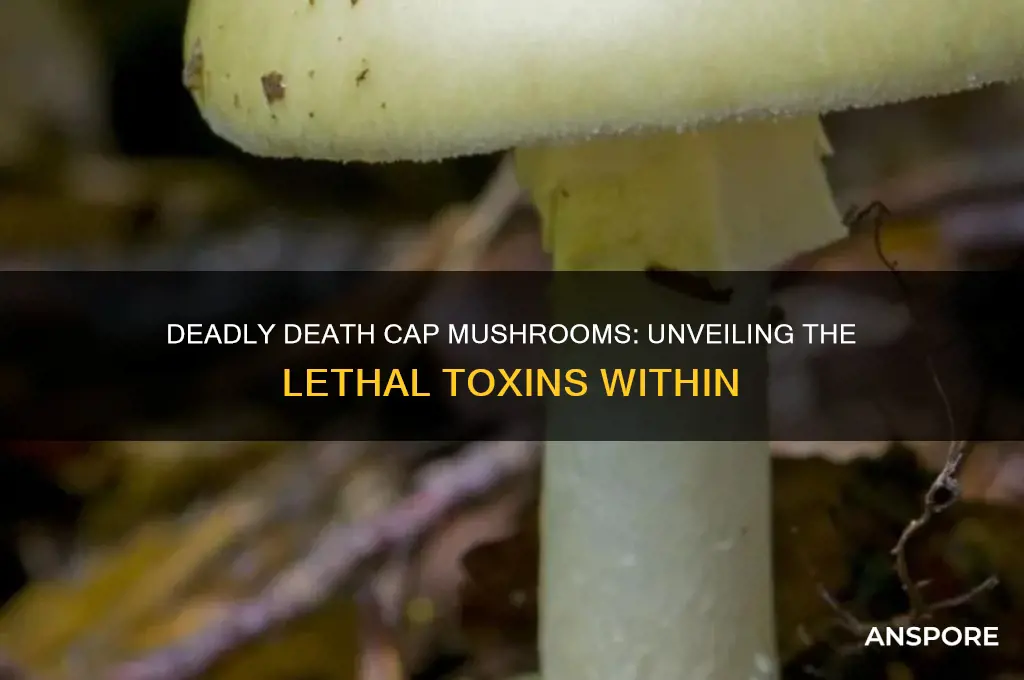
The death cap mushroom, scientifically known as *Amanita phalloides*, is one of the most poisonous fungi in the world, responsible for the majority of fatal mushroom poisonings globally. Its deadliness stems from the presence of potent toxins called amatoxins, which are cyclic octapeptides that cause severe liver and kidney damage by disrupting cellular RNA synthesis. Symptoms of poisoning often appear 6–24 hours after ingestion, starting with gastrointestinal distress, followed by potentially fatal organ failure if left untreated. Despite its innocuous appearance, resembling edible mushrooms, the death cap’s toxins are not destroyed by cooking, drying, or freezing, making it a silent but lethal threat to unsuspecting foragers.
| Characteristics | Values |
|---|---|
| Toxin Type | Amatoxins (primarily α-amanitin, β-amanitin, and γ-amanitin) |
| Toxicity Level | Extremely toxic; as little as 30 grams (or half a mushroom cap) can be fatal to humans |
| Lethal Dose | 0.1 mg/kg of body weight of α-amanitin |
| Symptoms Onset | Delayed, typically 6-24 hours after ingestion (initially asymptomatic) |
| Initial Symptoms | Gastrointestinal (vomiting, diarrhea, abdominal pain, dehydration) |
| Later Symptoms | Liver and kidney failure, jaundice, seizures, coma |
| Fatality Rate | 10-50% without treatment; higher without liver transplant |
| Toxin Mechanism | Inhibits RNA polymerase II, halting protein synthesis and causing cell death, particularly in liver and kidney cells |
| Stability | Toxins are heat-stable and not destroyed by cooking, drying, or freezing |
| Misidentification Risk | Often mistaken for edible mushrooms like paddy straw mushrooms (Volvariella volvacea) or young agarics |
| Geographic Distribution | Widespread in Europe, North America, Australia, and Asia, often found near oak, beech, and pine trees |
| Seasonal Appearance | Typically appears in late summer and autumn |
| Physical Appearance | Olive-green to yellowish-green cap, white gills, volva (cup-like base), and ring on stem |
| Scientific Name | Amanita phalloides |
| Common Names | Death Cap, Striking Amanita |
| Treatment | Gastric decontamination, activated charcoal, silibinin (milk thistle extract), liver transplant in severe cases |
| Prevention | Avoid foraging without expert knowledge; verify mushroom identity with multiple sources |
Explore related products
What You'll Learn
- Alpha-Amanitin Toxin: Primary toxin causing liver, kidney failure, and death within days of ingestion
- Symptom Delay: Symptoms appear 6-24 hours after consumption, delaying treatment and increasing fatality risk
- Misidentification Risk: Resembles edible mushrooms like young puffballs or paddy straw mushrooms, leading to accidental poisoning
- No Known Antidote: No specific cure exists; treatment relies on supportive care and organ transplants in severe cases
- Deadly Dose: As little as half a mushroom can be fatal to an adult due to high toxin concentration

Alpha-Amanitin Toxin: Primary toxin causing liver, kidney failure, and death within days of ingestion
The death cap mushroom, *Amanita phalloides*, owes its lethal reputation to alpha-amanitin, a potent toxin that stealthily destroys vital organs. Unlike many poisons that act immediately, alpha-amanitin operates with a delayed but devastating effect, often leading to symptoms appearing 6–24 hours after ingestion. This delay frequently results in misdiagnosis, as early signs like nausea, vomiting, and diarrhea mimic common food poisoning. By the time the toxin’s true impact becomes apparent, irreversible damage to the liver and kidneys may already be underway.
Alpha-amanitin’s lethality lies in its ability to inhibit RNA polymerase II, a critical enzyme responsible for protein synthesis in cells. Without this enzyme, cells cannot produce essential proteins, leading to rapid cell death, particularly in organs with high metabolic demands like the liver and kidneys. A mere 0.1 mg/kg of body weight—equivalent to half a death cap mushroom for an adult—is sufficient to cause severe poisoning. For children, the dose is even lower, making accidental ingestion particularly dangerous. The toxin’s stability further compounds the risk; it remains active even after cooking, freezing, or drying, rendering common food preparation methods ineffective in neutralizing it.
Treatment for alpha-amanitin poisoning is a race against time. Early administration of activated charcoal can help reduce toxin absorption if given within 1–2 hours of ingestion. Intravenous fluids and medications like silibinin, an antioxidant derived from milk thistle, are used to protect liver cells and support organ function. In severe cases, a liver transplant may be the only lifesaving option, though this is often complicated by the toxin’s simultaneous damage to the kidneys. Survival rates depend heavily on the speed of diagnosis and treatment, with delays significantly increasing mortality.
Prevention remains the most effective strategy. Foraging for wild mushrooms without expert knowledge is a high-risk activity, as death caps closely resemble edible species like the straw mushroom or young puffballs. Key identification features include a greenish cap, white gills, and a skirt-like ring on the stem, but even these can be misleading to the untrained eye. If unsure, the adage “when in doubt, throw it out” is critical. Public education campaigns and the availability of mushroom identification resources can reduce accidental poisonings, particularly in regions where death caps thrive, such as North America, Europe, and Australia.
In summary, alpha-amanitin’s insidious nature—its delayed onset, cellular sabotage, and resistance to destruction—makes it the primary driver of the death cap’s lethality. Awareness of its dangers, coupled with preventive measures and swift medical intervention, are essential to mitigating its deadly impact. Whether you’re a forager, a parent, or a healthcare provider, understanding this toxin’s mechanisms and risks is a matter of life and death.
Crafting Bioluminescent Mushroom Spores: A Step-by-Step Guide to Glowing Seeds
You may want to see also

Symptom Delay: Symptoms appear 6-24 hours after consumption, delaying treatment and increasing fatality risk
The death cap mushroom's insidious nature lies in its ability to deceive both the palate and the body's immediate response. Unlike many toxic substances that trigger rapid symptoms, the death cap's toxins operate on a delayed timer. This symptom delay, ranging from 6 to 24 hours after consumption, is a critical factor in its deadliness. During this asymptomatic period, the mushroom's amatoxins—deadly compounds that target the liver and kidneys—quietly infiltrate the body, causing irreversible damage before the first signs of illness appear.
Consider the scenario: a forager misidentifies a death cap as an edible species, cooks it into a meal, and shares it with family. Hours pass uneventfully, lulling them into a false sense of security. By the time symptoms like nausea, vomiting, and diarrhea emerge, the toxins have already begun dismantling vital organs. This delay not only complicates diagnosis but also reduces the window for effective treatment. For instance, prompt administration of activated charcoal or silibinin (a liver-protecting compound) can mitigate damage, but their efficacy diminishes significantly if administered more than 6 hours post-ingestion.
The delay exacerbates risk across age groups, but children and the elderly are particularly vulnerable. A child’s smaller body mass means even a tiny fragment of a death cap can deliver a lethal dose, while an elderly person’s slower metabolism may prolong toxin absorption, worsening outcomes. Practical precautions include educating foragers to cross-reference mushroom identifications with multiple reliable sources and carrying a portable mushroom guide. In suspected cases, immediately contact a poison control center or emergency services, providing details like the mushroom’s appearance and time of consumption.
Comparatively, other toxic mushrooms like the false morel cause symptoms within hours, allowing for quicker intervention. The death cap’s delayed onset, however, mimics gastroenteritis, leading to misdiagnosis and wasted treatment time. Hospitals often require advanced tests like liver enzyme assays to confirm amatoxin poisoning, further delaying care. This underscores the importance of public awareness: knowing the death cap’s characteristic white gills, skirt-like ring on the stem, and greenish cap can prevent ingestion altogether.
In conclusion, the death cap’s symptom delay is not merely a biological quirk but a strategic weapon in its arsenal. It exploits human complacency and medical limitations, turning hours into a race against time. By understanding this mechanism, foragers, healthcare providers, and the public can better prepare, respond, and ultimately reduce the fatality risk associated with this deceptively innocuous fungus.
Mastering Mushroom Growth in Merge Dragons: Tips and Tricks
You may want to see also

Misidentification Risk: Resembles edible mushrooms like young puffballs or paddy straw mushrooms, leading to accidental poisoning
The death cap mushroom, *Amanita phalloides*, is a master of deception, often mistaken for edible varieties like young puffballs or paddy straw mushrooms. This misidentification is not just a trivial error—it’s a potentially fatal one. The death cap’s smooth, greenish-brown cap and white gills can easily be confused with harmless species, especially by inexperienced foragers. For instance, young puffballs, which are prized for their mild flavor, share a similar rounded shape and pale coloration in their early stages. Similarly, paddy straw mushrooms, a staple in Asian cuisine, have a white, gill-like structure that can resemble the death cap’s underside. This visual mimicry is a silent predator, luring unsuspecting gatherers into a deadly trap.
To illustrate the risk, consider the case of a family in California who, in 2016, mistook death caps for paddy straw mushrooms. Within 48 hours of consumption, all members exhibited severe symptoms of poisoning, including liver failure. Despite medical intervention, one individual succumbed to the toxins. This tragedy underscores the importance of precise identification. Even a small fragment of a death cap—as little as 50 grams for an adult—contains enough alpha-amanitin to cause irreversible organ damage. For children, the lethal dose is even lower, estimated at around 10 grams. These toxins are not neutralized by cooking, drying, or freezing, making misidentification all the more perilous.
Foraging safely requires more than a casual glance. One practical tip is to examine the base of the mushroom. Death caps have a distinctive volva, a cup-like structure at the stem’s base, which is absent in true puffballs and paddy straw mushrooms. Additionally, death caps often emit a faint, unpleasant odor when cut, unlike their edible counterparts. Carrying a reliable field guide or using a mushroom identification app can provide a second layer of verification. However, even these tools are not foolproof; the final safeguard is the principle of "when in doubt, throw it out." No meal is worth the risk of poisoning.
The misidentification risk is compounded by the death cap’s adaptability. It thrives in a variety of environments, from woodlands to urban gardens, often growing near oak, chestnut, and pine trees. Its ability to form symbiotic relationships with tree roots allows it to spread silently, increasing the likelihood of accidental encounters. Foraging during the early stages of mushroom growth, when distinctions are less clear, heightens the danger. Educating oneself about regional mushroom species and their look-alikes is crucial, especially for those new to foraging. Workshops, local mycological societies, and expert-led walks can provide hands-on learning that no book or app can replicate.
Ultimately, the death cap’s resemblance to edible mushrooms is a stark reminder of nature’s duality—beautiful yet treacherous. While the allure of wild harvesting is undeniable, it demands respect and caution. By understanding the specific traits that differentiate the death cap from its benign doppelgängers, foragers can enjoy the bounty of the forest without falling victim to its most cunning inhabitant. The key lies in meticulous observation, continuous learning, and the humility to acknowledge the limits of one’s knowledge. In the world of mushrooms, certainty saves lives.
Crafting a Savory Wildfire Mushroom Crust: A Step-by-Step Guide
You may want to see also
Explore related products

No Known Antidote: No specific cure exists; treatment relies on supportive care and organ transplants in severe cases
The absence of a specific antidote for death cap mushroom poisoning transforms a potentially treatable mistake into a life-threatening crisis. Unlike many toxins, the amatoxins in *Amanita phalloides* are not neutralized by activated charcoal, gastric lavage, or other standard antidotal measures. Once ingested, these toxins bypass the body’s defenses, infiltrating cells and wreaking havoc on vital organs, particularly the liver and kidneys. This biochemical stealth underscores the urgency of early intervention—but even then, the lack of a targeted cure leaves medical professionals with limited options.
Treatment for death cap poisoning hinges on supportive care, a broad term that masks the intensity of the effort required. Patients are often hospitalized immediately, where they receive intravenous fluids to combat dehydration and electrolyte imbalances caused by vomiting and diarrhea. Medications like silibinin (a milk thistle derivative) and N-acetylcysteine may be administered to mitigate liver damage, though their efficacy remains debated. Continuous monitoring of liver and kidney function is critical, as amatoxins can cause rapid deterioration within 24–48 hours. For children, the elderly, or those with pre-existing conditions, even minor delays in treatment can escalate risks exponentially.
In severe cases, the only recourse is an organ transplant, a drastic measure that highlights the toxin’s relentless destructiveness. Amatoxins cause irreversible hepatotoxicity, leading to acute liver failure. Without a transplant, survival rates plummet below 20%. However, transplants are not without complications: immunosuppression required post-transplant can leave patients vulnerable to infections, and the procedure itself carries significant risks. Timing is critical—transplants are most effective when performed before multi-organ failure occurs, but the window is narrow, often less than 72 hours post-ingestion.
This grim reality serves as a stark reminder of the death cap’s lethality. Prevention remains the most effective strategy: avoid foraging without expert guidance, educate children about mushroom dangers, and store wild mushrooms separately from edible varieties to prevent accidental contamination. For those who suspect ingestion, immediate action is paramount. Inducing vomiting (if advised by poison control) and seeking emergency care within 6–12 hours can reduce toxin absorption. Yet, even with swift intervention, the absence of an antidote ensures that every case becomes a race against time, where the stakes are measured in organ function and survival.
Crafting Mario Mushroom Cupcakes: A Fun Baking Adventure Guide
You may want to see also

Deadly Dose: As little as half a mushroom can be fatal to an adult due to high toxin concentration
The death cap mushroom, *Amanita phalloides*, is notorious for its potency, and its toxicity is not to be underestimated. A startling fact underscores its danger: as little as half a mushroom contains enough toxins to be fatal to an adult. This is due to the high concentration of amatoxins, primarily alpha-amanitin, which are deadly even in minuscule amounts. For context, a single mushroom typically weighs around 20 to 50 grams, meaning a dose of just 10 grams—or half a mushroom—can deliver a lethal payload. This makes the death cap one of the most dangerous organisms in the natural world, particularly insidious because its toxins are heat-stable and not destroyed by cooking.
To understand the gravity of this, consider the following: amatoxins target the liver and, to a lesser extent, the kidneys, causing severe damage within 24 to 48 hours of ingestion. Symptoms often begin with gastrointestinal distress—vomiting, diarrhea, and abdominal pain—which can misleadingly subside, giving a false sense of recovery. However, this is followed by a more critical phase where liver failure sets in, often leading to death within 5 to 7 days without medical intervention. Children are even more vulnerable, with a smaller dose required to cause fatal poisoning. For instance, a quarter of a mushroom could be life-threatening for a child, making it crucial for parents and caregivers to educate themselves and their families about mushroom safety.
Practical precautions are essential when foraging or handling wild mushrooms. Always assume any unidentified mushroom is toxic, and never consume one unless it has been positively identified by an expert. Even experienced foragers can mistake the death cap for edible species like the straw mushroom or young puffballs due to its deceptively innocuous appearance. If ingestion is suspected, immediate medical attention is critical. Activated charcoal may be administered to reduce toxin absorption, and in severe cases, a liver transplant might be necessary. Time is of the essence, as delays in treatment significantly increase the risk of fatality.
Comparatively, the death cap’s toxicity dwarfs that of many other poisonous mushrooms. For example, the destroying angel (*Amanita bisporigera*) is also highly toxic, but the death cap’s widespread presence in Europe, North America, and other regions makes it a more frequent cause of poisoning. Its ability to thrive in urban areas, such as parks and gardens, further increases the likelihood of accidental ingestion. This contrasts with other toxic fungi that are less common or confined to specific habitats. The death cap’s combination of accessibility, resemblance to edible species, and extreme toxicity makes it a uniquely dangerous organism.
In conclusion, the death cap’s deadly dose of just half a mushroom highlights the critical importance of awareness and caution. Its high toxin concentration, coupled with delayed and deceptive symptoms, makes it a silent but lethal threat. By understanding its risks and taking proactive measures, individuals can protect themselves and others from this formidable fungus. Remember: when in doubt, throw it out—a moment of hesitation could save a life.
Hearty Mushroom Stew with Beatroot: A Cozy, Flavorful Recipe Guide
You may want to see also
Frequently asked questions
Death cap mushrooms (Amanita phalloides) contain potent toxins called amatoxins, which cause severe liver and kidney damage, often leading to organ failure and death if ingested.
Symptoms typically appear 6–24 hours after ingestion, starting with gastrointestinal issues like nausea, vomiting, and diarrhea, followed by more severe liver and kidney damage.
No, cooking, drying, or boiling does not destroy the amatoxins in death cap mushrooms. They remain deadly even after preparation.
Death caps can resemble edible mushrooms, but they have distinctive features like a greenish-yellow cap, white gills, and a bulbous base with a cup-like volva. However, identification should only be done by experts.
There is no specific antidote, but treatment includes supportive care, activated charcoal, and, in severe cases, liver transplantation. Early medical intervention is critical for survival.