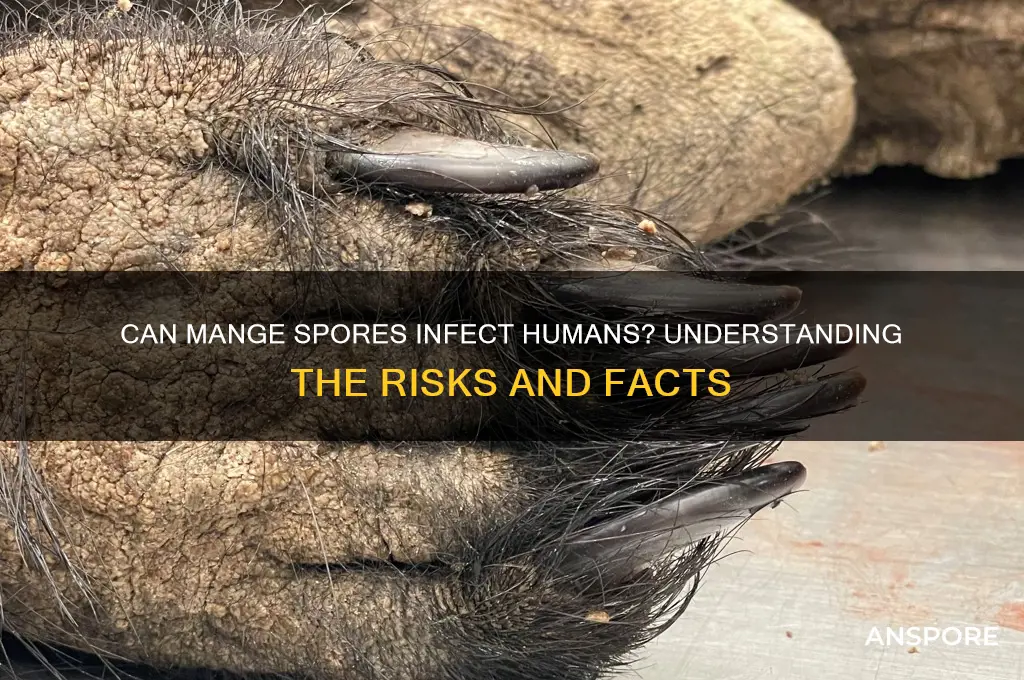
Mange, a skin disease caused by parasitic mites, primarily affects animals such as dogs, cats, and wildlife, but there is growing interest in whether the mites responsible for mange can also infect humans. While mange mites are species-specific, meaning they typically target a particular host, certain types, like *Sarcoptes scabiei*, can occasionally infest humans, leading to a condition known as scabies. However, the question of whether mange spores, or more accurately, mite eggs and fecal matter, can directly make humans sick remains a topic of concern. Although direct transmission from animals to humans is rare, prolonged exposure to infested animals or contaminated environments may pose risks, particularly for individuals with weakened immune systems. Understanding the potential for cross-species transmission and the health implications for humans is essential for both pet owners and public health professionals.
| Characteristics | Values |
|---|---|
| Can mange spores make humans sick? | No, mange spores (from sarcoptic mange mites) do not directly infect humans. |
| Mange Cause | Caused by parasitic mites (e.g., Sarcoptes scabiei) that burrow into skin. |
| Human Risk | Humans may experience temporary skin irritation (e.g., itching, redness) from contact with infected animals, but it is not mange. |
| Condition in Humans | Similar symptoms in humans are called scabies, caused by a related mite (Sarcoptes scabiei var. hominis). |
| Transmission | Mange mites from animals cannot complete their life cycle on humans. |
| Prevention | Avoid contact with infected animals; treat pets promptly if diagnosed. |
| Treatment for Animals | Topical medications, oral treatments, or injections prescribed by vets. |
| Treatment for Humans (Scabies) | Topical scabicidal creams (e.g., permethrin) prescribed by healthcare providers. |
| Zoonotic Potential | Low; human scabies is typically transmitted human-to-human, not from animals. |
| Affected Animals | Dogs, cats, foxes, wildlife (e.g., foxes, coyotes). |
| Symptoms in Animals | Intense itching, hair loss, skin lesions, crusting, and secondary infections. |
Explore related products
What You'll Learn

Sporotrichosis transmission risks
Mange spores, specifically those associated with sporotrichosis, pose a nuanced risk to human health. Unlike common misconceptions, sporotrichosis is not caused by mange mites but by the fungus *Sporothrix schenckii*. However, the confusion often arises because both conditions can affect animals, particularly cats, which can then transmit the fungus to humans. Understanding the transmission risks of sporotrichosis is crucial for prevention, especially for those in close contact with infected animals or contaminated environments.
Transmission of sporotrichosis primarily occurs through traumatic inoculation of the fungus into the skin. This typically happens when the skin is punctured by contaminated materials, such as thorns, soil, or even the teeth or claws of infected animals. For instance, gardeners, farmers, and veterinarians are at higher risk due to their exposure to soil and plants, while cat owners may contract the disease through scratches or bites from infected felines. The fungus thrives in organic matter, making outdoor activities in endemic areas a potential risk factor. To minimize exposure, wearing protective gloves and long sleeves when handling soil or plants is essential, particularly in regions where sporotrichosis is prevalent.
While sporotrichosis is not contagious between humans, the role of animals, especially cats, in its transmission cannot be overstated. Cats can develop severe, disseminated forms of the disease, shedding the fungus in their nasal and oral secretions. Humans can contract the infection through direct contact with these secretions or by inhaling fungal spores, though this is less common. Pet owners should avoid touching open wounds or mucous membranes after handling infected animals and seek veterinary care promptly if their cat shows symptoms like skin lesions or respiratory distress. Quarantining infected pets and maintaining good hygiene can significantly reduce transmission risks.
Interestingly, the severity of sporotrichosis in humans varies widely, influenced by factors such as the individual’s immune status and the fungal strain involved. Immunocompromised individuals, such as those with HIV/AIDS or undergoing chemotherapy, are at higher risk of developing severe, systemic infections. In contrast, healthy individuals typically experience localized skin infections, which, while painful and chronic, are rarely life-threatening. Early diagnosis and treatment, often involving antifungal medications like itraconazole or potassium iodide, are critical for managing the disease effectively. Awareness of these risks and proactive measures can help prevent sporotrichosis and mitigate its impact on human health.
Are Spores an Aerosol? Exploring the Science Behind Airborne Particles
You may want to see also

Symptoms in humans
Mange, primarily a condition affecting animals, is caused by microscopic mites burrowing into the skin. While these mites typically target specific host species, certain types, like *Sarcoptes scabiei*, can occasionally infest humans, leading to a condition known as scabies. This raises the question: can mange spores, or rather, mites, make humans sick? The answer lies in understanding the symptoms these mites induce in humans, which, though not life-threatening, can be intensely uncomfortable and require prompt treatment.
Identifying the Symptoms: A Practical Guide
The hallmark of scabies in humans is an unrelenting itch, particularly severe at night. This itch results from the body’s allergic reaction to the mites, their eggs, and their waste. Within 4–6 weeks of infestation, raised, red bumps, blisters, or pimple-like rashes appear, often in skin folds—between fingers, wrists, elbows, armpits, waist, buttocks, and genital areas. In infants and young children, the rash may also appear on the face, scalp, palms, and soles. A telltale sign is thin, irregular burrow tracks (2–10 mm long) on the skin, though these are harder to spot. If left untreated, chronic scratching can lead to secondary infections, such as impetigo or cellulitis, marked by warmth, swelling, and pus-filled sores.
Severity and Risk Factors: Who’s Most Affected?
While anyone can contract scabies, certain groups are more vulnerable to severe symptoms. Immunocompromised individuals, the elderly, and young children often experience a more aggressive form called *crusted scabies* (or Norwegian scabies). Here, thousands of mites infest the skin, causing thick, scaly crusts that may not itch but can easily spread the infestation. Caregivers, healthcare workers, and those in close-quarter settings (nursing homes, prisons) face higher transmission risks. Notably, scabies is not a sign of poor hygiene; it spreads through prolonged skin-to-skin contact, shared bedding, or clothing.
Differentiating Scabies from Other Conditions
Misdiagnosis is common, as scabies symptoms mimic other skin conditions. Eczema, hives, or bedbug bites may cause similar itching and rashes, but scabies’ nocturnal itch and burrow tracks are distinctive. Unlike allergic reactions, scabies persists without treatment. If over-the-counter anti-itch creams provide temporary relief but the rash worsens, consult a healthcare provider. A definitive diagnosis often involves scraping a small skin sample to identify mites, eggs, or fecal matter under a microscope.
Treatment and Prevention: Practical Steps
Prescription-strength topical creams like permethrin 5% or oral medications such as ivermectin are standard treatments. Apply creams from neck to toes (for adults) or scalp to soles (for infants) and leave overnight, repeating after 7 days. Wash all clothing, bedding, and towels in hot water (50°C/122°F) and dry on high heat. Items that cannot be washed should be sealed in plastic bags for 72 hours. Avoid sexual or close physical contact until treatment is complete. For crusted scabies, multiple ivermectin doses and topical keratolytic agents may be necessary. Early intervention not only alleviates symptoms but also prevents community outbreaks.
Understanding scabies symptoms empowers individuals to seek timely care, reducing discomfort and transmission. While mange mites are not typically harmful to humans, their impact is far from trivial—recognizing and addressing the signs swiftly is key to resolution.
Are Spores Legal in Canada? Understanding the Current Laws and Regulations
You may want to see also

Prevention methods
Mange spores, primarily associated with animals, can pose risks to humans through direct contact or environmental exposure. While not all mange-causing mites infect humans, species like *Sarcoptes scabiei* can lead to scabies, a contagious skin condition. Prevention hinges on minimizing exposure and disrupting the mite’s lifecycle.
Step 1: Avoid Direct Contact with Infected Animals
Mites thrive on skin-to-skin contact. If an animal shows signs of mange—hair loss, redness, or intense itching—refrain from handling it until treated by a veterinarian. Wear gloves and long sleeves when caring for potentially infected pets, and wash hands thoroughly with soap and water afterward. For livestock or wildlife, consult professionals to avoid transmission.
Step 2: Sanitize Environments and Belongings
Mange mites can survive off-host for 2–3 days. Vacuum and dispose of the bag immediately to remove mites from carpets, upholstery, and bedding. Wash linens, clothing, and pet bedding in hot water (122°F/50°C) and dry on high heat for 10–30 minutes. For non-washable items, seal in plastic bags for 72 hours to starve mites.
Step 3: Use Preventive Treatments for Pets and Humans
Topical treatments like ivermectin (prescription required) or permethrin creams (e.g., Elimite 5%) can eradicate mites on humans. Follow dosage guidelines: permethrin is applied from neck down for 8–14 hours, then washed off, repeated after 1 week. For pets, veterinarians may prescribe selamectin (Revolution) or oral ivermectin, depending on species and weight.
Caution: Mites Adapt to Environmental Stress
While mites die quickly in dry, hot conditions, they tolerate cooler, humid environments. Avoid relying solely on air drying or cold washes. In agricultural settings, quarantine infected animals and disinfect pens with acaricides (mite-killing agents) like amitraz, following label instructions for dilution and application.
Prevention requires a combination of personal hygiene, environmental control, and targeted treatments. Early detection in animals and prompt action reduce human exposure risk. For persistent cases, consult a dermatologist or veterinarian to tailor interventions, ensuring mites are eradicated before they spread further.
Can Botulinum Spores Survive Stomach Acid? Unraveling the Truth
You may want to see also
Explore related products

Treatment options
Mange, caused by microscopic mites, primarily affects animals but can occasionally lead to human skin irritation known as sarcoptic mange or scabies. While human cases are rare, understanding treatment options is crucial for those exposed to infected animals. The cornerstone of treatment involves eliminating the mites and alleviating symptoms, typically through topical medications. Permethrin cream, a common choice, is applied from the neck down and left on for 8–14 hours before washing off. This process is repeated after one week to ensure all mites and eggs are eradicated. For severe cases or permethrin resistance, oral ivermectin may be prescribed, usually as a single dose followed by a second dose 1–2 weeks later, under strict medical supervision.
Beyond pharmaceuticals, environmental management plays a critical role in preventing reinfestation. Wash all clothing, bedding, and towels in hot water (at least 122°F or 50°C) and dry on high heat to kill mites. Items that cannot be washed should be sealed in plastic bags for at least 72 hours. Vacuuming and disposing of the vacuum bag immediately can help remove mites from carpets and furniture. Pets suspected of carrying mange must be treated simultaneously by a veterinarian to break the cycle of transmission.
For individuals with compromised immune systems or those experiencing severe itching, adjunctive treatments may be necessary. Antihistamines like diphenhydramine (25–50 mg every 6 hours) or hydroxyzine (25 mg every 6–8 hours) can reduce itching and improve sleep. Topical corticosteroids, such as hydrocortisone 1% cream, may be applied to inflamed areas for short periods to alleviate discomfort, but prolonged use should be avoided due to potential side effects.
A comparative analysis of treatment efficacy reveals that permethrin and ivermectin are equally effective in most cases, but ivermectin is reserved for treatment failures or systemic infestations. Natural remedies, such as tea tree oil or neem oil, lack robust clinical evidence and are not recommended as primary treatments. Cost and accessibility also factor into treatment choices, with permethrin being more affordable and widely available compared to ivermectin.
In conclusion, treating mange in humans requires a multi-faceted approach combining medication, environmental hygiene, and symptom management. Adherence to treatment protocols and coordination with healthcare providers and veterinarians are essential to ensure complete eradication and prevent recurrence. With prompt and proper intervention, most cases resolve within weeks, restoring comfort and peace of mind.
Cotton Grass: Flowering Conifer or Spore Producer? Unraveling the Mystery
You may want to see also

Animal-to-human spread
Mange, a skin disease caused by parasitic mites, primarily affects animals but raises questions about its potential to harm humans. While mange mites are species-specific, meaning they prefer animal hosts, certain types can cause temporary skin irritation in humans through a condition known as zoonotic mange. For instance, sarcoptic mange, caused by *Sarcoptes scabiei*, can lead to scabies-like symptoms in humans after close contact with infected animals. This highlights the importance of understanding animal-to-human transmission risks and taking preventive measures.
Consider the scenario of a pet owner whose dog has sarcoptic mange. Direct contact with the infected animal or its bedding can transfer mites to human skin. Symptoms typically appear within 1–4 days and include intense itching, redness, and small bumps, often misdiagnosed as allergies or insect bites. Unlike scabies in humans, zoonotic mange from animals does not burrow into human skin long-term, limiting infestation to superficial layers. However, repeated exposure can prolong symptoms, emphasizing the need for prompt treatment of both the animal and human.
Preventing animal-to-human spread of mange requires proactive steps. First, isolate infected animals and consult a veterinarian for treatment, often involving topical medications like selamectin or oral ivermectin. For humans, wash hands thoroughly after handling pets, and avoid sharing bedding or clothing with infected animals. If symptoms occur, seek medical attention for topical treatments such as permethrin cream (5% concentration), applied from neck to toes and left for 8–14 hours before washing off. Repeat application after one week to ensure mite eradication.
Comparatively, not all mange mites pose equal risks. For example, *Demodex* mites, responsible for demodectic mange in dogs, are highly species-specific and rarely affect humans. In contrast, *Sarcoptes scabiei* can cross species more readily, making sarcoptic mange a greater concern for zoonotic transmission. Understanding these differences helps tailor prevention strategies, such as prioritizing sarcoptic mange treatment in pets and maintaining hygiene practices to minimize exposure.
In conclusion, while mange spores (mites) from animals rarely cause long-term harm to humans, temporary skin irritation is possible, particularly with sarcoptic mange. By recognizing symptoms, treating infected animals promptly, and practicing good hygiene, the risk of animal-to-human spread can be effectively managed. Awareness and proactive measures are key to protecting both pets and their owners from the discomfort of zoonotic mange.
Does Bleach Kill Mold Spores? Uncovering the Truth Behind the Myth
You may want to see also
Frequently asked questions
Mange spores, specifically from sarcoptic mange (caused by the Sarcoptes scabiei mite), can infest humans, causing a condition known as scabies, but this is not the same as mange in animals.
While humans can experience temporary skin irritation or allergic reactions from contact with mange-infected animals, it typically does not lead to long-term illness or systemic disease.
Mange mites from animals (e.g., canine or feline scabies) can cause temporary skin irritation in humans but usually do not establish a full-blown mange infection, as they are not adapted to human hosts.
Humans exposed to mange spores may experience itching, redness, or a rash, but these symptoms are typically mild and resolve once contact with the infected animal is avoided.