enhance their pain-relieving effects.
Practical tips for integration include choosing organic, lab-tested mushroom products to ensure purity and potency. Avoid raw mushrooms, as cooking or extracting enhances bioavailability. If you’re pregnant, breastfeeding, or have an autoimmune condition, consult a healthcare provider before starting any mushroom regimen. While not a standalone treatment, mushrooms could serve as a natural adjunct to conventional pain management strategies for endometriosis.
Shiitake Mushrooms in Dumplings: A Flavorful Addition or Overrated?
You may want to see also
Frequently asked questions
Some mushrooms, like shiitake and reishi, contain anti-inflammatory and immune-boosting properties that may help manage endometriosis symptoms, but scientific evidence is limited, and they should not replace medical treatment.
Certain mushrooms, such as lion’s mane and turkey tail, have anti-inflammatory compounds that may help reduce inflammation, but their direct impact on endometriosis-related inflammation is not yet fully understood.
Medicinal mushrooms like chaga, cordyceps, and maitake are often suggested for their potential to support hormonal balance and reduce inflammation, but consult a healthcare provider before incorporating them into your diet.