The question of whether an X-ray can detect spores in the lungs is a common concern, particularly for individuals exposed to fungal or bacterial environments. While X-rays are a valuable tool for visualizing lung tissue and identifying abnormalities like infections or tumors, they are not capable of directly detecting microscopic spores. Spores are typically too small to be visible on standard X-ray imaging, which focuses on larger structures and density changes. However, if spores have caused an infection or inflammation in the lungs, an X-ray may reveal secondary signs such as infiltrates, nodules, or cavities, prompting further diagnostic tests like CT scans, sputum cultures, or biopsies to confirm the presence of spores.
| Characteristics | Values |
|---|---|
| Can X-rays detect spores in lungs? | No, standard X-rays cannot directly visualize individual spores. |
| Reason for limitation | Spores are microscopic and lack sufficient density to be visible on X-rays. |
| What X-rays can show | X-rays may detect lung abnormalities caused by spore-related infections (e.g., fungal pneumonia, aspergillosis), such as infiltrates, nodules, or cavities. |
| Alternative imaging methods | CT scans (high-resolution) or MRI may provide better visualization of lung tissue changes caused by spores. |
| Direct spore detection | Requires laboratory tests (e.g., sputum culture, biopsy, or PCR) for confirmation. |
| Clinical relevance | X-rays are useful for diagnosing spore-related lung diseases but not for identifying spores themselves. |
| Latest advancements | No recent breakthroughs in using X-rays to directly detect spores; focus remains on detecting secondary lung damage. |
Explore related products
What You'll Learn

X-ray limitations for detecting spores
X-rays, a cornerstone of medical imaging, excel at visualizing dense structures like bones and certain soft tissues. However, their effectiveness in detecting spores within the lungs is severely limited. Spores, being microscopic and often less dense than surrounding lung tissue, lack the contrast necessary to be discernible on a standard X-ray image. This fundamental limitation arises from the physics of X-ray imaging, where denser materials absorb more radiation, creating darker areas on the film or digital image. Spores, with their lightweight composition, simply do not create enough contrast to stand out.
For instance, consider *Aspergillus* spores, a common cause of fungal infections in immunocompromised individuals. These spores, measuring around 2-3 micrometers in diameter, are virtually invisible on a chest X-ray, even in cases of severe pulmonary aspergillosis. This highlights the need for alternative imaging modalities when suspecting spore-related lung infections.
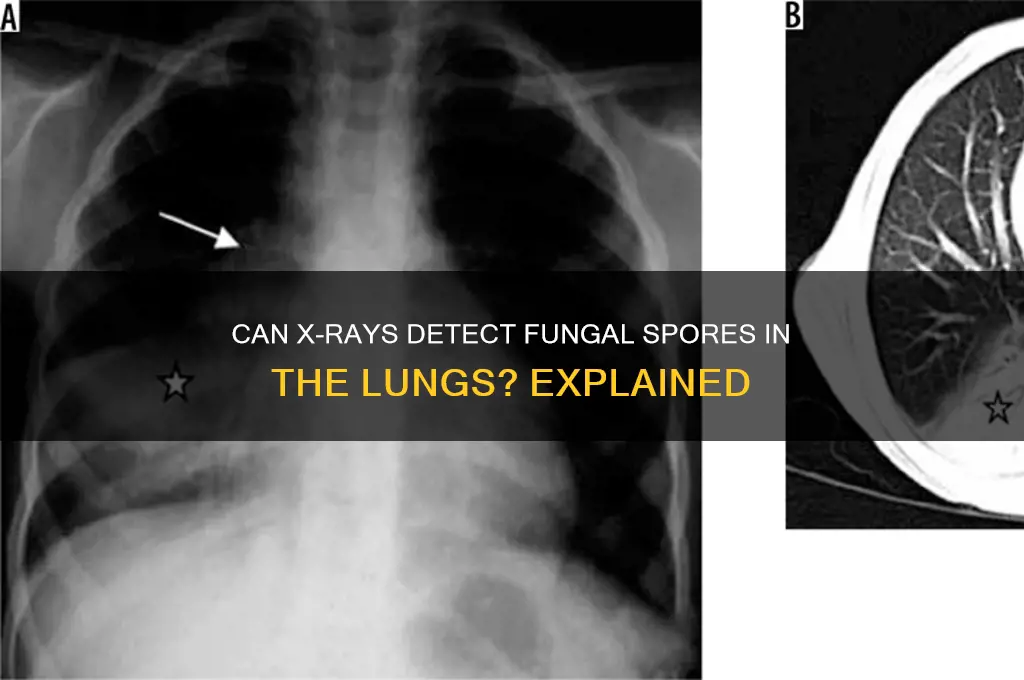
While X-rays may not directly visualize spores, they can provide indirect clues to their presence. In cases of fungal pneumonia, for example, X-rays might reveal infiltrates, cavities, or nodules, which are inflammatory responses to the spores rather than the spores themselves. These findings, however, are non-specific and could indicate various other lung conditions. Therefore, relying solely on X-ray findings for diagnosis can lead to misdiagnosis or delayed treatment.
A more accurate approach involves combining X-ray findings with clinical symptoms, patient history, and other diagnostic tools like CT scans, sputum cultures, or serological tests. CT scans, with their higher resolution and ability to differentiate tissue densities, can sometimes detect larger spore aggregations or the characteristic patterns of certain fungal infections.
It's crucial to understand that X-rays are not a definitive tool for diagnosing spore-related lung conditions. Their primary role lies in ruling out other potential causes of respiratory symptoms and providing a baseline for monitoring disease progression. For instance, a normal chest X-ray in a patient with suspected fungal pneumonia doesn't exclude the diagnosis but rather prompts further investigation with more sensitive methods. This underscores the importance of a comprehensive diagnostic approach that goes beyond the limitations of a single imaging modality.
Is Spore Available on Xbox? Exploring Compatibility and Gaming Options
You may want to see also

Alternative imaging methods for spores
While X-rays are a common diagnostic tool, their ability to detect spores in the lungs is limited. Spores, being microscopic, often lack the density to produce a visible contrast on X-ray images. This limitation necessitates the exploration of alternative imaging methods that offer greater sensitivity and specificity for spore detection.
High-Resolution Computed Tomography (HRCT): This advanced form of CT scanning utilizes thinner slices and higher resolution, enabling the detection of subtle lung abnormalities. HRCT can identify characteristic patterns associated with spore-related infections, such as nodules, cavities, and ground-glass opacities. For instance, in cases of pulmonary aspergillosis, HRCT may reveal halo signs or air crescent signs, indicative of fungal invasion.
Magnetic Resonance Imaging (MRI): MRI employs strong magnetic fields and radio waves to generate detailed images of soft tissues. While less commonly used for lung imaging due to motion artifacts from breathing, MRI can be valuable in specific scenarios. For example, MRI with gadolinium contrast enhancement can help differentiate between spore-induced lesions and other pulmonary conditions, particularly in immunocompromised patients.
Positron Emission Tomography (PET): PET scanning involves injecting a radioactive tracer, typically fluorodeoxyglucose (FDG), which is taken up by metabolically active cells. This technique can identify areas of increased metabolic activity, potentially indicating spore proliferation. However, PET is often used in conjunction with CT (PET/CT) to provide both anatomical and functional information, enhancing diagnostic accuracy.
Optical Coherence Tomography (OCT): Emerging as a promising tool for pulmonary imaging, OCT uses light waves to capture high-resolution cross-sectional images of lung tissue. Its ability to visualize airway microstructures and detect early signs of infection makes it a potential candidate for spore detection, particularly in research settings. However, further studies are needed to establish its clinical utility in this context.
Considerations and Future Directions: Each alternative imaging method has its strengths and limitations. HRCT remains the mainstay for evaluating pulmonary spore infections, while MRI and PET offer complementary information in specific cases. OCT, though experimental, holds promise for early detection and monitoring. Ongoing research aims to refine these techniques, improve their accessibility, and integrate them into clinical protocols for more accurate and timely diagnosis of spore-related lung conditions.
Do Angiosperms Produce Spores? Unveiling the Truth About Seed Plants
You may want to see also

Symptoms of spore-related lung infections
Spores, when inhaled, can lead to lung infections that manifest with distinct symptoms, often depending on the type of spore and the individual’s immune response. Common culprits include fungal spores like *Aspergillus* or bacterial spores such as *Bacillus anthracis*. Early symptoms frequently mimic those of a respiratory infection, including persistent cough, chest pain, and shortness of breath. These symptoms may be accompanied by systemic signs like fever, fatigue, and unexplained weight loss, particularly in immunocompromised individuals. Recognizing these early indicators is crucial, as spore-related infections can progress rapidly if left untreated.
In more severe cases, spore-related lung infections can lead to conditions like allergic bronchopulmonary aspergillosis (ABPA) or invasive pulmonary aspergillosis. ABPA often presents with wheezing, coughing, and the production of brown-flecked mucus, while invasive aspergillosis may cause hemoptysis (coughing up blood) and severe respiratory distress. Bacterial spore infections, such as inhalation anthrax, can result in acute symptoms like high fever, severe chest pain, and respiratory failure within days of exposure. These advanced symptoms require immediate medical attention, as they can be life-threatening.
Diagnosing spore-related lung infections involves a combination of clinical evaluation, imaging, and laboratory tests. While an X-ray may not directly show spores, it can reveal characteristic patterns such as nodules, cavities, or infiltrates in the lungs, which suggest fungal or bacterial growth. For instance, *Aspergillus* infections often appear as a "halo sign" on imaging, where a dense, round lesion is surrounded by a less dense area. However, definitive diagnosis typically requires sputum cultures, blood tests, or biopsy to identify the specific pathogen.
Prevention and early intervention are key to managing spore-related lung infections. Immunocompromised individuals, such as those with HIV, cancer, or organ transplants, should take precautions to avoid environments with high spore concentrations, like construction sites or areas with visible mold. For those exposed to bacterial spores, such as anthrax, prophylactic antibiotics like ciprofloxacin or doxycycline (typically 500 mg twice daily for 60 days) may be prescribed. Regular monitoring and prompt treatment can significantly improve outcomes and reduce the risk of complications.
In summary, spore-related lung infections present with a range of symptoms, from mild respiratory discomfort to severe, life-threatening conditions. While X-rays cannot detect spores directly, they play a vital role in identifying associated lung abnormalities. Early recognition of symptoms, combined with appropriate diagnostic and preventive measures, is essential for effective management. Understanding these specifics empowers individuals and healthcare providers to act swiftly, potentially preventing long-term damage or fatal outcomes.
Are Anthrax Spores Identical? Unraveling the Genetic Similarities and Differences
You may want to see also
Explore related products

Common spore-causing lung conditions
Spores, the resilient reproductive units of certain fungi and bacteria, can infiltrate the lungs and trigger a range of conditions, some of which may be visible on an X-ray. While X-rays are not specifically designed to detect spores, they can reveal the lung damage or abnormalities caused by spore-related infections. Here’s a focused guide on common spore-causing lung conditions and how they might appear in imaging.
Histoplasmosis, often called "cave disease," is caused by inhaling spores of the fungus *Histoplasma capsulatum*. This condition is prevalent in areas with bird or bat droppings, such as caves or old buildings. On an X-ray, acute histoplasmosis may show small nodules or a diffuse infiltrate in the lungs, resembling pneumonia. Chronic cases can lead to fibrotic changes or cavities, particularly in immunocompromised individuals. Treatment typically involves antifungal medications like itraconazole for mild to moderate cases, with amphotericin B reserved for severe infections.
Another spore-related condition is aspergillosis, caused by *Aspergillus* fungi commonly found in soil and decaying vegetation. Invasive aspergillosis, which affects immunocompromised patients, can manifest as dense, wedge-shaped opacities (Halsey plaques) on X-rays or CT scans. Allergic bronchopulmonary aspergillosis (ABPA), more common in asthmatics, may show central bronchiectasis or transient pulmonary opacities. Treatment varies: corticosteroids for ABPA, and voriconazole or isavuconazole for invasive cases.
Coccidioidomycosis, or Valley Fever, results from inhaling spores of *Coccidioides* fungi in arid regions like the southwestern U.S. X-rays often reveal nodules, cavities, or diffuse infiltrates, mimicking tuberculosis. Most cases resolve without treatment, but severe or disseminated infections require antifungals like fluconazole. Interestingly, a positive coccidioidin skin test can confirm exposure, though it’s not a standard diagnostic tool.
Lastly, blastomycosis, caused by *Blastomyces dermatitidis*, is found near waterways and wooded areas. X-rays may show acute pneumonia-like infiltrates or chronic cavitary lesions resembling tuberculosis. Treatment includes itraconazole for mild cases and amphotericin B for severe infections. Early diagnosis is crucial, as symptoms like fever, cough, and weight loss can mimic other respiratory conditions.
While X-rays cannot directly identify spores, they are invaluable in diagnosing the lung damage caused by these spore-related conditions. Recognizing patterns—such as nodules, cavities, or infiltrates—can guide further testing, including fungal cultures or serology. For high-risk individuals, such as those with HIV or organ transplants, proactive monitoring and prompt treatment are essential to prevent complications. Always consult a healthcare provider for accurate diagnosis and management.
Does Spore Effectively Work on Grass-Type Pokémon? A Detailed Analysis
You may want to see also

When to seek medical evaluation
Spores in the lungs often remain undetected until symptoms escalate, making timely medical evaluation critical. Persistent or worsening respiratory symptoms like chronic cough, unexplained fever, or difficulty breathing warrant immediate attention, especially if you’ve been exposed to moldy environments or contaminated materials. While chest X-rays may not directly visualize spores, they can reveal secondary infections or abnormalities like fungal masses or cavities, which are red flags for spore-related conditions such as aspergillosis or histoplasmosis. If symptoms coincide with occupational or environmental risk factors—such as working in agriculture, construction, or water-damaged buildings—seek evaluation promptly to rule out spore-induced complications.
Analyzing the urgency, individuals with weakened immune systems (e.g., HIV, cancer, or organ transplant recipients) should prioritize medical assessment at the first sign of respiratory distress. Spores like *Aspergillus* or *Cryptococcus* can rapidly progress to severe infections in immunocompromised patients, often requiring antifungal therapy like voriconazole (4 mg/kg every 12 hours) or amphotericin B (0.7–1 mg/kg/day). Early detection through imaging and lab tests, such as sputum cultures or serum antigen assays, can prevent life-threatening conditions like invasive pulmonary aspergillosis. Delaying care in these cases increases mortality risk, emphasizing the need for proactive monitoring.
For otherwise healthy individuals, the decision to seek evaluation hinges on symptom persistence and severity. A cough lasting over three weeks, unexplained weight loss, or hemoptysis (coughing up blood) should prompt a visit to a healthcare provider. While chest X-rays may appear normal in early stages, a high-resolution CT scan can detect subtle changes like ground-glass opacities or nodules, guiding further diagnostic steps. If exposure to bird or bat droppings is suspected, histoplasmosis testing (e.g., urine antigen or blood tests) becomes essential, as this fungal infection often mimics tuberculosis or pneumonia.
Comparatively, children and older adults face higher risks due to developing or weakened immune systems. Parents should monitor for recurrent respiratory infections, wheezing, or failure to thrive in children, as these could indicate environmental spore exposure. In seniors, symptoms like fatigue, chest pain, or reduced lung function should not be dismissed as age-related decline. Pediatricians and geriatric specialists often recommend environmental assessments alongside medical evaluations to identify and mitigate spore sources, such as mold in schools or homes.
Practically, if you suspect spore exposure, document symptoms, potential sources (e.g., workplace, home), and recent travel to endemic areas like the Ohio or Mississippi River valleys for histoplasmosis. Bring this information to your appointment to aid diagnosis. While X-rays alone may not confirm spores, they serve as a crucial first step in identifying complications. Follow-up with a pulmonologist or infectious disease specialist may be necessary for definitive diagnosis and treatment, ensuring spores don’t silently compromise lung health.
Rhizopus Spores: Understanding Their Haploid or Diploid Nature Explained
You may want to see also
Frequently asked questions
An X-ray is not capable of detecting spores in the lungs. It can show signs of infection or tissue damage caused by spores, but it cannot identify the spores themselves.
If spores are causing an infection, an X-ray may reveal abnormalities like inflammation, fluid buildup, or lesions in the lung tissue, but it cannot directly visualize the spores.
Yes, advanced imaging techniques like CT scans or MRI may provide more detailed views of lung tissue, but even these methods cannot specifically identify spores. Laboratory tests or biopsies are typically needed for confirmation.






























