The death cap mushroom (*Amanita phalloides*) is one of the most poisonous fungi in the world, responsible for the majority of fatal mushroom poisonings globally. Its toxins, primarily amatoxins, cause severe liver and kidney damage, often leading to organ failure if left untreated. If ingested, immediate medical attention is crucial, as symptoms may not appear for 6–24 hours, creating a false sense of security. Treatment typically involves gastric decontamination, supportive care, and, in severe cases, liver transplantation. Additionally, medications like silibinin (milk thistle extract) and N-acetylcysteine may be used to mitigate toxin effects. Early identification and intervention are key to survival, as delays can significantly worsen outcomes.
| Characteristics | Values |
|---|---|
| Toxicity | Extremely toxic due to amatoxins (alpha-amanitin, beta-amanitin) |
| Symptoms | Delayed onset (6-24 hours): vomiting, diarrhea, abdominal pain, dehydration, liver failure, kidney failure, coma |
| Fatality Rate | 10-50% without treatment; higher without prompt medical intervention |
| Treatment Availability | Yes, but requires immediate medical attention |
| First Aid | Call emergency services, do not induce vomiting, avoid home remedies |
| Medical Treatments | - Activated charcoal (if ingested recently) - Gastric lavage - Intravenous fluids - Silibinin (milk thistle extract) - Liver transplant in severe cases - Supportive care (dialysis, medications) |
| Time Sensitivity | Critical; treatment must begin within hours of ingestion |
| Prognosis | Depends on time to treatment, amount consumed, and individual health |
| Prevention | Avoid consuming wild mushrooms unless identified by an expert |
| Geographic Distribution | Found in Europe, North America, Australia, and other temperate regions |
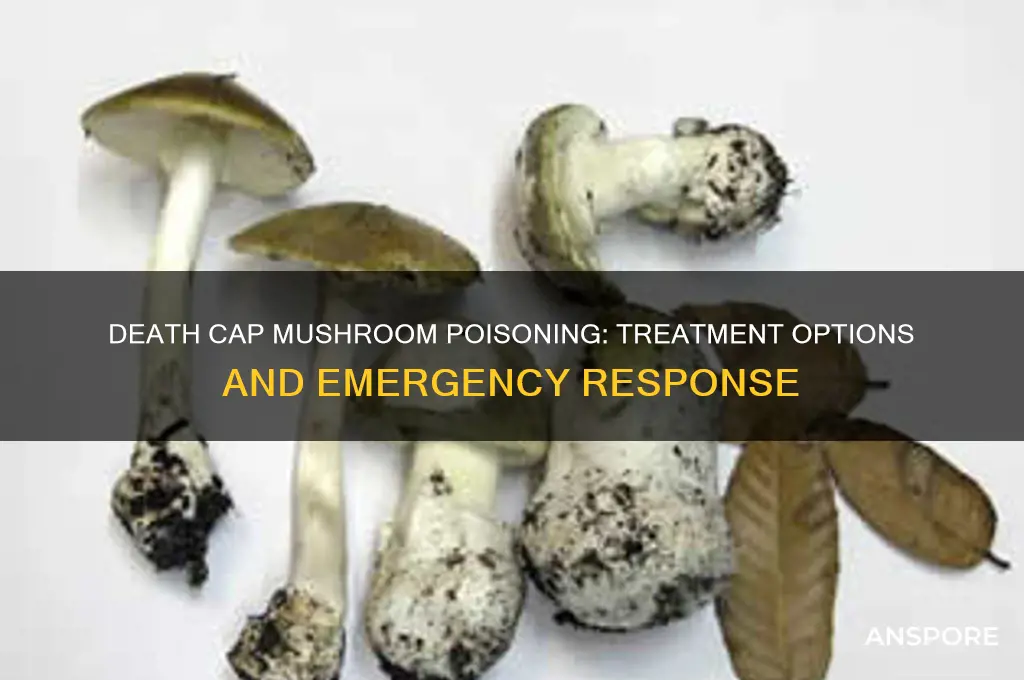
| Identification | Death cap (Amanita phalloides) is greenish-yellow with a white stalk |
| Misidentification Risk | High; often mistaken for edible mushrooms like straw mushrooms or puffballs |
Explore related products
What You'll Learn
- Immediate Actions: Induce vomiting, seek emergency care, and provide activated charcoal to prevent absorption
- Medical Treatments: Intravenous fluids, liver support, and antidotes like silibinin to manage toxicity
- Symptom Management: Address nausea, diarrhea, and dehydration with medications and hydration therapy
- Liver Transplant: Consideration for severe cases with irreversible liver damage due to amatoxins
- Prognosis Factors: Survival depends on early treatment, toxin levels, and overall health condition

Immediate Actions: Induce vomiting, seek emergency care, and provide activated charcoal to prevent absorption
If someone has ingested a death cap mushroom (*Amanita phalloides*), immediate and aggressive action is crucial to increase the chances of survival. The first step is to induce vomiting as quickly as possible. This can help expel the toxin from the stomach before it is fully absorbed into the bloodstream. To induce vomiting, you can use a finger or a spoon to stimulate the back of the throat, but it’s essential to act within the first hour of ingestion for maximum effectiveness. However, if the person is unconscious, vomiting should not be induced to avoid the risk of choking. Instead, focus on seeking emergency medical care immediately.
The next critical step is to seek emergency medical care without delay. Call emergency services or rush the individual to the nearest hospital. Time is of the essence, as death cap poisoning can lead to severe liver and kidney damage within 24 to 48 hours. Inform the medical team about the suspected ingestion of a death cap mushroom, as this will help them initiate targeted treatment protocols. The hospital may administer medications like silibinin (an active compound in milk thistle) to protect the liver, as well as intravenous fluids and electrolytes to stabilize the patient.
While waiting for emergency care, activated charcoal can be administered to help prevent further absorption of the toxins. Activated charcoal works by binding to the toxins in the gastrointestinal tract, reducing their absorption into the bloodstream. It is most effective when given within the first hour of ingestion but can still be beneficial even if given later. However, activated charcoal should only be used under the guidance of a healthcare professional, as improper administration can lead to complications, especially in severe cases.
It’s important to note that do not wait for symptoms to appear before taking action. Death cap poisoning often has a latency period, with symptoms like nausea, vomiting, and diarrhea appearing 6 to 24 hours after ingestion, followed by a false "recovery" period before severe liver and kidney failure set in. Early intervention is key to preventing irreversible damage. Avoid giving any home remedies or attempting to neutralize the toxin without professional advice, as this can delay proper treatment.
In summary, the immediate actions for death cap mushroom ingestion are clear: induce vomiting if safe, seek emergency care immediately, and provide activated charcoal under professional guidance to prevent toxin absorption. These steps, combined with prompt medical intervention, can significantly improve the prognosis in a life-threatening situation like death cap poisoning.
Do Capuchin Monkeys Eat Mushrooms? Exploring Their Dietary Habits
You may want to see also

Medical Treatments: Intravenous fluids, liver support, and antidotes like silibinin to manage toxicity
When someone ingests a death cap mushroom (*Amanita phalloides*), immediate and aggressive medical treatment is crucial to counteract its potent toxins, primarily amatoxins, which cause severe liver damage. Intravenous (IV) fluids are the cornerstone of initial treatment. These fluids, typically administered in an emergency setting, help stabilize the patient by maintaining hydration, supporting blood pressure, and promoting urine production. Enhanced diuresis (urine output) is particularly important as it aids in flushing out the toxins from the body, reducing their absorption and minimizing further liver damage. IV fluids also help counteract the dehydration caused by symptoms like vomiting and diarrhea, which are common after ingestion.
In addition to IV fluids, liver support is critical in managing death cap mushroom poisoning. Amatoxins directly target liver cells, leading to acute liver failure. Continuous monitoring of liver function tests, such as alanine transaminase (ALT) and aspartate transaminase (AST), is essential to assess the extent of liver damage. In severe cases, extracorporeal liver support systems, such as molecular adsorbent recirculating system (MARS) therapy, may be employed. These systems help remove toxins from the blood, providing temporary support to the failing liver and buying time for the organ to recover or for a liver transplant to be considered if necessary.
Another key component of treatment is the use of antidotes, with silibinin being the most prominent. Silibinin, derived from milk thistle, acts by inhibiting the uptake of amatoxins into liver cells and promoting their excretion. It is most effective when administered early, ideally within 24–48 hours of ingestion. The standard protocol involves high-dose intravenous silibinin, often given over several days. Studies have shown that silibinin significantly improves survival rates in patients with death cap mushroom poisoning, especially when combined with aggressive supportive care.
In some cases, activated charcoal may be administered shortly after ingestion to bind the toxins in the gastrointestinal tract and prevent further absorption. However, its effectiveness diminishes rapidly after the first few hours, making it a secondary measure compared to IV fluids, liver support, and antidotes. Additionally, N-acetylcysteine (NAC) may be used to protect liver cells from oxidative damage, though its role is supplementary to silibinin and other primary treatments.
Finally, in cases of severe liver failure unresponsive to medical management, liver transplantation may be the last resort. This is considered when all other treatments fail and the patient’s life is at imminent risk. However, transplantation is a complex and resource-intensive procedure, and its success depends on timely availability of a donor organ and the patient’s overall condition. Early and comprehensive medical intervention, including IV fluids, liver support, and antidotes like silibinin, remains the best approach to managing death cap mushroom toxicity and improving survival outcomes.
Exploring Fly Agaric Mushrooms: Safe Consumption Guide and Tips
You may want to see also

Symptom Management: Address nausea, diarrhea, and dehydration with medications and hydration therapy
When treating poisoning from a death cap mushroom (*Amanita phalloides*), managing gastrointestinal symptoms like nausea, vomiting, and diarrhea is critical to prevent complications such as dehydration and electrolyte imbalance. Antiemetic medications are the first line of defense against nausea and vomiting. Drugs like ondansetron or metoclopramide can be administered to control these symptoms, allowing the patient to tolerate oral fluids or medications better. These medications work by blocking signals in the brain that trigger nausea, providing rapid relief and improving the patient’s comfort.
Diarrhea management is equally important, as prolonged or severe diarrhea can lead to significant fluid and electrolyte loss. Antidiarrheal agents such as loperamide may be used cautiously, but their use must be balanced against the need to eliminate toxins from the gastrointestinal tract. In severe cases, intravenous (IV) fluids are often necessary to replace lost fluids and electrolytes. Oral rehydration solutions (ORS) can be used if the patient is able to drink, but IV hydration therapy is typically preferred due to its reliability and speed in correcting dehydration.
Hydration therapy is a cornerstone of symptom management in death cap mushroom poisoning. IV fluids, such as lactated Ringer’s solution or normal saline, are administered to restore fluid balance and maintain blood pressure. The type and rate of fluid administration are tailored to the patient’s condition, with close monitoring of electrolyte levels, particularly potassium and magnesium, which can become depleted due to vomiting and diarrhea. Continuous assessment of hydration status, including monitoring urine output and vital signs, ensures that the therapy is effective.
In addition to fluids, electrolyte replacement is essential to prevent complications like cardiac arrhythmias or muscle weakness. Potassium, magnesium, and calcium supplements may be given intravenously or orally, depending on the severity of depletion. This step is particularly crucial in patients with prolonged or severe symptoms, as electrolyte imbalances can exacerbate the toxicity of the mushroom’s toxins. Regular blood tests may be conducted to guide replacement therapy and ensure levels remain within safe ranges.
Finally, supportive care plays a vital role in symptom management. Patients should be encouraged to rest and avoid strenuous activity, as dehydration and electrolyte imbalances can cause fatigue and weakness. Monitoring for signs of worsening dehydration, such as decreased urine output, dry mucous membranes, or dizziness, is essential. In severe cases, hospitalization in an intensive care unit may be required to provide continuous monitoring and aggressive hydration therapy. Early and proactive management of these symptoms can significantly improve outcomes in death cap mushroom poisoning.
Mushrooms in the Bible: Forbidden Food or Culinary Freedom?
You may want to see also
Explore related products

Liver Transplant: Consideration for severe cases with irreversible liver damage due to amatoxins
In cases of severe poisoning from consuming the death cap mushroom (*Amanita phalloides*), which contains potent amatoxins, liver transplant may be considered as a life-saving intervention. Amatoxins cause irreversible liver damage by inhibiting RNA polymerase II, leading to hepatocyte necrosis and acute liver failure. Despite aggressive supportive care, such as activated charcoal, silibinin, and N-acetylcysteine, some patients progress to fulminant hepatic failure, where liver transplant becomes the only viable option. The decision to proceed with a transplant is critical and must be made swiftly, as delays can result in multiorgan failure or death.
The indication for liver transplant in amatoxin poisoning is based on the severity of liver damage and the patient's clinical deterioration. Key criteria include rapidly rising liver enzymes (AST, ALT), coagulopathy (prothrombin time/INR), and signs of hepatic encephalopathy. Patients with a King’s College Criteria-positive status or MELD (Model for End-Stage Liver Disease) score indicative of poor prognosis are prioritized for transplant evaluation. It is essential to rule out other contraindications, such as irreversible brain damage or uncontrolled infection, before proceeding.
The timing of liver transplant is crucial. Amatoxin-induced liver failure progresses rapidly, often within 48–72 hours of ingestion, necessitating immediate access to a transplant center. The procedure involves removing the damaged liver and replacing it with a healthy donor organ. Post-transplant, patients require lifelong immunosuppression to prevent organ rejection, along with close monitoring for complications such as infection or graft dysfunction. The success rate of liver transplant in amatoxin poisoning is relatively high, with survival rates comparable to transplants for other causes of acute liver failure.
However, liver transplant is not without risks. Surgical complications, rejection episodes, and long-term immunosuppression-related issues (e.g., infections, malignancies) are significant concerns. Additionally, the availability of donor organs remains a limiting factor, emphasizing the importance of early identification and management of amatoxin poisoning. In resource-limited settings or when transplant is not feasible, extracorporeal liver support systems may serve as a bridge to recovery or transplant, though their efficacy is still under investigation.
In conclusion, liver transplant is a critical consideration for severe cases of amatoxin poisoning with irreversible liver damage. It offers a second chance at life for patients who would otherwise succumb to acute liver failure. However, the decision requires a multidisciplinary approach, involving toxicologists, hepatologists, and transplant surgeons, to ensure timely and appropriate intervention. Public awareness about the dangers of death cap mushrooms and the importance of immediate medical attention after ingestion remains paramount in preventing such severe outcomes.
Deadly Mushroom Danger: How Quickly Do Dogs React to Poisoning?
You may want to see also

Prognosis Factors: Survival depends on early treatment, toxin levels, and overall health condition
The prognosis for someone who has ingested a death cap mushroom (*Amanita phalloides*) depends critically on early treatment, toxin levels absorbed by the body, and the individual’s overall health condition. Immediate medical intervention is paramount, as the toxins in the death cap, primarily alpha-amanitin, cause severe liver and kidney damage, often leading to organ failure if untreated. Recognizing symptoms such as nausea, vomiting, diarrhea, and abdominal pain within 6–24 hours of ingestion is crucial. Delay in treatment significantly worsens the prognosis, as the toxins continue to accumulate and cause irreversible damage.
Toxin levels play a pivotal role in determining survival outcomes. The amount of mushroom consumed directly correlates with the severity of poisoning. Even a small portion of a death cap contains enough alpha-amanitin to cause fatal liver damage. However, the body’s absorption rate and the time it takes for toxins to reach critical organs also influence the prognosis. Gastric decontamination, including induced vomiting or activated charcoal administration, can reduce toxin absorption if performed within hours of ingestion. Blood tests to measure toxin levels and liver function are essential for assessing the severity of the poisoning and guiding treatment.
The individual’s overall health condition is another critical factor in survival. Patients with pre-existing liver or kidney disease, weakened immune systems, or poor overall health are at higher risk of severe complications or death. Conversely, young, healthy individuals with robust organ function may have a better chance of recovery, especially with aggressive treatment. Chronic health conditions can exacerbate the effects of the toxins, making it harder for the body to recover even with medical intervention.
Early treatment is the most significant determinant of survival. Immediate medical care, including hospitalization, supportive therapies, and specific treatments like silibinin (a milk thistle derivative) or liver transplantation in severe cases, can drastically improve outcomes. Silibinin helps protect liver cells from toxin damage, but its effectiveness depends on timely administration. In cases of advanced liver failure, a liver transplant may be the only life-saving option. However, this is a last resort and depends on the availability of a donor and the patient’s stability.
In summary, survival after ingesting a death cap mushroom hinges on a combination of early treatment, toxin levels, and the individual’s overall health condition. Prompt recognition of symptoms, immediate medical intervention, and aggressive management of toxin effects are essential for a favorable prognosis. Public awareness of the dangers of death cap mushrooms and the importance of seeking urgent medical care cannot be overstated, as it can mean the difference between life and death.
Avoid the Mushroom Vavr: A Guide to Safe Foraging Practices
You may want to see also
Frequently asked questions
Yes, immediate medical treatment is crucial. Seek emergency care right away, as death cap poisoning can be fatal without prompt intervention.
Call poison control or go to the nearest emergency room immediately. Do not wait for symptoms to appear, as early treatment improves survival chances.
Treatment includes gastric decontamination (e.g., activated charcoal), supportive care, and medications like silibinin (milk thistle extract) to protect the liver from damage.
Early treatment significantly improves survival rates, but the outcome depends on the severity of poisoning and how quickly treatment is initiated.
Survivors may experience long-term liver damage or require a liver transplant, depending on the extent of organ injury caused by the toxins.











































