Gastroparesis, a condition characterized by delayed stomach emptying, often requires careful dietary management to avoid symptoms like nausea, bloating, and abdominal pain. When considering whether someone with gastroparesis can eat cream of mushrooms, it’s essential to evaluate the dish’s ingredients and consistency. Cream of mushrooms typically contains dairy (cream) and mushrooms, both of which can be problematic for some individuals with gastroparesis. Dairy may exacerbate symptoms due to its fat content, while mushrooms, being fibrous, can be difficult to digest. However, if the soup is well-blended and low in fat, it might be tolerated in small portions. Consulting a healthcare provider or dietitian is crucial to determine if cream of mushrooms can be safely incorporated into a gastroparesis-friendly diet.
| Characteristics | Values |
|---|---|
| Dietary Restrictions | Gastroparesis patients are often advised to avoid high-fat foods, as they can slow digestion and worsen symptoms. Cream of mushroom soup, being cream-based, is typically high in fat. |
| Fiber Content | Mushrooms themselves are low in fiber, but the soup may contain added ingredients (e.g., thickeners) that could affect tolerance. |
| Individual Tolerance | Tolerance varies widely among gastroparesis patients. Some may tolerate small amounts of cream-based soups, while others may experience discomfort. |
| Low-Fat Alternatives | Opting for low-fat or fat-free versions of cream of mushroom soup may be better tolerated. |
| Portion Control | Small portions are recommended to minimize the risk of triggering symptoms. |
| Consultation | Always consult a healthcare provider or dietitian before introducing new foods into a gastroparesis diet. |
| Symptom Monitoring | Patients should monitor their symptoms after consuming cream of mushroom soup to assess tolerance. |
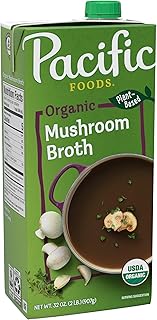
| Alternative Options | Consider broth-based mushroom soups or pureed mushroom dishes as lower-fat alternatives. |
| Added Ingredients | Check for added ingredients like onions, garlic, or spices, which may irritate the stomach in some individuals. |
| Hydration | Ensure adequate hydration when consuming cream-based soups, as they can be thick and potentially dehydrating. |
Explore related products
$15.29 $19.99
What You'll Learn
- Low-Fiber Mushroom Options: Choose well-cooked, canned, or pureed mushrooms to minimize fiber content for easier digestion
- Cream Base Tolerance: Opt for lactose-free or plant-based cream to avoid dairy-related gastrointestinal discomfort
- Portion Control Tips: Consume small, frequent servings to prevent overwhelming the delayed gastric emptying
- Symptom Monitoring: Track bloating, nausea, or pain after eating to assess individual tolerance levels
- Consultation with Dietitian: Seek professional advice to tailor mushroom cream dishes to gastroparesis dietary needs

Low-Fiber Mushroom Options: Choose well-cooked, canned, or pureed mushrooms to minimize fiber content for easier digestion
For individuals with gastroparesis, managing fiber intake is crucial to avoid exacerbating symptoms like bloating, nausea, and abdominal pain. Mushrooms, while nutritious, can be high in fiber, particularly when consumed raw or lightly cooked. However, by selecting low-fiber mushroom options—such as well-cooked, canned, or pureed varieties—those with gastroparesis can still enjoy this versatile ingredient without discomfort. The key lies in preparation methods that break down tough fibers, making digestion easier.
Well-cooked mushrooms are an excellent choice for gastroparesis-friendly diets. Prolonged cooking, such as sautéing or simmering for 20–30 minutes, softens the cell walls and reduces fiber content. For instance, adding mushrooms to a slow-cooked soup or stew allows them to tenderize fully, minimizing the risk of digestive distress. Pairing well-cooked mushrooms with low-fat cream or broth can create a soothing cream of mushroom dish that aligns with dietary restrictions often recommended for gastroparesis.
Canned mushrooms offer another practical option, as the canning process involves heat treatment that naturally reduces fiber. Opt for low-sodium varieties to avoid additional gastrointestinal strain. Canned mushrooms can be easily pureed or blended into creamy sauces, ensuring a smooth texture that’s gentle on the stomach. For example, blending canned mushrooms with a small amount of unsweetened almond milk and spices creates a fiber-reduced cream of mushroom alternative.
Pureed mushrooms are perhaps the most digestible form for those with gastroparesis. By processing mushrooms into a smooth consistency, fiber is broken down, and the dish becomes easier to tolerate. A simple recipe involves steaming mushrooms until tender, then blending them with a minimal amount of low-fat cream or plant-based milk. This method not only reduces fiber but also allows for better portion control, typically limiting servings to ½ cup to avoid overloading the digestive system.
When incorporating low-fiber mushroom options into a gastroparesis diet, it’s essential to monitor portion sizes and combine them with other low-fiber foods. For instance, pairing a small serving of pureed mushroom sauce with cooked white rice or gluten-free pasta can create a balanced, easy-to-digest meal. Always consult a healthcare provider or dietitian to tailor these options to individual tolerance levels, as responses to specific foods can vary. With careful preparation and mindful choices, cream of mushrooms can remain a comforting and enjoyable dish for those managing gastroparesis.
Mailing Psilocybin Mushrooms: Legal Risks and Postal Regulations Explained
You may want to see also

Cream Base Tolerance: Opt for lactose-free or plant-based cream to avoid dairy-related gastrointestinal discomfort
Individuals with gastroparesis often face challenges when consuming dairy products due to their high fat content, which can slow gastric emptying. Cream-based dishes, like cream of mushrooms, may exacerbate symptoms such as nausea, bloating, or abdominal pain. However, this doesn’t necessarily mean cream-based soups are off the table. By opting for lactose-free or plant-based cream alternatives, those with gastroparesis can enjoy similar textures and flavors without triggering dairy-related gastrointestinal discomfort.
Analyzing the options, lactose-free cream is processed to break down lactose, making it easier to digest for those with mild lactose intolerance. Plant-based alternatives, such as coconut cream or cashew cream, offer a dairy-free solution that aligns with vegan diets and avoids lactose altogether. Both options reduce the fat content compared to traditional heavy cream, which is crucial for managing gastroparesis symptoms. For instance, coconut cream contains medium-chain triglycerides (MCTs), which are metabolized faster than long-chain fats found in dairy, potentially easing digestion.
Incorporating these alternatives into cream of mushroom soup is straightforward. Substitute equal parts lactose-free or plant-based cream for traditional cream in recipes. For a smoother consistency, blend cashews with water until creamy, or use canned coconut cream for a richer texture. When preparing the soup, keep portions small—start with a ½ cup serving to monitor tolerance. Pairing the soup with low-fiber vegetables, like cooked carrots or zucchini, can further reduce digestive strain.
A comparative look at these alternatives reveals that lactose-free cream retains a dairy-like flavor, making it ideal for those who prefer traditional taste profiles. Plant-based options, however, introduce unique flavors—coconut cream adds a subtle sweetness, while cashew cream offers a neutral, nutty undertone. Experimenting with these options allows individuals to tailor the dish to their preferences while prioritizing digestive comfort.
In conclusion, cream of mushrooms can be adapted for gastroparesis by choosing lactose-free or plant-based cream alternatives. These swaps reduce fat content and eliminate lactose, minimizing the risk of gastrointestinal discomfort. Practical adjustments, such as portion control and ingredient pairing, further enhance tolerance. By embracing these modifications, individuals with gastroparesis can enjoy creamy, comforting dishes without compromising their digestive health.
Can Mushrooms Grow from Dead Mushrooms? Exploring Fungal Recycling
You may want to see also

Portion Control Tips: Consume small, frequent servings to prevent overwhelming the delayed gastric emptying
Managing gastroparesis often means rethinking how you eat, not just what you eat. For those wondering if cream of mushrooms can be part of their diet, the answer lies in portion control. Gastroparesis slows gastric emptying, so large meals can overwhelm the stomach, leading to discomfort, nausea, or vomiting. The key is to consume small, frequent servings—think 4–6 meals a day, each no larger than 1–1.5 cups. This approach prevents overloading the stomach while ensuring adequate nutrition. For cream of mushrooms, a typical serving should be around ½ cup, paired with easily digestible foods like steamed vegetables or plain rice.
Portion control isn’t just about reducing quantity; it’s about strategic timing. Aim to eat every 2–3 hours to maintain a steady flow of nutrients without taxing the digestive system. For example, start with a ½ cup of cream of mushrooms at lunch, followed by a small snack like a banana or crackers in the afternoon. Avoid eating within 2 hours of bedtime to give your stomach time to process the food. This structured approach minimizes the risk of symptoms flaring up while allowing you to enjoy a variety of foods, including cream of mushrooms, in moderation.
The science behind small, frequent meals is rooted in the mechanics of gastroparesis. When the stomach empties slowly, large volumes of food can ferment, causing bloating, pain, or reflux. By keeping portions small, you reduce the workload on the stomach, allowing it to process food more efficiently. For instance, a ½ cup serving of cream of mushrooms provides flavor and nutrients without overwhelming the system. Pairing it with low-fiber, low-fat ingredients further eases digestion, making it a viable option for those with gastroparesis.
Practical tips can make portion control easier to implement. Use measuring cups to ensure consistency in serving sizes, especially for creamy soups like cream of mushrooms. Invest in small, portion-controlled containers for meals and snacks. Keep a food diary to track what and when you eat, noting any symptoms that arise. This helps identify patterns and adjust portions accordingly. For example, if ½ cup of cream of mushrooms causes discomfort, try reducing it to ⅓ cup or blending it to a smoother consistency for easier digestion.
Ultimately, portion control is a balancing act—one that requires patience and experimentation. While cream of mushrooms can be part of a gastroparesis-friendly diet, its success depends on how it’s consumed. Small, frequent servings are the cornerstone of this strategy, ensuring the stomach isn’t overburdened. By adopting this approach, individuals with gastroparesis can enjoy a wider variety of foods without exacerbating their symptoms. It’s not about restriction but about mindful adaptation to support digestive health.
Can Iguanas Safely Eat Mushrooms? A Pet Owner's Guide
You may want to see also
Explore related products

Symptom Monitoring: Track bloating, nausea, or pain after eating to assess individual tolerance levels
Individuals with gastroparesis often face a trial-and-error process when determining which foods they can tolerate. Cream of mushroom soup, with its creamy texture and mushroom content, may trigger symptoms in some but not others. Symptom monitoring becomes a critical tool for assessing personal tolerance levels. By systematically tracking bloating, nausea, or abdominal pain after consuming this dish, patients can identify patterns and make informed dietary choices. A food and symptom journal, noting portion sizes and timing, can provide valuable insights into how the body reacts.
Analyzing the data collected through symptom monitoring allows for a nuanced understanding of individual triggers. For instance, a patient might notice that a small serving of cream of mushroom soup causes mild bloating but no nausea, while a larger portion leads to severe discomfort. This information can guide portion control and meal planning. Additionally, tracking symptoms over time can reveal whether tolerance changes, which is particularly important for gastroparesis patients whose condition may fluctuate. The goal is to create a personalized dietary profile that minimizes discomfort while maximizing nutritional intake.
Practical tips for effective symptom monitoring include using a standardized scale to rate symptoms (e.g., 1 for mild, 5 for severe) and recording meals immediately after consumption to ensure accuracy. Apps or templates designed for food tracking can streamline this process. It’s also essential to consider other factors, such as hydration levels and physical activity, which can influence symptom severity. For example, drinking water with a meal might exacerbate bloating in some individuals, while others may find it helps digestion. Consistency in tracking is key to identifying reliable patterns.
Comparing symptom monitoring to other dietary management strategies highlights its advantages. Unlike generic dietary restrictions, which may unnecessarily limit food choices, symptom monitoring tailors recommendations to the individual. It also empowers patients to take an active role in their care, fostering a sense of control over a condition that often feels unpredictable. However, it’s important to consult healthcare providers when interpreting results, as they can offer additional guidance and ensure nutritional needs are met. Symptom monitoring is not a standalone solution but a valuable component of a comprehensive gastroparesis management plan.
In conclusion, symptom monitoring provides a data-driven approach to navigating dietary challenges in gastroparesis. By tracking bloating, nausea, or pain after eating cream of mushroom soup or other foods, individuals can make informed decisions about their diet. This method requires patience and consistency but offers the potential for improved quality of life by reducing symptom flare-ups. With practical tools and a systematic approach, patients can transform uncertainty into actionable insights, one meal at a time.
Drying Oyster Mushrooms: A Simple Guide to Preserving Flavor
You may want to see also

Consultation with Dietitian: Seek professional advice to tailor mushroom cream dishes to gastroparesis dietary needs
Managing gastroparesis requires a meticulous approach to diet, and creamy dishes like mushroom soup often raise concerns due to their fat content and texture. While cream of mushrooms might seem off-limits, a consultation with a dietitian can transform this dish into a gastroparesis-friendly option. Dietitians specialize in tailoring meals to individual needs, considering factors like fat tolerance, portion size, and symptom triggers. By analyzing your specific condition, they can recommend modifications such as using low-fat cream substitutes, blending the soup to a smoother consistency, or incorporating digestive enzymes to aid absorption. This personalized approach ensures you enjoy the flavors without exacerbating symptoms.
For instance, a dietitian might suggest replacing heavy cream with unsweetened almond milk or silken tofu to reduce fat content while maintaining creaminess. They could also advise cooking mushrooms thoroughly to soften their fibrous texture, making them easier to digest. Portion control is another critical aspect; a dietitian may recommend starting with small servings, such as ½ cup, to monitor tolerance. Additionally, pairing the soup with a source of soluble fiber, like a small portion of cooked oatmeal, can help regulate digestion. These adjustments, guided by professional expertise, make cream of mushrooms a viable option for some individuals with gastroparesis.
It’s essential to recognize that gastroparesis varies widely among patients, and what works for one person may not work for another. A dietitian can conduct a thorough assessment, including reviewing your medical history, current symptoms, and dietary preferences, to create a customized plan. They may also introduce gradual dietary changes, starting with simpler forms of mushrooms, like sautéed or puréed, before progressing to cream-based dishes. This step-by-step approach minimizes the risk of discomfort and allows your body to adapt to new foods.
Beyond recipe modifications, a dietitian can educate you on broader dietary strategies for gastroparesis, such as eating smaller, more frequent meals and avoiding high-fat or high-fiber foods in large quantities. They can also address nutrient deficiencies, which are common in gastroparesis, by suggesting supplements or fortified foods. For example, if mushroom cream soup becomes a regular part of your diet, they might recommend adding vitamin D or calcium-fortified ingredients to compensate for potential nutrient gaps.
In conclusion, while cream of mushrooms may initially appear incompatible with gastroparesis, a dietitian’s expertise can make it a safe and enjoyable addition to your diet. Their ability to tailor recipes, monitor progress, and provide comprehensive dietary guidance ensures that you can explore flavorful options without compromising your health. If you’re considering incorporating cream of mushrooms into your meal plan, consulting a dietitian is not just advisable—it’s essential for navigating gastroparesis with confidence and creativity.
Mushrooms for Babies: Safe and Nutritious at 12 Months?
You may want to see also
Frequently asked questions
It depends on the individual’s tolerance, but cream of mushrooms is often high in fat and can be difficult to digest for those with gastroparesis. It’s best to consult a doctor or dietitian before consuming it.
Mushrooms are generally low in fiber and can be easier to digest when cooked, but creamy or fatty preparations like cream of mushrooms may worsen symptoms. Opt for simpler preparations if tolerated.
Yes, cream of mushrooms is high in fat, which can slow gastric emptying and exacerbate gastroparesis symptoms like nausea, bloating, or abdominal pain.
Low-fat versions may be better tolerated, but portion size and individual sensitivity still matter. Start with a small amount and monitor how your body reacts.
Broth-based soups with soft, low-fiber ingredients like cooked vegetables or lean proteins are often better tolerated than creamy soups like cream of mushrooms.