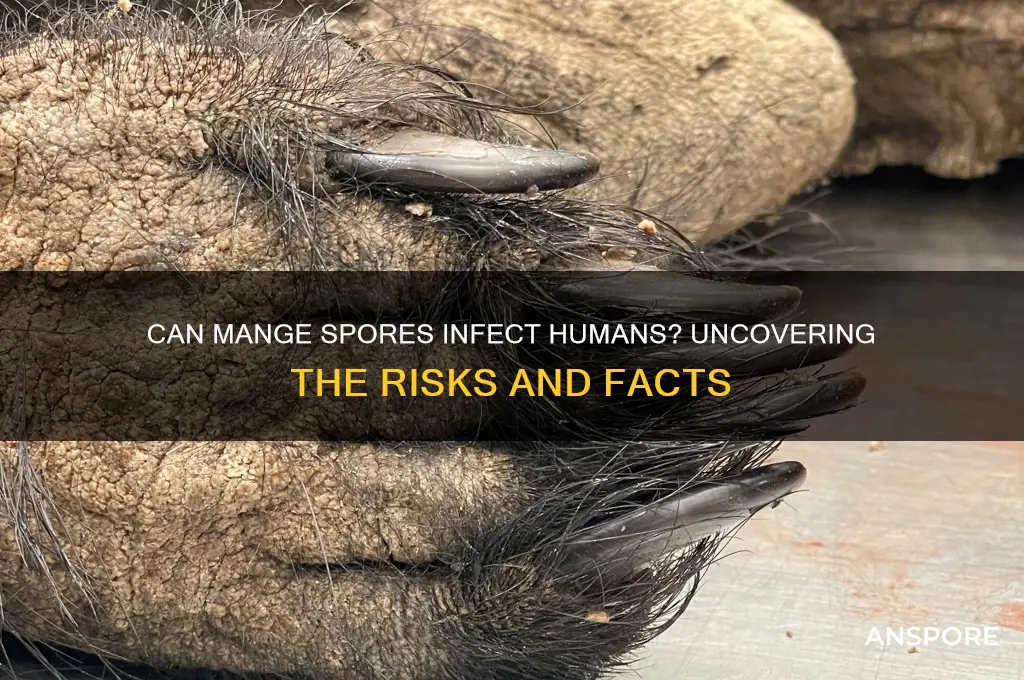
Mange, a skin disease primarily caused by parasitic mites, is commonly associated with animals such as dogs, cats, and wildlife, but questions often arise about whether the spores or mites responsible for mange can affect humans. While mange mites are species-specific, meaning they typically infest only their primary host, certain types, like *Sarcoptes scabiei*, can cause a condition known as scabies in humans. However, the spores themselves are not the primary concern; rather, it is the mites that can lead to skin irritation, itching, and infection in humans if they come into contact with an infested animal. Understanding the differences between mange in animals and its potential impact on humans is crucial for proper prevention and treatment.
Explore related products
What You'll Learn

Can mange spores infect humans directly?
Mange, caused by parasitic mites, primarily affects animals, but the question of whether mange spores can directly infect humans is a nuanced one. Mange mites, such as *Sarcoptes scabiei*, are known to burrow into the skin of their hosts, causing intense itching and skin lesions. While these mites are highly adapted to their specific animal hosts, certain species, like *Sarcoptes scabiei var. hominis*, can infect humans, leading to a condition called scabies. However, this is not a case of spores infecting humans; rather, it involves direct transmission of live mites through close physical contact.
To clarify, mange does not produce spores. Spores are typically associated with fungi or bacteria, not parasitic mites. Mange mites reproduce through eggs, which hatch into larvae and eventually mature into adults. This distinction is crucial because it eliminates the possibility of spore-based infection in humans. Instead, human infection occurs when live mites migrate from an infested animal or person to a new host, often during prolonged skin-to-skin contact. For example, pet owners handling dogs with sarcoptic mange (*Sarcoptes scabiei var. canis*) may experience temporary skin irritation, but this is usually a short-lived reaction to the mites, not a full-blown infection.
From a practical standpoint, preventing direct mite transmission is key. If you suspect your pet has mange, avoid close contact until they are treated by a veterinarian. Wear protective gloves when handling infested animals, and wash your hands thoroughly afterward. For humans, scabies is treatable with prescription creams like permethrin or ivermectin, which kill the mites and their eggs. It’s also essential to clean and vacuum living spaces to remove any mites that may have fallen off the host, as they can survive off the host for a few days.
Comparatively, while mange mites pose a minor risk to humans, other zoonotic parasites, like hookworms or ringworm, are more likely to cause persistent infections. Ringworm, for instance, is a fungal infection that produces spores, which can easily spread to humans through contact with contaminated surfaces or animals. Mange, however, relies on live mites for transmission, making it less of a direct threat to human health. Understanding this difference helps in adopting appropriate preventive measures.
In conclusion, mange spores cannot infect humans directly because mange mites do not produce spores. The risk to humans lies in direct contact with live mites, which can cause temporary skin irritation but rarely leads to full-blown scabies unless the specific human variant of the mite is involved. By focusing on hygiene, protective measures, and prompt treatment of infested animals, the risk of mite transmission can be effectively minimized.
Does Milky Spore Kill All Grubs? A Comprehensive Guide
You may want to see also

Symptoms of potential mange spore exposure in humans
Mange, primarily a condition affecting animals, is caused by microscopic mites that burrow into the skin. While the mites themselves are species-specific, the spores or debris from their presence can become airborne, raising questions about human exposure. Although rare, humans can experience symptoms from contact with mange spores, particularly in environments heavily infested with infected animals. Recognizing these symptoms early is crucial for timely intervention.
Initial Symptoms and Identification
Exposure to mange spores in humans often manifests as mild to moderate skin irritation. This includes itching, redness, and small bumps or rashes, typically appearing within 24 to 48 hours of contact. Unlike animal mange, human symptoms are usually localized to the area of exposure, such as the hands, arms, or face. For instance, handling an infected dog without protective gloves may result in a rash on the hands. These symptoms are often mistaken for allergies or insect bites, making it essential to consider recent contact with potentially infested animals.
Progression and Severity
If exposure is prolonged or the spore concentration is high, symptoms can escalate. Intense itching may lead to scratching, causing skin breaks and secondary bacterial infections. In rare cases, individuals with compromised immune systems or prolonged exposure might develop more severe reactions, such as widespread dermatitis or respiratory irritation from inhaling spore-laden dust. Children and the elderly are particularly vulnerable due to their thinner skin and weaker immune responses. Monitoring symptoms closely and avoiding further exposure are critical steps in preventing complications.
Practical Tips for Prevention and Management
To minimize the risk of mange spore exposure, wear protective clothing and gloves when handling animals suspected of having mange. After contact, wash hands thoroughly with soap and water. If symptoms appear, over-the-counter antihistamines or topical corticosteroids can alleviate itching and inflammation. For persistent or severe symptoms, consult a healthcare provider, who may prescribe stronger treatments. Regularly cleaning and disinfecting areas where infested animals reside can also reduce spore presence, safeguarding both human and animal health.
Comparative Perspective
While mange spores are not directly infectious to humans, their impact is comparable to other environmental irritants like mold or pollen. The body’s reaction is often an immune response to foreign particles rather than an infection. Unlike scabies, which is caused by a human-specific mite, mange-related symptoms in humans are transient and resolve with proper care. Understanding this distinction helps in managing expectations and responses, ensuring that minor irritations do not escalate into unnecessary panic or medical intervention.
Does Rain Increase Mold Spores? Understanding the Link Between Rain and Mold
You may want to see also

Differences between animal and human mange spores
Mange, caused by microscopic mites, manifests differently in animals and humans, primarily due to species-specific mite variants. Sarcoptes scabiei is the notorious culprit behind scabies in humans, burrowing into the skin and triggering intense itching. In animals, Sarcoptes scabiei also exists, but distinct subspecies like *S. scabiei var. canis* (dogs) and *S. scabiei var. suis* (pigs) are more common. While cross-species transmission is possible, these variants are less likely to establish long-term infestations in humans due to evolutionary adaptations. For instance, canine scabies mites may cause temporary skin irritation in humans but rarely lead to full-blown scabies.
The lifecycle and behavior of mange mites further highlight differences. Human scabies mites have a 2-4 week lifecycle, with females tunneling into the skin to lay eggs. Animal mites, such as those affecting dogs or cattle, often have shorter lifecycles and may inhabit superficial skin layers or hair follicles. This distinction influences treatment approaches. Human scabies requires systemic medications like permethrin or ivermectin, while animal mange treatments often involve topical solutions or dips containing amitraz or lime sulfur. Dosage and application methods vary significantly; for example, ivermectin for dogs is administered orally at 0.2 mg/kg, whereas humans receive a single oral dose of 200 mcg/kg under medical supervision.
Environmental persistence of mange spores is another critical difference. Animal mange mites, particularly those causing sarcoptic mange in wildlife like foxes, can survive off-host for up to 3 weeks in cool, humid conditions. In contrast, human scabies mites rarely survive more than 48 hours outside the skin, limiting environmental transmission. This makes animal mange a greater public health concern in rural or agricultural settings, where humans may inadvertently come into contact with infested bedding, soil, or equipment. Practical tips include wearing gloves when handling potentially infested animals and washing hands thoroughly afterward.
Finally, the clinical presentation of mange differs markedly between species. Humans exhibit symptoms like severe itching, rash, and burrows (thin, wavy lines on the skin), often localized to hands, wrists, and genital areas. In animals, symptoms vary widely: dogs may develop hair loss, crusting, and intense itching, while cattle show thickened skin and lice-like lesions. Misdiagnosis can occur when humans contract animal mange, as symptoms may mimic allergic reactions or eczema. If exposure to infested animals is suspected, seek medical attention promptly, especially if symptoms include persistent itching or unusual skin lesions. Understanding these differences ensures appropriate treatment and prevents unnecessary panic or mismanagement.
Can Breloom Learn Spore? Move Relearner Guide for Pokémon Trainers
You may want to see also
Explore related products

How mange spores spread to humans from animals
Mange, caused by microscopic mites, primarily affects animals but can occasionally spread to humans, leading to a condition known as sarcoptic mange or scabies. The mites responsible for mange do not produce spores; instead, they are living parasites that burrow into the skin, causing intense itching and irritation. However, the question of spore transmission arises from a misunderstanding, as spores are typically associated with fungi or bacteria, not mites. Despite this, the spread of mange mites from animals to humans is a genuine concern, particularly in close-contact scenarios.
Transmission Pathways: Direct Contact
The most common way mange mites spread from animals to humans is through direct, prolonged contact with an infested animal. Dogs, foxes, and other wildlife are frequent carriers of sarcoptic mange mites. When a human touches or handles an infected animal, the mites can quickly crawl onto their skin, seeking warmth and a new host. This risk is highest in situations like petting stray animals, caring for infected pets without protective gear, or handling wildlife. For example, hunters or veterinarians may be at increased risk due to their exposure to potentially infested animals.
Indirect Transmission: Environmental Contamination
While less common, indirect transmission can occur when mites survive off a host for short periods. Mange mites can live in bedding, furniture, or soil for up to 36 hours, depending on environmental conditions. If a human comes into contact with these contaminated surfaces and then touches their face or skin, mites may transfer. This is particularly relevant in households with infested pets, where shared living spaces increase the likelihood of exposure. Regular cleaning and disinfection of pet areas can mitigate this risk, especially using acaricides (mite-killing agents) recommended by veterinarians.
Prevention and Practical Tips
To minimize the risk of mange transmission, avoid direct contact with stray or wild animals, especially those showing signs of mange (e.g., hair loss, redness, or excessive scratching). When handling pets suspected of having mange, wear gloves and long sleeves. Wash hands thoroughly after contact and launder clothing in hot water. For households with infected pets, isolate the animal and treat it under veterinary guidance. Additionally, vacuum and disinfect living areas frequently to eliminate any mites that may have fallen off the host.
Human Infection: Symptoms and Treatment
When humans contract mange, symptoms typically appear within 2–6 weeks after exposure. These include severe itching, especially at night, and a rash with small red bumps or burrows. Unlike animal mange, human scabies is usually self-limiting and treatable with topical medications like permethrin or ivermectin, prescribed by a healthcare provider. Early detection and treatment are crucial to prevent secondary infections from scratching. While uncomfortable, human scabies is rarely life-threatening and does not lead to long-term complications with proper care.
In summary, while mange mites do not produce spores, their spread from animals to humans is a real but preventable risk. Understanding transmission pathways and adopting practical precautions can effectively protect both humans and pets from this parasitic infestation.
Playing Spore Without Origin: Is It Possible? A Guide
You may want to see also

Prevention methods for human mange spore exposure
Mange, primarily a veterinary concern, rarely affects humans directly, but understanding spore exposure prevention is crucial for at-risk groups. While mange itself is caused by mites, not spores, the broader context of zoonotic transmission and environmental persistence of pathogens informs preventive strategies. For individuals in close contact with infected animals—veterinarians, farmers, or pet owners—minimizing skin-to-skin contact is paramount. Wear protective gloves, long sleeves, and pants when handling potentially infected animals, and avoid touching your face until after thorough handwashing with soap and water for at least 20 seconds.
Environmental decontamination is another critical step, as mites and their byproducts can survive in bedding, carpets, or soil. Wash contaminated fabrics in hot water (130°F or 54°C) and dry on high heat for at least 30 minutes to kill mites. For non-washable surfaces, use acaricides like permethrin or ivermectin, following label instructions for concentration and application. Vacuum frequently, disposing of the bag immediately to prevent recontamination. In agricultural settings, quarantine infected animals and disinfect their living areas with approved solutions, ensuring proper ventilation during application.
Personal hygiene extends to pet care routines. After treating an infected pet, bathe them with a veterinarian-recommended shampoo, such as those containing benzoyl peroxide or chlorhexidine, to reduce mite populations. Avoid sharing personal items like towels or bedding with pets, and regularly clean their grooming tools. For high-risk individuals, consider prophylactic measures: consult a healthcare provider about ivermectin use, though its efficacy in preventing human exposure is not well-established and should only be used under medical supervision.
Comparatively, human prevention mirrors veterinary protocols but emphasizes behavioral changes. Unlike animals, humans benefit from awareness and proactive measures. For instance, educating children about avoiding stray animals and teaching them proper hand hygiene after petting animals reduces exposure risk. In endemic areas, community-wide efforts, such as pet treatment campaigns and public health education, can lower transmission rates. While mange spores are not a direct threat, these methods address the broader risk of mite-borne illnesses, ensuring a safer environment for both humans and animals.
Exploring Galactic Adventures: Can You Purchase It Without Spore?
You may want to see also
Frequently asked questions
Mange spores, which are caused by mites like *Sarcoptes scabiei*, can infest humans, but the resulting condition is called scabies, not mange. Scabies in humans is caused by a different subspecies of the mite.
Mange mites from animals can temporarily infest humans, causing itching and skin irritation, but they cannot complete their life cycle on humans and will eventually die off.
While touching an animal with mange may cause temporary skin irritation or allergic reactions in humans, it does not lead to a persistent infection or serious illness.
Mange spores in the environment are not typically a significant health risk to humans, as they are adapted to animal hosts and cannot survive long outside their host.
Humans cannot develop mange from infected animals, but they may experience temporary skin irritation or scabies-like symptoms from exposure to animal mites.