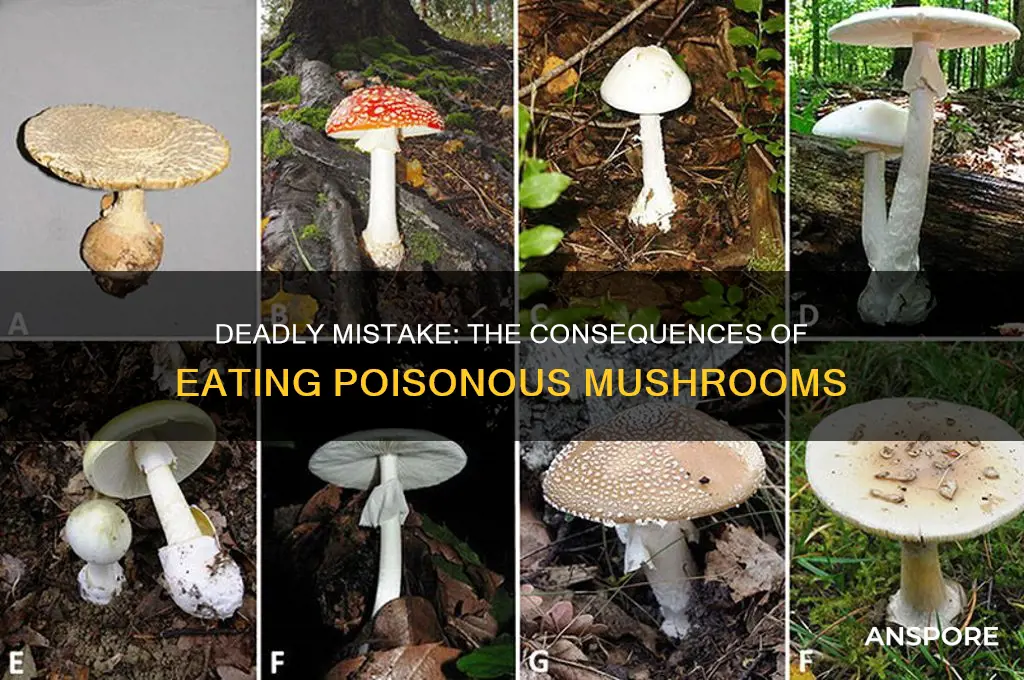
Eating a poisonous mushroom can have severe and potentially life-threatening consequences, as many species contain toxins that can cause rapid and debilitating symptoms. Depending on the type of mushroom ingested, effects can range from mild gastrointestinal distress, such as nausea, vomiting, and diarrhea, to more severe conditions like liver or kidney failure, seizures, and even death. Some toxins, like those found in the Death Cap (*Amanita phalloides*) or Destroying Angel (*Amanita bisporigera*), can be fatal if not treated promptly. Symptoms may appear within hours or be delayed, making identification and medical intervention critical. Misidentification of mushrooms is a common cause of poisoning, underscoring the importance of expert knowledge or consultation before consuming wild fungi. Immediate medical attention is essential if poisoning is suspected, as early treatment can significantly improve outcomes.
| Characteristics | Values |
|---|---|
| Gastrointestinal Symptoms | Nausea, vomiting, diarrhea, abdominal pain, cramps, and dehydration. |
| Neurological Effects | Hallucinations, confusion, seizures, dizziness, and muscle weakness. |
| Liver Damage | Jaundice, liver failure, and elevated liver enzymes (e.g., Amanita species). |
| Kidney Damage | Kidney failure or dysfunction in severe cases. |
| Cardiovascular Effects | Irregular heartbeat, low blood pressure, and cardiac arrest. |
| Respiratory Distress | Difficulty breathing or respiratory failure in extreme cases. |
| Psychological Symptoms | Anxiety, agitation, delirium, or coma. |
| Onset of Symptoms | Can range from 20 minutes to 24 hours depending on the mushroom species. |
| Long-Term Effects | Permanent organ damage, chronic health issues, or death. |
| Treatment | Gastric lavage, activated charcoal, supportive care, and antidotes (if available). |
| Fatality Risk | Varies by species; some (e.g., Death Cap) have high mortality rates. |
| Prevention | Avoid consuming wild mushrooms unless identified by an expert. |
Explore related products
What You'll Learn
- Immediate Symptoms: Nausea, vomiting, diarrhea, abdominal pain, and cramps appear within hours of ingestion
- Organ Damage: Liver, kidneys, or heart may fail due to toxic compounds in certain mushrooms
- Neurological Effects: Hallucinations, seizures, confusion, or coma can occur from psychoactive toxins
- Long-Term Consequences: Chronic health issues like liver cirrhosis or kidney damage may develop
- Fatal Outcomes: Some poisonous mushrooms, like the Death Cap, can be lethal if untreated

Immediate Symptoms: Nausea, vomiting, diarrhea, abdominal pain, and cramps appear within hours of ingestion
The body’s reaction to a poisonous mushroom is swift and unforgiving. Within hours of ingestion, the gastrointestinal system rebels, signaling distress through nausea, vomiting, diarrhea, abdominal pain, and cramps. These symptoms are the body’s desperate attempt to expel the toxin before it can cause further harm. For instance, the *Amanita phalloides* (Death Cap) contains amatoxins that disrupt cellular function, leading to these immediate symptoms as the liver and kidneys begin to fail. Recognizing this rapid onset is critical, as it distinguishes toxic mushrooms from those causing delayed reactions, such as hallucinogenic species.
Consider this scenario: a hiker forages a mushroom resembling a harmless chanterelle but unknowingly consumes a *Galerina marginata*. Within 6–24 hours, they experience severe nausea and vomiting. The timing is key—immediate symptoms like these often correlate with mushrooms containing gastrointestinal irritants, such as muscarine or coprine. Unlike delayed reactions, which might involve organ failure or neurological effects, these symptoms are the body’s first line of defense. However, they are not merely inconvenient; prolonged vomiting and diarrhea can lead to dehydration, especially in children or the elderly, requiring immediate rehydration with oral solutions or, in severe cases, intravenous fluids.
From a practical standpoint, anyone experiencing these symptoms after mushroom ingestion should act swiftly. First, call a poison control center or seek emergency medical care. Bring a sample of the mushroom for identification, as this aids in treatment. Do not induce vomiting unless advised by a professional, as some toxins can cause further damage when regurgitated. Keep the person hydrated with small sips of water if they can tolerate it, but avoid solid food until symptoms subside. Time is of the essence—delaying treatment can allow toxins to progress to more severe stages, such as liver or kidney damage.
Comparatively, these immediate symptoms differ from those caused by psychoactive mushrooms, which often induce hallucinations or paranoia within 20–90 minutes. The distinction lies in the toxin type and its mechanism of action. Gastrointestinal symptoms are typically linked to mushrooms containing protoplasmic poisons, which directly damage cells, whereas psychoactive effects stem from compounds like psilocybin that alter brain chemistry. Understanding this difference can guide initial response: one requires urgent medical intervention, while the other may necessitate monitoring for psychological distress.
In conclusion, the rapid onset of nausea, vomiting, diarrhea, abdominal pain, and cramps is a red flag for mushroom poisoning. These symptoms are not merely discomforts but urgent warnings that demand immediate action. By recognizing the timing, severity, and associated risks, individuals can mitigate harm and seek appropriate care. Always remember: when in doubt, leave mushrooms to the experts, as the consequences of misidentification can be life-threatening.
Mushroom Supplements: Can They Boost Your Dog's Lifespan?
You may want to see also

Organ Damage: Liver, kidneys, or heart may fail due to toxic compounds in certain mushrooms
Toxic compounds in certain mushrooms can wreak havoc on vital organs, leading to potentially fatal consequences. Among the most vulnerable are the liver, kidneys, and heart, which may fail due to the accumulation of these poisons. For instance, the death cap mushroom (*Amanita phalloides*) contains amatoxins that specifically target liver cells, causing severe damage within hours of ingestion. Even a small bite—as little as 30 grams—can be lethal to an adult, while children are at risk from even smaller amounts. Recognizing symptoms like nausea, vomiting, and abdominal pain within 6–24 hours is crucial, as delayed treatment significantly increases the risk of liver failure.
The kidneys, too, are at risk from mushroom toxins, particularly those found in species like the destroyng angel (*Amanita bisporigera*). These toxins cause acute kidney injury by disrupting filtration and excretion processes, leading to a dangerous buildup of waste products in the body. Unlike liver damage, kidney failure from mushroom poisoning often manifests later, typically 3–5 days after ingestion, with symptoms such as reduced urine output, swelling, and fatigue. Dialysis may be required in severe cases, but prevention remains the best strategy—always verify mushroom identity before consumption.
Heart failure, though less common, can occur due to cardiotoxic compounds in certain mushrooms, such as the toxins found in the ivory funnel (*Clitocybe dealbata*). These substances interfere with the heart’s electrical system, causing irregular rhythms (arrhythmias) that can be life-threatening. Symptoms like dizziness, palpitations, and chest pain may appear within 1–3 hours of ingestion. Immediate medical attention is essential, as antiarrhythmic medications or even pacemakers may be needed to stabilize the heart.
To minimize the risk of organ damage, follow these practical steps: avoid consuming wild mushrooms unless identified by an expert, cook all mushrooms thoroughly (though this does not neutralize all toxins), and educate children about the dangers of eating unknown fungi. If poisoning is suspected, contact a poison control center or seek emergency care immediately. Carrying a small sample of the mushroom for identification can aid diagnosis. Remember, time is critical—rapid treatment can mean the difference between recovery and organ failure.
Mushrooms and Sinus Drainage: Uncovering the Surprising Connection
You may want to see also

Neurological Effects: Hallucinations, seizures, confusion, or coma can occur from psychoactive toxins
Psychoactive toxins in certain mushrooms can unleash a cascade of neurological effects, transforming a foraging mistake into a medical emergency. These toxins, such as psilocybin, muscimol, and ibotenic acid, target the brain's neurotransmitter systems, particularly those involving serotonin and acetylcholine. Even a small bite of a mushroom like the Amanita muscaria or Psilocybe species can lead to profound alterations in perception, cognition, and consciousness. The onset of symptoms can be rapid, often within 30 minutes to 2 hours after ingestion, making prompt identification and treatment critical.
Hallucinations are among the most striking effects of psychoactive mushroom toxins. Unlike the controlled settings of therapeutic psilocybin use, accidental ingestion often results in unpredictable and distressing visual, auditory, or tactile distortions. These experiences can be terrifying, especially for individuals unaware of the cause or unprepared for the intensity. For instance, a child who consumes a fragment of a Psilocybe mushroom might describe seeing "moving colors" or "talking animals," while an adult could experience more complex and disorienting visions. The severity of hallucinations often correlates with the dose ingested, but individual sensitivity and mushroom potency can skew this relationship.
Seizures represent a more severe neurological consequence, triggered by toxins that disrupt the brain's electrical activity. Ibotenic acid, found in Amanita muscaria, can overstimulate glutamate receptors, leading to convulsions that may progress to status epilepticus—a life-threatening condition requiring immediate medical intervention. Seizures are particularly dangerous in children and the elderly, whose brains are more vulnerable to such disturbances. Even in healthy adults, seizures can cause physical injury, aspiration pneumonia, or long-term neurological damage if not managed promptly.
Confusion and coma are late-stage effects that signal severe poisoning. Confusion often begins as mild disorientation but can escalate to agitation, incoherence, or unresponsiveness. Coma, typically induced by toxins like amatoxins (though not strictly psychoactive), can also result from the cumulative stress of seizures, dehydration, or metabolic imbalances caused by prolonged neurological disruption. In such cases, supportive care in an intensive care unit becomes essential, often involving ventilation, fluid management, and anticonvulsant medications.
To mitigate these risks, prevention is paramount. Educate yourself and others about the appearance of common toxic mushrooms, such as the Amanita species, and avoid consuming wild mushrooms unless identified by a mycologist. If ingestion occurs, seek medical attention immediately, even if symptoms seem mild. Bring a sample of the mushroom for identification, as this can guide treatment. Remember, the neurological effects of psychoactive toxins are not just a "bad trip"—they are a medical crisis requiring swift and informed action.
Delicious Pairing: Cooking Chicken and Mushrooms Together – Tips & Recipes
You may want to see also
Explore related products

Long-Term Consequences: Chronic health issues like liver cirrhosis or kidney damage may develop
The insidious nature of poisonous mushrooms lies not only in their immediate toxicity but also in their potential to wreak havoc on vital organs over time. While acute symptoms like nausea, vomiting, and diarrhea often dominate discussions about mushroom poisoning, the long-term consequences can be far more devastating. Chronic health issues such as liver cirrhosis and kidney damage are silent threats that may emerge months or even years after ingestion, often catching victims off guard. These conditions develop as the toxins accumulate and gradually erode organ function, making early detection and intervention critical.
Consider the case of amatoxin-containing mushrooms, such as the Death Cap (*Amanita phalloides*). Even a small bite—as little as 50 grams for an adult—can lead to severe liver damage if left untreated. Amatoxins are cyclic octapeptides that selectively target hepatocytes, causing irreversible harm. Over time, repeated exposure or a single significant ingestion can progress to liver cirrhosis, a condition characterized by scarring and loss of liver function. This is not merely a theoretical risk; case studies have documented patients developing cirrhosis years after a single poisoning incident, often requiring liver transplantation for survival.
Kidney damage, though less commonly discussed, is another grave long-term consequence of mushroom poisoning. Certain toxins, like orellanine found in the Fool’s Webcap (*Cortinarius orellanus*), specifically target renal tissue. Orellanine causes acute tubular necrosis, a condition where the kidney’s filtering units are destroyed. While some individuals may recover partial function, others face chronic kidney disease or end-stage renal failure, necessitating dialysis or transplantation. The onset of symptoms is often delayed, with kidney damage becoming apparent 3–14 days after ingestion, making it easy to overlook the connection to mushroom consumption.
Preventing these long-term consequences requires vigilance and swift action. If poisoning is suspected, immediate medical attention is non-negotiable. Activated charcoal may be administered to reduce toxin absorption, and in severe cases, liver or kidney support therapies are initiated. For high-risk toxins like amatoxins, silibinin (a milk thistle derivative) has shown promise in mitigating liver damage when given within 48 hours of ingestion. However, the most effective strategy remains avoidance—never consume wild mushrooms unless positively identified by an expert. Even experienced foragers make mistakes, underscoring the importance of caution.
In conclusion, the long-term consequences of eating poisonous mushrooms are no less dangerous than the immediate symptoms. Liver cirrhosis and kidney damage are not inevitable outcomes but are entirely preventable with awareness and prompt treatment. Understanding the risks, recognizing the signs, and acting decisively can mean the difference between recovery and lifelong debilitation. When it comes to mushrooms, the old adage holds true: better safe than sorry.
Freezing Mushroom Stroganoff: Tips for Storing and Reheating Perfectly
You may want to see also

Fatal Outcomes: Some poisonous mushrooms, like the Death Cap, can be lethal if untreated
The Death Cap mushroom, scientifically known as *Amanita phalloides*, is a silent assassin lurking in forests and gardens. Its innocuous appearance—a pale green or yellowish cap with a slender stem—believes it to be edible, but a single bite can lead to irreversible damage. Ingesting just 50 grams of this mushroom, roughly half a cap, contains enough toxins to kill an adult. The culprit is amatoxin, a potent hepatotoxin that targets the liver, leading to organ failure within days if left untreated.
Symptoms of Death Cap poisoning are deceptively delayed, often appearing 6 to 24 hours after consumption. Initially, victims may experience nausea, vomiting, and diarrhea, which can be mistaken for food poisoning. However, as the toxin wreaks havoc on the liver, more severe symptoms emerge, including jaundice, seizures, and kidney failure. Without immediate medical intervention, the mortality rate can soar to 50% or higher. Even those who survive often face long-term complications, such as permanent liver damage or the need for a transplant.
To mitigate the risk of fatal outcomes, swift action is critical. If ingestion is suspected, induce vomiting immediately and seek emergency medical care. Hospitals may administer activated charcoal to absorb remaining toxins and provide supportive care, such as intravenous fluids and electrolyte management. In severe cases, a liver transplant may be the only lifesaving option. Time is of the essence; delays in treatment significantly reduce the chances of survival.
Prevention is the most effective strategy. Foraging for mushrooms without expert knowledge is a gamble with life. Always consult a mycologist or use a reliable field guide when identifying fungi. Avoid consuming any mushroom unless you are 100% certain of its safety. Educating children about the dangers of wild mushrooms and teaching them to never touch or taste unknown fungi can also prevent accidental poisoning. The Death Cap’s lethal potential serves as a stark reminder that nature’s beauty can sometimes conceal deadly threats.
Mushrooms and Ascorbic Acid: Unveiling Their Nutritional Synergy
You may want to see also
Frequently asked questions
Immediate symptoms can include nausea, vomiting, diarrhea, abdominal pain, and cramps, often appearing within 6 to 24 hours after ingestion.
Yes, some poisonous mushrooms contain toxins that can cause severe organ damage, such as liver or kidney failure, and can be fatal if not treated promptly.
No, not all poisonous mushrooms are deadly. Some cause mild gastrointestinal symptoms, while others can lead to life-threatening conditions depending on the species and amount consumed.
It’s difficult to identify poisonous mushrooms based on appearance alone, as many toxic and edible species look similar. Always consult an expert or avoid wild mushrooms altogether.
Seek medical attention immediately. Call poison control or go to the emergency room, and if possible, bring a sample of the mushroom for identification.