Consuming a poisonous mushroom can have severe and potentially life-threatening consequences, as many toxic species contain potent toxins that can cause symptoms ranging from gastrointestinal distress, such as nausea, vomiting, and diarrhea, to more serious effects like organ failure, neurological damage, or even death. The severity of the reaction depends on the type of mushroom ingested, the amount consumed, and the individual's overall health. Some mushrooms, like the Death Cap (*Amanita phalloides*), contain toxins that can cause liver and kidney damage, while others, like the Destroying Angel (*Amanita bisporigera*), can lead to respiratory failure. Immediate medical attention is crucial if poisoning is suspected, as prompt treatment, including gastric decontamination, supportive care, and, in some cases, specific antidotes, can significantly improve outcomes. However, misidentification of mushrooms is common, making it essential to avoid foraging wild mushrooms without expert knowledge.
| Characteristics | Values |
|---|---|
| Symptoms Onset | Varies from 20 minutes to 24 hours after ingestion, depending on the mushroom species. |
| Gastrointestinal Symptoms | Nausea, vomiting, abdominal pain, diarrhea, and cramps are common in many cases. |
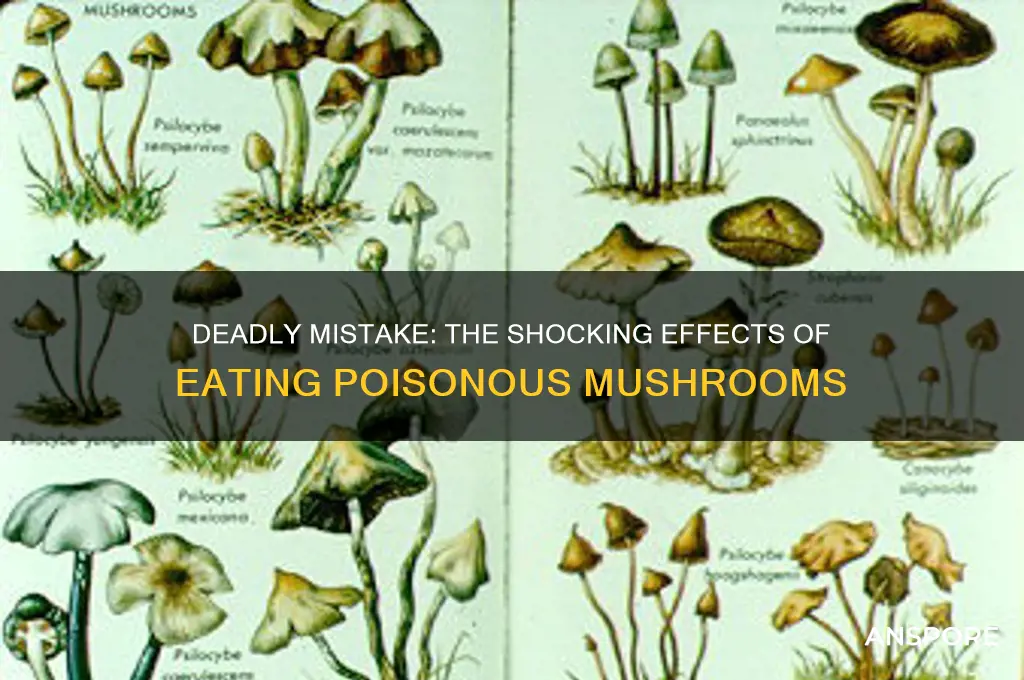
| Neurological Symptoms | Hallucinations, confusion, seizures, drowsiness, or coma in severe cases (e.g., Amanita muscaria, Psilocybe species). |
| Liver and Kidney Damage | Acute liver failure (e.g., Amanita phalloides, "Death Cap") or kidney damage in severe poisonings. |
| Cardiovascular Effects | Low blood pressure, irregular heartbeat, or heart failure in extreme cases. |
| Respiratory Distress | Difficulty breathing or respiratory failure in rare, severe poisonings. |
| Long-Term Effects | Permanent organ damage (liver, kidneys) or death in untreated severe cases. |
| Fatality Risk | High with certain species (e.g., Amanita phalloides, Galerina marginata) if not treated promptly. |
| Treatment | Gastric decontamination, activated charcoal, supportive care, and in severe cases, liver transplantation. |
| Prevention | Avoid consuming wild mushrooms unless identified by an expert mycologist. |
Explore related products
What You'll Learn
- Symptoms of Poisoning: Nausea, vomiting, diarrhea, abdominal pain, dizziness, confusion, hallucinations, and organ failure
- Types of Toxins: Amatoxins, orellanine, muscarine, and coprine cause different symptoms and severity levels
- Time to Onset: Symptoms can appear within minutes to 24 hours after ingestion
- Treatment Options: Gastric lavage, activated charcoal, antidotes, and supportive care are common treatments
- Long-Term Effects: Liver damage, kidney failure, neurological issues, and death can occur in severe cases

Symptoms of Poisoning: Nausea, vomiting, diarrhea, abdominal pain, dizziness, confusion, hallucinations, and organ failure
Consuming a poisonous mushroom can lead to a range of severe symptoms, often appearing within 6 to 24 hours after ingestion, depending on the type of toxin involved. The initial symptoms typically include nausea and vomiting, which are the body’s natural defense mechanisms to expel the toxin. These symptoms can be intense and persistent, causing significant discomfort. Diarrhea often follows, further dehydrating the individual and exacerbating the body’s stress. These gastrointestinal symptoms are the body’s immediate response to the toxins present in the mushroom and should never be ignored, as they are early warning signs of poisoning.
As the toxins continue to affect the body, abdominal pain becomes a prominent symptom. This pain can range from mild cramping to severe, unrelenting discomfort, often localized in the stomach area. The pain is a result of the toxins irritating the gastrointestinal tract and can be a sign of deeper tissue damage. Alongside abdominal pain, individuals may experience dizziness, which can make it difficult to stand or walk. This dizziness is often accompanied by a general feeling of weakness and fatigue, further complicating the individual’s ability to seek help.
The neurological symptoms of mushroom poisoning can be particularly alarming. Confusion is a common sign that the toxins are affecting the brain, leading to disorientation and difficulty thinking clearly. In more severe cases, hallucinations may occur, causing the individual to see, hear, or feel things that are not real. These symptoms are indicative of the toxin’s impact on the central nervous system and require immediate medical attention. Hallucinations can be distressing and may lead to dangerous behavior if the individual is not monitored closely.
One of the most critical and life-threatening consequences of mushroom poisoning is organ failure. Certain toxins, such as amatoxins found in the Death Cap mushroom, can cause severe damage to the liver and kidneys. Symptoms of organ failure may include jaundice (yellowing of the skin and eyes), decreased urine output, and swelling in the abdomen or legs. Organ failure is a medical emergency and requires urgent treatment, including hospitalization, supportive care, and, in some cases, organ transplantation. Early recognition of the symptoms and prompt medical intervention are crucial to prevent fatal outcomes.
In summary, the symptoms of mushroom poisoning—nausea, vomiting, diarrhea, abdominal pain, dizziness, confusion, hallucinations, and organ failure—can progress rapidly and are highly dependent on the type of mushroom consumed. If there is any suspicion of mushroom poisoning, it is essential to seek medical help immediately. Bringing a sample of the mushroom, if available, can aid in identification and treatment. Time is of the essence in these cases, as delayed treatment can lead to irreversible damage or death. Always exercise caution and avoid consuming wild mushrooms unless they have been positively identified by an expert.
Mastering Mushroom Meals: A Beginner's Guide to Eating Mushrooms
You may want to see also

Types of Toxins: Amatoxins, orellanine, muscarine, and coprine cause different symptoms and severity levels
Mushroom poisoning can lead to a range of symptoms, from mild gastrointestinal discomfort to severe organ failure, depending on the type of toxin ingested. Among the most dangerous toxins found in poisonous mushrooms are amatoxins, orellanine, muscarine, and coprine, each causing distinct symptoms and varying levels of severity. Understanding these toxins is crucial for recognizing poisoning and seeking appropriate medical treatment.
Amatoxins, primarily found in mushrooms like the Death Cap (*Amanita phalloides*) and Destroying Angel (*Amanita bisporigera*), are among the most lethal toxins. They cause severe liver and kidney damage by inhibiting RNA polymerase II, a crucial enzyme for protein synthesis. Symptoms initially include vomiting, diarrhea, and abdominal pain, which may subside after a few days, giving a false sense of recovery. However, within 2–3 days, liver and kidney failure can occur, leading to jaundice, seizures, coma, and potentially death if untreated. Amatoxin poisoning requires immediate medical intervention, often including liver transplantation in severe cases.
Orellanine, found in mushrooms like the Fool’s Webcap (*Cortinarius orellanus*), targets the kidneys rather than the liver. Symptoms typically appear 2–3 days after ingestion and include nausea, vomiting, and lower back pain, indicative of kidney damage. Unlike amatoxins, orellanine poisoning does not cause gastrointestinal symptoms initially, making it harder to diagnose early. Prolonged exposure can lead to acute tubular necrosis, a severe kidney injury that may result in renal failure. Treatment focuses on supportive care and dialysis if necessary, but recovery can be slow and incomplete.
Muscarine, named after the mushroom genus *Clitocybe* (e.g., *Clitocybe dealbata*), acts on the muscarinic acetylcholine receptors in the body. Symptoms appear quickly, within 15–30 minutes of ingestion, and include excessive sweating, salivation, tearing, abdominal cramps, and diarrhea. In severe cases, it can cause blurred vision, bronchial secretions, and respiratory distress. Muscarine poisoning is rarely fatal and can be treated with anticholinergic medications to counteract the toxin’s effects.
Coprine, found in mushrooms like the Tippler’s Bane (*Coprinus atramentarius*), causes a unique reaction when combined with alcohol consumption. Within minutes to hours of drinking alcohol after ingesting coprine, individuals experience flushing, nausea, vomiting, rapid heartbeat, and anxiety. This reaction is similar to that caused by disulfiram, a drug used to treat alcoholism. While not life-threatening, the symptoms can be extremely uncomfortable. Treatment involves avoiding alcohol and managing symptoms until the toxin is metabolized.
In summary, the toxins amatoxins, orellanine, muscarine, and coprine cause distinct symptoms and severity levels, ranging from mild discomfort to organ failure and death. Recognizing the type of mushroom ingested and its associated toxin is critical for effective treatment. Immediate medical attention is essential in suspected cases of mushroom poisoning, as early intervention can significantly improve outcomes.
Delicious Chanterelle Mushrooms: A Guide to Preparation and Enjoyment
You may want to see also

Time to Onset: Symptoms can appear within minutes to 24 hours after ingestion
The time it takes for symptoms to appear after ingesting a poisonous mushroom can vary widely, typically ranging from minutes to 24 hours. This variability depends on the type of mushroom consumed and the specific toxins it contains. For instance, mushrooms containing amatoxins, such as the Death Cap (*Amanita phalloides*), often have a delayed onset of symptoms. Initially, you might feel fine for 6 to 24 hours after ingestion, which can falsely reassure you that the mushroom was safe. However, this latency period is followed by severe symptoms like vomiting, diarrhea, and abdominal pain, which can progress to liver and kidney failure if left untreated.
On the other hand, mushrooms containing muscarine or ibotenic acid, such as certain species of *Clitocybe* or *Inocybe*, can cause symptoms to appear much faster, often within 15 to 30 minutes. These symptoms may include excessive sweating, salivation, tearing, abdominal cramps, and confusion. The rapid onset is a critical indicator that immediate medical attention is required to prevent complications. Similarly, mushrooms with giromitrin toxins, like the False Morel (*Gyromitra esculenta*), can cause symptoms within 30 minutes to 2 hours, including nausea, dizziness, and seizures.
Mushrooms containing orellanine, such as the Fool's Parsley (*Athamantha exitox*), have an even longer latency period, with symptoms often appearing 24 to 48 hours after ingestion. However, within the first 24 hours, you might experience mild gastrointestinal discomfort, which can be misleading. The toxin primarily targets the kidneys, leading to severe renal failure if treatment is delayed. This delayed onset underscores the importance of seeking medical help immediately if you suspect mushroom poisoning, even if you feel well initially.
It’s crucial to understand that the time to onset is not a reliable indicator of the mushroom’s toxicity. A quick onset does not necessarily mean the poisoning is less severe, and a delayed onset does not imply it is less dangerous. For example, while symptoms from amatoxin-containing mushrooms take longer to appear, they are often life-threatening. Conversely, rapid-onset symptoms from muscarine toxins, though alarming, may resolve with prompt treatment. If you or someone you know has ingested a wild mushroom and symptoms appear at any point within minutes to 24 hours, immediately contact a poison control center or seek emergency medical care. Do not wait for symptoms to worsen, as early intervention can be life-saving.
In summary, the time to onset of symptoms after eating a poisonous mushroom can range from minutes to 24 hours, depending on the toxin involved. This variability highlights the importance of treating any mushroom ingestion seriously, especially if the mushroom’s identity is uncertain. Always err on the side of caution and seek medical help promptly, even if symptoms seem mild or delayed. Quick action can prevent severe complications and save lives.
Can Turtles Safely Eat Mushrooms? Exploring Their Dietary Habits
You may want to see also
Explore related products

Treatment Options: Gastric lavage, activated charcoal, antidotes, and supportive care are common treatments
If someone ingests a poisonous mushroom, immediate medical intervention is crucial to minimize the risk of severe complications or death. Treatment options are tailored to the type of mushroom and the symptoms presented, but several standard procedures are commonly employed. Gastric lavage, also known as stomach pumping, is often the first step in treatment. This procedure involves flushing the stomach with a saline solution to remove any remaining mushroom fragments and toxins. It is most effective when performed within 1-2 hours of ingestion, as it can significantly reduce the amount of toxin absorbed into the bloodstream. However, its utility diminishes after this window, as the toxins may have already been absorbed.
Another immediate treatment is the administration of activated charcoal, which works by binding to toxins in the gastrointestinal tract and preventing their absorption. Activated charcoal is most effective when given shortly after ingestion, ideally within the first hour. It is often used in conjunction with gastric lavage to maximize toxin removal. While it is generally safe, it may interfere with the absorption of other medications, so healthcare providers must carefully manage its use in poisoned patients.
In cases where the specific toxin is known, antidotes may be administered to counteract the mushroom's effects. For example, silibinin is used to treat poisoning from the death cap mushroom (*Amanita phalloides*), which contains amatoxins. These antidotes work by inhibiting the toxin's harmful effects on the liver and other organs. However, not all poisonous mushrooms have specific antidotes, and their availability may vary by region. Identifying the mushroom species as quickly as possible is critical to determine if an antidote can be used.
Supportive care is a cornerstone of treatment for mushroom poisoning, as it addresses the symptoms and complications caused by the toxins. This may include intravenous fluids to prevent dehydration, medications to manage nausea, vomiting, or seizures, and, in severe cases, liver or kidney support. For instance, patients with acute liver failure may require a liver transplant. Continuous monitoring of vital signs, organ function, and electrolyte levels is essential to stabilize the patient and prevent long-term damage. Supportive care is often prolonged, especially in cases of severe poisoning, and may require hospitalization in an intensive care unit.
In summary, the treatment of poisonous mushroom ingestion involves a combination of gastric lavage, activated charcoal, antidotes, and supportive care. The effectiveness of these treatments depends on the timing of intervention, the type of mushroom ingested, and the severity of symptoms. Prompt medical attention is vital, as delays can lead to irreversible organ damage or death. Public education on mushroom identification and the dangers of foraging without expertise can also play a significant role in preventing such incidents.
Do Crickets Eat Mushrooms? Unveiling Their Dietary Habits and Preferences
You may want to see also

Long-Term Effects: Liver damage, kidney failure, neurological issues, and death can occur in severe cases
Consuming poisonous mushrooms can lead to severe long-term health consequences, particularly if the toxins target vital organs. One of the most critical long-term effects is liver damage. Many toxic mushrooms, such as those containing amatoxins (found in the Death Cap and Destroying Angel species), directly attack liver cells. Over time, this can result in hepatitis, liver failure, or even the need for a liver transplant. The liver’s role in detoxifying the body means its impairment can have cascading effects on overall health, making this a life-threatening complication.
Another severe long-term effect is kidney failure, often caused by the same toxins that damage the liver. The kidneys filter waste from the blood, and when exposed to mushroom toxins like orellanine (found in the Deadly Webcap), they can become irreversibly damaged. This may lead to chronic kidney disease, dialysis dependence, or the need for a kidney transplant. Both liver and kidney damage can develop gradually, sometimes becoming apparent only days or weeks after ingestion, making early diagnosis and treatment crucial.
Neurological issues are also a significant long-term concern following the consumption of poisonous mushrooms. Certain species, such as those containing muscarine or ibotenic acid, can cause persistent nerve damage or cognitive impairment. Symptoms may include memory loss, confusion, seizures, or peripheral neuropathy. In severe cases, these neurological effects can be permanent, drastically reducing quality of life and requiring long-term management by specialists.
The most devastating long-term effect of eating a poisonous mushroom is death, which can occur if the toxins overwhelm the body’s ability to recover. Even with medical intervention, the cumulative damage to the liver, kidneys, and nervous system can be fatal. Survival often depends on the speed of treatment, the type of mushroom ingested, and the individual’s overall health. Long-term survivors may face ongoing health challenges, emphasizing the importance of prevention and immediate medical attention if poisoning is suspected.
To mitigate these long-term effects, it is essential to avoid consuming wild mushrooms unless they have been positively identified by an expert. If ingestion occurs, seek emergency medical care immediately, even if symptoms seem mild. Early treatment, such as activated charcoal, gastric lavage, or specific antidotes, can reduce the severity of long-term complications. Awareness and education are key to preventing the potentially irreversible consequences of poisonous mushroom consumption.
Can Cats Safely Eat Mushrooms? Risks and Facts Revealed
You may want to see also
Frequently asked questions
Immediate symptoms can include nausea, vomiting, diarrhea, abdominal pain, and cramps, often appearing within 6 to 24 hours after ingestion. Some toxic mushrooms may also cause sweating, dizziness, or hallucinations.
Yes, consuming certain poisonous mushrooms, such as the Death Cap (*Amanita phalloides*) or Destroying Angel (*Amanita bisporigera*), can be fatal. These mushrooms contain toxins that cause severe liver and kidney damage, leading to organ failure if not treated promptly.
Seek immediate medical attention. Call your local poison control center or go to the emergency room. Bring a sample of the mushroom (if safely possible) for identification. Do not wait for symptoms to appear, as some toxins can cause delayed but severe reactions.
No, not all poisonous mushrooms are deadly. Some cause mild gastrointestinal distress, while others can lead to severe or life-threatening symptoms. The toxicity varies by species, so proper identification is crucial. Always avoid consuming wild mushrooms unless you are absolutely certain they are safe.











































