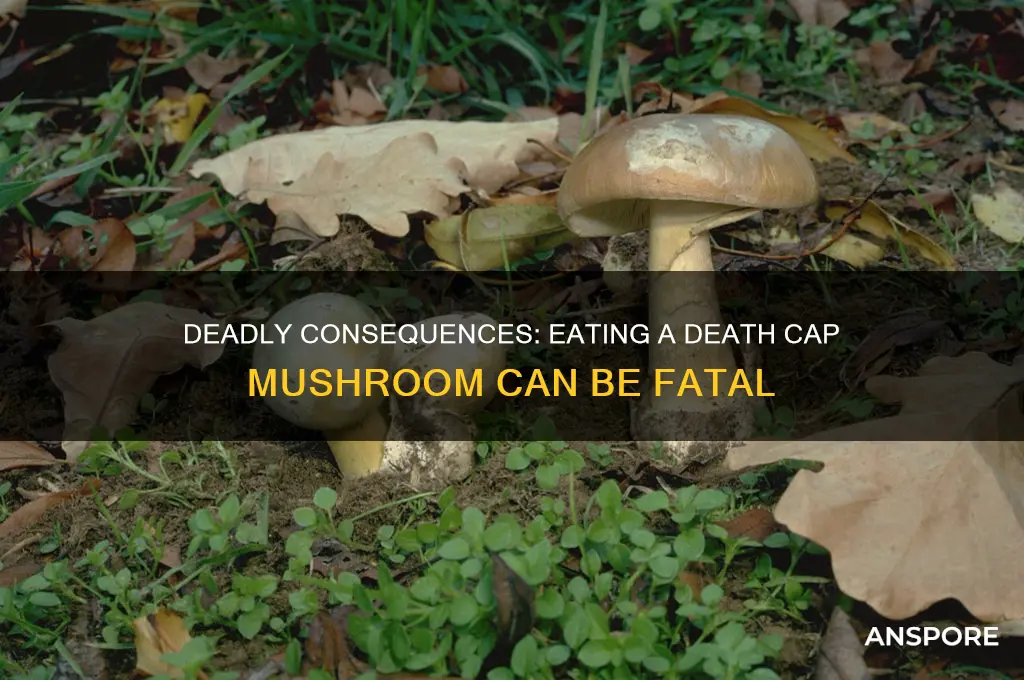
The death cap mushroom, scientifically known as *Amanita phalloides*, is one of the most poisonous fungi in the world, responsible for the majority of fatal mushroom poisonings globally. Ingesting even a small amount can lead to severe symptoms, typically appearing 6 to 24 hours after consumption, as the toxins—primarily amatoxins—begin to damage the liver and kidneys. Early signs include gastrointestinal distress, such as vomiting, diarrhea, and abdominal pain, which may temporarily subside, giving a false sense of recovery. However, within 24 to 48 hours, life-threatening complications like liver failure, kidney dysfunction, and electrolyte imbalances can develop, often requiring immediate medical intervention, including liver transplantation in severe cases. Without prompt treatment, the mortality rate can exceed 50%, making it crucial to avoid misidentifying this deadly mushroom for edible varieties.
| Characteristics | Values |
|---|---|
| Scientific Name | Amanita phalloides |
| Common Name | Death Cap |
| Toxicity | Extremely toxic; contains amatoxins (e.g., alpha-amanitin) |
| Symptoms (Early) | Asymptomatic for 6–24 hours after ingestion |
| Symptoms (Later) | Severe gastrointestinal distress (vomiting, diarrhea, abdominal pain) |
| Organ Damage | Liver and kidney failure due to amatoxin accumulation |
| Fatality Rate | 10–50% without treatment; higher without medical intervention |
| Treatment | Activated charcoal, gastric lavage, supportive care, liver transplant |
| Onset of Symptoms | 6–24 hours after ingestion |
| Duration of Symptoms | 2–3 days of severe symptoms, followed by potential organ failure |
| Misidentification Risk | Often mistaken for edible mushrooms like straw mushrooms or caesar’s mushroom |
| Geographic Distribution | Widespread in Europe, North America, Australia, and New Zealand |
| Prevention | Avoid foraging without expert knowledge; cook all wild mushrooms thoroughly |
| Antidote | None specific; treatment focuses on symptom management and organ support |
| Long-Term Effects | Survivors may experience chronic liver damage or require long-term care |
| Appearance | Greenish-yellow cap, white gills, bulbous base with cup-like volva |
Explore related products
What You'll Learn
- Rapid Onset Symptoms: Nausea, vomiting, diarrhea, and abdominal pain begin 6-24 hours after ingestion
- Liver and Kidney Failure: Toxins destroy liver and kidney cells, leading to organ shutdown
- Neurological Effects: Confusion, seizures, and coma may occur as toxins affect the brain
- Delayed Symptoms: Initial recovery can be followed by severe organ failure 3-5 days later
- Treatment and Survival: Immediate medical care, including liver transplant, is critical for survival

Rapid Onset Symptoms: Nausea, vomiting, diarrhea, and abdominal pain begin 6-24 hours after ingestion
The rapid onset symptoms following the ingestion of a death cap mushroom (*Amanita phalloides*) are a critical indicator of poisoning and require immediate attention. Typically, these symptoms manifest 6 to 24 hours after consumption, a delay that often lulls victims into a false sense of security. During this latency period, the toxins in the mushroom, primarily alpha-amanitin, are absorbed into the bloodstream and begin to wreak havoc on the body. The first signs of toxicity are gastrointestinal in nature, as the toxins irritate the stomach and intestinal lining. Nausea is often the initial symptom, presenting as a sudden and intense feeling of discomfort or the urge to vomit. This is quickly followed by vomiting, which can be severe and persistent, leading to dehydration if not managed promptly.
As the toxins continue to affect the digestive system, diarrhea develops, often watery and profuse. This symptom, combined with vomiting, can rapidly deplete the body’s fluids and electrolytes, further exacerbating the condition. The abdominal pain that accompanies these symptoms is typically described as cramping or sharp and localized to the stomach area. This pain is a direct result of the inflammation and damage caused by alpha-amanitin to the liver and gastrointestinal tract. The combination of these symptoms—nausea, vomiting, diarrhea, and abdominal pain—creates a cycle of distress that can be both physically and mentally exhausting for the victim.
It is crucial to recognize that these rapid onset symptoms are not merely a case of food poisoning but a sign of a life-threatening toxin at work. The delay between ingestion and symptom onset often leads individuals to underestimate the severity of the situation. However, the damage to the liver, which is the primary target of alpha-amanitin, is already underway during this phase. The gastrointestinal symptoms are the body’s initial response to the toxin, but they are just the beginning of a potentially fatal progression if treatment is not sought immediately.
If you or someone you know experiences these symptoms after consuming wild mushrooms, especially if a death cap is suspected, seek emergency medical attention immediately. Do not wait for symptoms to worsen, as the latency period can be deceptive. Medical professionals can administer activated charcoal to reduce toxin absorption, provide intravenous fluids to combat dehydration, and initiate liver-protecting treatments. Time is of the essence, as the rapid onset symptoms are a clear warning that the body is under attack by one of the most deadly toxins found in nature.
In summary, the rapid onset symptoms of nausea, vomiting, diarrhea, and abdominal pain following death cap ingestion are a medical emergency. These symptoms, appearing 6 to 24 hours after consumption, signal the beginning of a toxic cascade that can lead to liver failure and death if untreated. Awareness of these signs and swift action are critical to improving the chances of survival. Always avoid consuming wild mushrooms unless they have been positively identified by an expert, as the consequences of a mistake can be irreversible.
Exploring Nature's Fungus Fans: Animals That Eat Mushrooms
You may want to see also

Liver and Kidney Failure: Toxins destroy liver and kidney cells, leading to organ shutdown
The death cap mushroom, scientifically known as *Amanita phalloides*, contains potent toxins that can cause severe and often fatal damage to the body, particularly the liver and kidneys. The primary toxins responsible for this damage are amatoxins, which are cyclic octapeptides that specifically target and destroy liver and kidney cells. When ingested, these toxins are rapidly absorbed into the bloodstream and transported to the liver, where they begin their destructive process. Amatoxins inhibit RNA polymerase II, a crucial enzyme for protein synthesis, leading to cell death in the liver and kidneys. This cellular destruction is the first step in the cascade of events that can result in organ failure.
Within 6 to 24 hours after ingestion, symptoms such as abdominal pain, vomiting, and diarrhea may appear, often misleadingly suggesting a simple case of food poisoning. However, as the toxins continue to wreak havoc on the liver and kidneys, more severe symptoms emerge. The liver, responsible for detoxifying the blood and regulating metabolism, begins to fail as its cells are systematically destroyed. This leads to a condition known as acute liver failure, characterized by jaundice, confusion, and coagulation disorders. Simultaneously, the kidneys, which filter waste from the blood and regulate fluid balance, also suffer irreversible damage, resulting in acute kidney injury. The inability of these organs to perform their essential functions sets the stage for a rapid decline in overall health.
As liver and kidney function deteriorates, toxins and waste products accumulate in the bloodstream, further exacerbating the condition. Elevated levels of ammonia, a byproduct of protein metabolism, can lead to hepatic encephalopathy, causing confusion, drowsiness, and even coma. The kidneys' failure to filter waste results in electrolyte imbalances and fluid retention, which can lead to swelling, high blood pressure, and cardiovascular instability. Without prompt and aggressive medical intervention, this dual organ failure becomes irreversible, often culminating in multiple organ dysfunction syndrome (MODS) and death.
Treatment for death cap mushroom poisoning focuses on supportive care and attempts to mitigate toxin effects. Gastric decontamination, such as induced vomiting or activated charcoal, may be used if ingestion is recent. Intravenous fluids are administered to maintain hydration and support kidney function, while medications like N-acetylcysteine and silibinin may be used to protect liver cells. In severe cases, liver transplantation may be the only lifesaving option, though it is not always feasible due to the rapid progression of the disease. Early recognition and medical intervention are critical, as the toxins' destructive effects on the liver and kidneys can be swift and unforgiving.
Prevention remains the most effective strategy against death cap mushroom poisoning. Proper identification of mushrooms before consumption is essential, as the death cap closely resembles edible species. Education and awareness are key, especially in regions where these mushrooms are prevalent. If ingestion is suspected, immediate medical attention is imperative, as the toxins' impact on the liver and kidneys can be irreversible within a short timeframe. Understanding the deadly consequences of these toxins underscores the importance of caution and vigilance when foraging for wild mushrooms.
Delicious Seafood Mushroom Recipes: A Beginner's Guide to Cooking
You may want to see also

Neurological Effects: Confusion, seizures, and coma may occur as toxins affect the brain
The death cap mushroom, scientifically known as *Amanita phalloides*, contains potent toxins that can wreak havoc on the human body, particularly the nervous system. Among the most alarming consequences of ingestion are the neurological effects, which manifest as the toxins begin to interfere with brain function. Initial symptoms often include confusion, where the victim may experience disorientation, difficulty concentrating, and an inability to think clearly. This confusion arises as the toxins disrupt normal neurotransmitter activity, impairing the brain’s ability to process information effectively. It is crucial to recognize these early signs, as they are often the first indicators of poisoning and require immediate medical attention.
As the toxins continue to affect the brain, more severe neurological symptoms can emerge, including seizures. These seizures occur due to the toxins' interference with the electrical activity in the brain, leading to uncontrolled, abnormal movements and loss of consciousness. Seizures are a medical emergency and can cause further damage if not promptly treated. The onset of seizures is a clear sign that the poisoning is progressing rapidly, and the individual’s condition is deteriorating. At this stage, hospitalization is imperative to manage the seizures and prevent complications such as injury or respiratory distress.
In the most severe cases, the neurological effects of death cap mushroom poisoning can escalate to coma. A coma is a state of profound unconsciousness where the individual is unresponsive to external stimuli. This occurs as the toxins cause widespread damage to brain cells, leading to a catastrophic failure of brain function. The induction of a coma is a life-threatening condition and often indicates that multiple organ systems are failing, including the liver and kidneys, which are also targeted by the mushroom’s toxins. Immediate intensive care, including supportive therapies and, in some cases, liver transplantation, may be required to save the individual’s life.
It is important to note that the progression from confusion to seizures and eventually coma is not inevitable in all cases, but it underscores the severity of death cap mushroom poisoning. The speed and intensity of these neurological effects depend on factors such as the amount of mushroom consumed, the individual’s overall health, and the timing of medical intervention. However, even in milder cases, neurological symptoms should never be underestimated, as they can rapidly worsen without treatment. Prevention is key, and avoiding the consumption of wild mushrooms, especially those resembling the death cap, is the most effective way to prevent these devastating effects.
In summary, the neurological effects of death cap mushroom poisoning are a direct result of toxins targeting the brain, leading to confusion, seizures, and potentially coma. These symptoms are not only life-threatening but also indicative of the broader systemic damage caused by the mushroom’s toxins. Recognizing the early signs of confusion and seeking immediate medical help can significantly improve outcomes. Public awareness and education about the dangers of the death cap mushroom are essential to prevent accidental ingestion and the severe neurological consequences that follow.
Delicious Mushroom Snack Ideas: Easy, Healthy, and Tasty Ways to Enjoy
You may want to see also
Explore related products
$14.99

Delayed Symptoms: Initial recovery can be followed by severe organ failure 3-5 days later
The delayed symptoms of death cap mushroom (Amanita phalloides) poisoning are particularly insidious and life-threatening. After an initial period of apparent recovery, typically 24 to 48 hours after ingestion, the toxins in the mushroom begin to wreak havoc on the body’s organs. This second phase of poisoning is marked by severe organ failure, primarily affecting the liver and kidneys, which can lead to rapid deterioration of health and, if untreated, death. The toxins, known as amatoxins, are not destroyed by cooking or digestion and continue to cause damage even after the initial symptoms seem to subside.
During the initial recovery phase, victims may feel better, leading them to believe the danger has passed. However, this is a critical deception. Amatoxins silently infiltrate liver cells, disrupting protein synthesis and causing irreversible damage. By the time symptoms reappear, often 3 to 5 days after ingestion, the liver may already be in acute failure. Early signs of this phase include jaundice (yellowing of the skin and eyes), dark urine, and abdominal swelling due to fluid accumulation. These symptoms indicate that the liver is struggling to perform its vital functions, such as filtering toxins and producing bile.
Kidney failure often accompanies liver failure in death cap poisoning, further complicating the prognosis. The kidneys, responsible for filtering waste from the blood, become overwhelmed by the toxins and the body’s inflammatory response. This can lead to a dangerous buildup of waste products in the blood, a condition known as azotemia, and eventually kidney shutdown. Symptoms of kidney failure include reduced urine output, swelling in the legs and face, and confusion or difficulty thinking clearly due to the accumulation of toxins in the brain.
The delayed onset of organ failure makes death cap poisoning particularly challenging to treat. By the time symptoms reappear, the damage is often extensive and irreversible. Immediate medical intervention, including supportive care, liver transplantation in severe cases, and medications to stabilize organ function, is crucial. However, even with aggressive treatment, the mortality rate remains high, emphasizing the importance of early identification and intervention. Anyone suspected of ingesting a death cap mushroom should seek medical attention immediately, even if they feel better initially, as this could be the calm before the storm of severe organ failure.
Prevention is the best defense against death cap poisoning. Accurate identification of mushrooms is critical, as death caps closely resemble edible species like the straw mushroom or young puffballs. When in doubt, avoid consumption altogether. Public education and awareness campaigns can help reduce the incidence of poisoning, but if ingestion occurs, time is of the essence. Recognizing the potential for delayed symptoms and acting swiftly can mean the difference between life and death.
Are Leftover Mushrooms Safe to Eat? A Complete Guide
You may want to see also

Treatment and Survival: Immediate medical care, including liver transplant, is critical for survival
If someone ingests a death cap mushroom (*Amanita phalloides*), immediate and aggressive medical intervention is crucial for survival. The toxins in the mushroom, primarily alpha-amanitin, cause severe liver damage, often leading to liver failure within 24 to 48 hours of ingestion. The first step in treatment is to seek emergency medical care without delay. Time is of the essence, as the toxins begin to cause irreversible damage rapidly. Upon arrival at a medical facility, healthcare providers will likely administer activated charcoal to reduce further absorption of the toxins, though this is most effective if given within the first few hours after ingestion.
The cornerstone of treatment for death cap poisoning is supportive care to stabilize the patient while the body attempts to eliminate the toxins. This includes intravenous fluids to maintain hydration, electrolyte balance, and medications to manage symptoms such as nausea, vomiting, and abdominal pain. Continuous monitoring of liver function is essential, as the toxins specifically target liver cells, leading to acute liver failure. Blood tests will be performed regularly to assess liver enzymes, coagulation factors, and kidney function, as the toxins can also affect the kidneys.
In severe cases, a liver transplant may be the only life-saving option. Alpha-amanitin causes extensive destruction of liver cells, and once liver failure occurs, the damage is often irreversible. Patients with signs of liver failure, such as jaundice, confusion, and coagulation disorders, will be evaluated for transplant eligibility. The decision to proceed with a transplant is complex and depends on factors like the availability of a donor organ, the patient’s overall health, and the extent of organ damage. However, liver transplantation has been shown to significantly improve survival rates in death cap poisoning cases.
Early administration of certain medications, such as silibinin (an active compound in milk thistle), has been explored as a potential treatment to protect liver cells from toxin damage. While not a substitute for transplantation in severe cases, these therapies may buy critical time and improve outcomes when used in conjunction with other treatments. Additionally, techniques like plasmapheresis, which filters toxins from the blood, have been used experimentally but are not yet standard practice.
Survival after ingesting a death cap mushroom depends heavily on the speed and effectiveness of medical intervention. Delayed treatment significantly reduces the chances of recovery, as the toxins act quickly and relentlessly. Public awareness of the dangers of death cap mushrooms and the importance of immediate medical care cannot be overstated. If ingestion is suspected, contacting poison control or emergency services immediately is vital. With prompt and comprehensive treatment, including liver transplantation when necessary, survival is possible, but the window of opportunity is narrow, making rapid action critical.
Dried Baby Bella Mushrooms: Nutritious, Tasty, and Worth Eating?
You may want to see also
Frequently asked questions
Immediate symptoms typically appear 6–24 hours after ingestion and include severe abdominal pain, vomiting, diarrhea, and dehydration. These symptoms are often mistaken for food poisoning.
Yes, consuming a death cap mushroom can be fatal. It contains potent toxins (amatoxins) that cause liver and kidney failure, often leading to death if not treated promptly.
There is no specific antidote, but treatment includes supportive care, activated charcoal, and, in severe cases, liver transplantation. Early medical intervention is critical for survival.
Avoid foraging for wild mushrooms unless you are an expert. Death caps resemble edible mushrooms like paddy straw mushrooms, so always verify with a knowledgeable source before consuming any wild fungi.