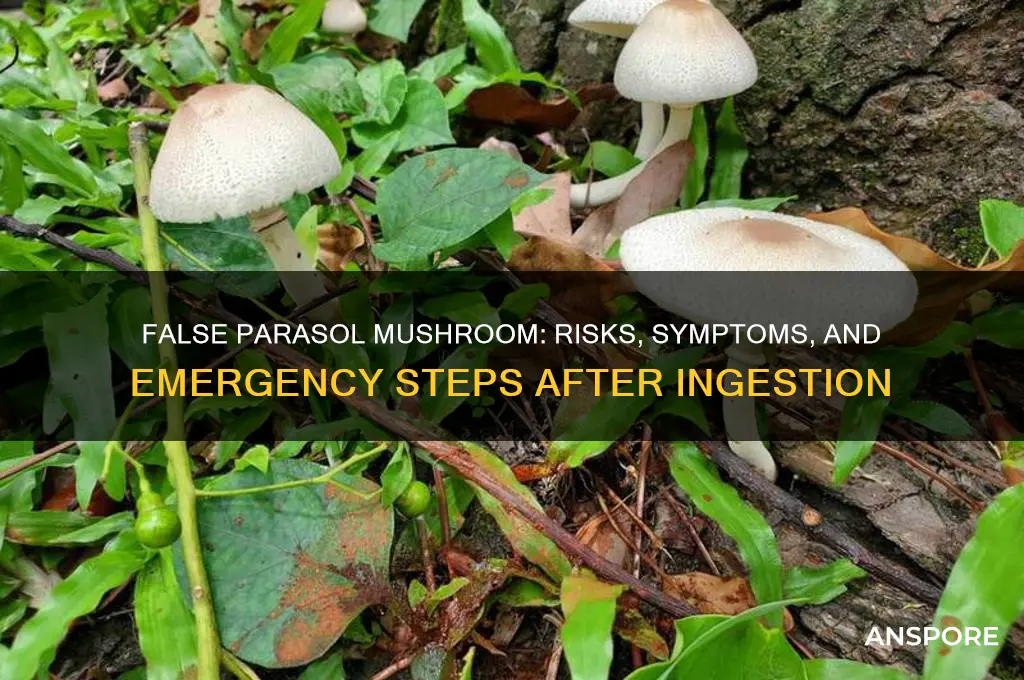
Eating a false parasol mushroom, often mistaken for its edible counterpart due to its similar appearance, can lead to severe health risks. The false parasol, scientifically known as *Chlorophyllum molybdites*, contains toxins that cause gastrointestinal distress, including nausea, vomiting, diarrhea, and abdominal pain, typically within a few hours of ingestion. While rarely fatal, the symptoms can be intense and require medical attention, especially for children or individuals with compromised health. Proper identification by an expert is crucial, as misidentification can easily occur, highlighting the importance of caution when foraging wild mushrooms.
| Characteristics | Values |
|---|---|
| Scientific Name | Chlorophyllum molybdites |
| Common Names | False Parasol, Green-spored Lepiota |
| Toxicity | Mild to moderately toxic |
| Symptoms | Gastrointestinal distress (nausea, vomiting, diarrhea, abdominal pain) |
| Onset of Symptoms | 30 minutes to 2 hours after ingestion |
| Duration of Symptoms | 4 to 24 hours |
| Treatment | Supportive care (rehydration, rest); medical attention if severe |
| Fatality Risk | Rarely fatal, but can cause severe dehydration in vulnerable individuals |
| Misidentification | Often mistaken for edible parasol mushrooms (Macrolepiota procera) |
| Key Identifier | Greenish spore print, bulbous base with sac-like volva |
| Habitat | Lawns, gardens, wooded areas, often in urban settings |
| Season | Summer and early fall |
| Prevention | Proper identification, avoid foraging without expertise |
Explore related products
What You'll Learn
- Toxic Symptoms: Nausea, vomiting, diarrhea, and abdominal pain occur within hours of ingestion
- Amatoxin Effects: Liver and kidney damage can develop 24-48 hours post-consumption
- Misidentification Risks: Often confused with edible parasol mushrooms due to similar appearance
- Medical Treatment: Immediate hospitalization, activated charcoal, and liver support are critical interventions
- Long-Term Impact: Severe cases may lead to liver failure or require a transplant

Toxic Symptoms: Nausea, vomiting, diarrhea, and abdominal pain occur within hours of ingestion
The false parasol mushroom, scientifically known as *Chlorophyllum molybdites*, is a common cause of mushroom poisoning in many parts of the world. While it resembles the edible parasol mushroom, consuming it can lead to severe gastrointestinal distress. The toxic symptoms typically manifest within hours of ingestion, with nausea being one of the first indicators. This sensation of unease and discomfort in the stomach is often the body’s initial response to the toxins present in the mushroom. It serves as a warning sign that something is amiss, prompting the individual to seek attention or relief.
Following nausea, vomiting is a frequent and immediate reaction to the toxins in the false parasol mushroom. The body attempts to expel the harmful substances by forcing the stomach contents out. This can occur repeatedly, leading to dehydration and further discomfort. Vomiting is a protective mechanism but can also be a source of distress, especially if it persists for an extended period. It is crucial to monitor fluid intake during this phase to prevent complications from dehydration.
Diarrhea is another common symptom that arises shortly after ingestion of the false parasol mushroom. The toxins irritate the lining of the intestines, causing them to secrete excess water and electrolytes. This results in loose, watery stools that can occur frequently. Diarrhea contributes to fluid loss and can lead to electrolyte imbalances if not managed properly. It is essential to replace lost fluids and electrolytes to avoid further health issues.
Abdominal pain accompanies these symptoms, often described as cramping or discomfort in the stomach area. This pain is caused by the inflammation and irritation of the gastrointestinal tract due to the mushroom’s toxins. The intensity of the pain can vary but is typically persistent and may worsen with movement or pressure. Over-the-counter pain relievers may provide temporary relief, but medical attention is necessary to address the underlying cause and prevent complications.
These symptoms—nausea, vomiting, diarrhea, and abdominal pain—are the body’s response to the toxic compounds in the false parasol mushroom. They usually appear within 2 to 24 hours after consumption, depending on the amount ingested and individual sensitivity. If you or someone you know has consumed this mushroom and experiences these symptoms, seek medical help immediately. Prompt treatment, including supportive care and fluid management, can alleviate symptoms and prevent more serious health consequences. Always exercise caution when foraging for mushrooms and consult experts to avoid misidentification.
Are Fairy Ring Mushrooms Safe to Eat? A Comprehensive Guide
You may want to see also

Amatoxin Effects: Liver and kidney damage can develop 24-48 hours post-consumption
The false parasol mushroom, often mistaken for its edible counterpart, contains amatoxins—a group of highly toxic compounds that pose severe health risks if ingested. Amatoxins are cyclic octapeptides that are resistant to heat, drying, and stomach acid, making them particularly dangerous. When consumed, these toxins are rapidly absorbed into the bloodstream and begin to wreak havoc on the body’s vital organs, primarily the liver and kidneys. The effects of amatoxin poisoning are insidious, with symptoms often delayed, which can lead to a false sense of security after ingestion.
Within 24 to 48 hours of consuming a false parasol mushroom, amatoxins start to exert their destructive effects on the liver. These toxins specifically target hepatocytes, the primary cells of the liver, disrupting their structure and function. This leads to acute hepatotoxicity, characterized by severe liver damage. Early signs of liver dysfunction may include nausea, vomiting, abdominal pain, and diarrhea, which are often mistaken for a simple stomach bug. However, as the toxins continue to damage liver cells, more severe symptoms such as jaundice (yellowing of the skin and eyes), dark urine, and light-colored stools may develop. Without prompt medical intervention, this can progress to acute liver failure, a life-threatening condition requiring immediate treatment.
Simultaneously, amatoxins also inflict significant damage on the kidneys, leading to acute kidney injury. The kidneys, responsible for filtering waste and excess fluids from the blood, become compromised as the toxins interfere with their cellular function. This can result in reduced urine output, swelling in the legs or face, and electrolyte imbalances. In severe cases, kidney failure may occur, further complicating the patient’s condition. The dual assault on the liver and kidneys creates a critical situation where the body’s ability to detoxify and maintain homeostasis is severely impaired.
The progression of amatoxin effects is rapid and relentless, often leading to a cascade of organ failures if not treated aggressively. Supportive care is crucial in managing amatoxin poisoning, including intravenous fluids, medications to protect liver and kidney function, and, in severe cases, liver transplantation. Early recognition of symptoms and immediate medical attention are paramount, as delayed treatment significantly increases the risk of fatal outcomes. It is essential to avoid self-diagnosis or home remedies, as only professional medical care can mitigate the toxic effects of amatoxins.
Prevention remains the best approach to avoiding amatoxin poisoning. Proper identification of mushrooms before consumption is critical, as the false parasol mushroom closely resembles edible varieties. When in doubt, consult an expert or avoid consumption altogether. Educating oneself and others about the dangers of toxic mushrooms can save lives and prevent the devastating effects of amatoxin exposure.
Mushrooms: Nutritional Powerhouses or Just a Tasty Fad?
You may want to see also

Misidentification Risks: Often confused with edible parasol mushrooms due to similar appearance
The false parasol mushroom, scientifically known as *Chlorophyllum molybdites*, poses significant misidentification risks due to its striking resemblance to edible parasol mushrooms like *Macrolepiota procera*. Both species share similar features, such as large caps, prominent gills, and a central stalk, making it easy for foragers to mistake one for the other. However, consuming *Chlorophyllum molybdites* can lead to severe gastrointestinal distress, including nausea, vomiting, diarrhea, and abdominal pain, typically within 1 to 3 hours of ingestion. This similarity in appearance underscores the critical need for careful identification before consuming any wild mushrooms.
One of the primary challenges in distinguishing between the false parasol and its edible counterpart lies in their physical characteristics. Both mushrooms have a creamy white to light brown cap that can reach impressive sizes, often with a similar scaly or flaky texture. The gills of both species are closely spaced and white when young, turning darker with age. However, subtle differences exist: the false parasol often has a greener spore print and its gills may develop a greenish tinge as it matures, a feature not typically seen in edible parasols. Foragers must pay close attention to these details, as overlooking them can lead to accidental poisoning.
Another factor contributing to misidentification is the habitat in which these mushrooms grow. Both false parasols and edible parasols thrive in similar environments, such as grassy areas, lawns, and woodland edges, often appearing in large clusters. This overlap in habitat increases the likelihood of confusion, especially for inexperienced foragers who may rely on location as a clue. It is essential to remember that habitat alone is not a reliable identifier, and thorough examination of the mushroom's physical traits is crucial.
The consequences of misidentifying a false parasol mushroom are not life-threatening in most cases, but the resulting symptoms can be extremely unpleasant. Unlike some toxic mushrooms that cause organ failure or long-term damage, *Chlorophyllum molybdites* primarily affects the digestive system. However, severe dehydration from vomiting and diarrhea can occur, particularly in children, the elderly, or individuals with compromised immune systems. Prompt medical attention is advised if symptoms persist or worsen, though most cases resolve within 24 hours with proper hydration and rest.
To minimize the risk of misidentification, foragers should adopt a multi-step approach to mushroom identification. This includes examining the spore print, observing the color and texture of the gills and cap, and noting any changes in appearance as the mushroom ages. Consulting field guides, using reputable online resources, and seeking guidance from experienced mycologists can also provide valuable support. When in doubt, the safest rule is to avoid consumption altogether, as the potential risks far outweigh the benefits of a meal. Awareness and caution are key to safely enjoying the bounty of wild mushrooms while avoiding the pitfalls of misidentification.
Portobello Mushrooms and Pregnancy: Safe or Risky for Expecting Moms?
You may want to see also
Explore related products

Medical Treatment: Immediate hospitalization, activated charcoal, and liver support are critical interventions
If someone ingests a false parasol mushroom (often confused with edible parasol mushrooms), immediate medical attention is crucial due to its potential toxicity. The false parasol mushroom, scientifically known as *Chlorophyllum molybdites*, contains toxins that can cause severe gastrointestinal symptoms, including nausea, vomiting, diarrhea, and abdominal pain. These symptoms typically appear within 1 to 3 hours after ingestion and can be debilitating. Immediate hospitalization is essential to monitor the patient’s condition and prevent complications, especially in severe cases or when ingested in large quantities.
Upon arrival at the hospital, one of the first interventions is the administration of activated charcoal. This treatment is most effective when given within the first hour of ingestion but can still be beneficial up to six hours afterward. Activated charcoal binds to the toxins in the gastrointestinal tract, preventing their absorption into the bloodstream. This step is critical in reducing the severity of poisoning and minimizing the risk of systemic effects. However, it should only be administered by healthcare professionals to ensure proper dosage and avoid complications such as aspiration.
Simultaneously, liver support becomes a critical intervention, as the toxins in *Chlorophyllum molybdites* can cause hepatotoxicity, or liver damage. The liver is responsible for filtering toxins from the blood, and severe poisoning can overwhelm its capacity, leading to elevated liver enzymes and, in extreme cases, liver failure. Medical professionals may monitor liver function through blood tests and provide supportive care, such as intravenous fluids to maintain hydration and electrolyte balance. In severe cases, medications to protect liver function or even liver transplantation may be considered, though these are rare.
In addition to activated charcoal and liver support, symptomatic treatment is essential to manage the patient’s discomfort. Antiemetics may be prescribed to control nausea and vomiting, while antidiarrheal medications can help alleviate gastrointestinal distress. Pain management is also important, as abdominal pain can be intense. Patients are typically kept under observation for at least 24 hours to ensure symptoms do not worsen and to monitor for any signs of organ damage.
Finally, patient education and prevention are key components of long-term management. Mushroom poisoning is often the result of misidentification, so educating individuals about the risks of foraging and the importance of proper identification is vital. Encouraging people to consult mycologists or use reliable guides when collecting mushrooms can prevent accidental ingestion. In the event of suspected poisoning, contacting a poison control center or seeking medical help immediately can significantly improve outcomes. Prompt and appropriate medical treatment, including hospitalization, activated charcoal, and liver support, remains the cornerstone of managing false parasol mushroom toxicity.
Magic Mushrooms and Nausea: Why Some People Vomit After Consumption
You may want to see also

Long-Term Impact: Severe cases may lead to liver failure or require a transplant
Consuming a false parasol mushroom (often confused with edible parasol mushrooms) can have devastating long-term consequences due to its toxic properties. These mushrooms contain amatoxins, which are highly poisonous compounds that specifically target the liver. While symptoms may initially appear as gastrointestinal distress—such as nausea, vomiting, and diarrhea—the real danger lies in the delayed onset of severe liver damage. If left untreated, the toxins can cause irreversible harm to liver cells, leading to long-term complications that may culminate in liver failure.
In severe cases, the liver’s ability to function is compromised to such an extent that it can no longer perform its vital roles, such as filtering toxins, regulating blood composition, and aiding digestion. This failure is not immediate but develops over days or weeks as the amatoxins continue to damage liver tissue. Patients may experience jaundice, abdominal swelling, and confusion as the liver’s deterioration progresses. At this stage, medical intervention becomes critical to prevent fatal outcomes.
When liver failure occurs due to false parasol mushroom poisoning, a liver transplant may become the only viable treatment option. This is particularly true if the damage is so extensive that the liver cannot recover on its own. However, liver transplants are complex procedures with significant risks, including rejection of the new organ, lifelong immunosuppression, and the potential for complications from surgery. The availability of donor organs also poses a challenge, as the demand often exceeds supply, leaving some patients in a critical, time-sensitive situation.
Even after a successful transplant, survivors face long-term challenges. They must adhere to strict medication regimens to prevent organ rejection and undergo regular medical monitoring. Additionally, the psychological impact of such a severe health event cannot be overlooked, as patients may experience anxiety, depression, or post-traumatic stress disorder. The financial burden of ongoing medical care and lifestyle adjustments further compounds the long-term impact of this poisoning.
Prevention remains the most effective strategy to avoid these dire consequences. Proper identification of mushrooms before consumption is crucial, as the false parasol closely resembles its edible counterpart. Educating oneself about mushroom foraging or consulting experts can significantly reduce the risk of accidental poisoning. In the event of ingestion, immediate medical attention is essential, as early treatment with activated charcoal, antidotes, and supportive care can mitigate the severity of long-term liver damage and the need for a transplant.
Delicious and Safe: A Guide to Edible Mushrooms for Foodies
You may want to see also
Frequently asked questions
Symptoms can include severe gastrointestinal distress, such as nausea, vomiting, diarrhea, abdominal pain, and dehydration. In some cases, liver and kidney damage may occur, leading to more serious health complications.
Symptoms typically appear within 6 to 24 hours after ingestion, depending on the amount consumed and individual sensitivity.
While fatalities are rare, severe poisoning can occur, especially if medical treatment is delayed. Prompt medical attention is crucial to prevent life-threatening complications.
False parasol mushrooms often have a bulbous base with a volva (cup-like structure) and may have a greenish or yellowish tinge. Edible parasol mushrooms usually lack a volva and have a more uniform white or cream color. Always consult an expert if unsure.
Seek immediate medical attention. Call poison control or go to the nearest emergency room. Do not induce vomiting unless instructed by a medical professional, and bring a sample of the mushroom for identification if possible.