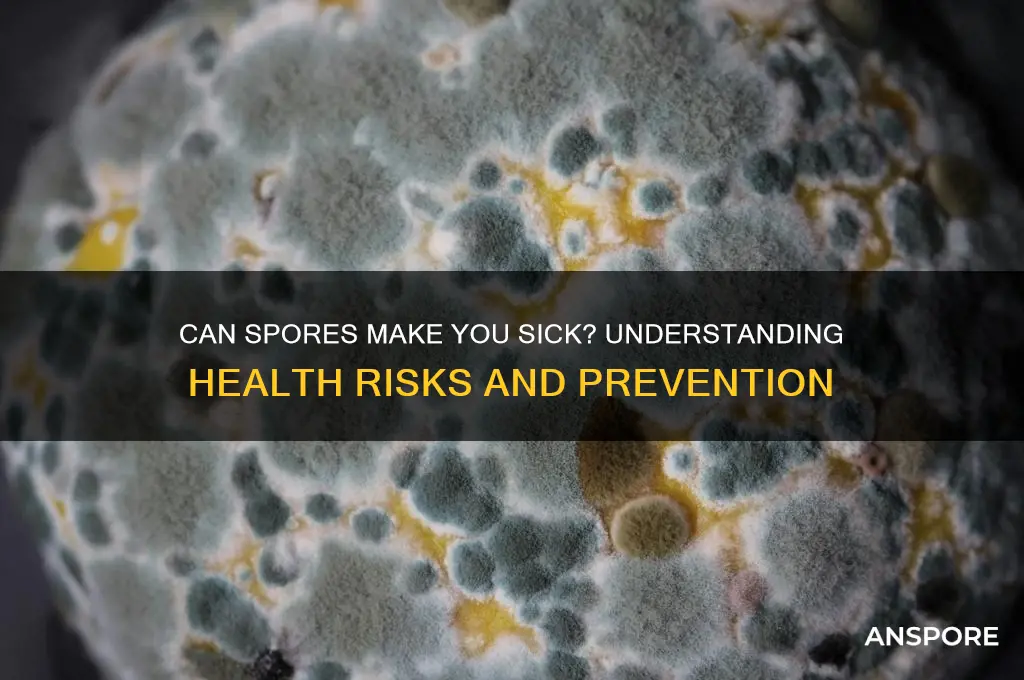
Spores, the reproductive units of certain bacteria, fungi, and plants, are ubiquitous in the environment and can survive in harsh conditions for extended periods. While many spores are harmless, some can pose health risks to humans, particularly those with weakened immune systems or pre-existing respiratory conditions. For instance, mold spores can trigger allergic reactions, asthma attacks, or infections when inhaled, while bacterial spores like those from *Clostridium botulinum* or *Bacillus anthracis* can cause serious illnesses such as botulism or anthrax if ingested or inhaled. Understanding the potential risks associated with spores is crucial for preventing exposure and managing health concerns effectively.
| Characteristics | Values |
|---|---|
| Can spores make you sick? | Yes, certain types of spores can cause illness in humans. |
| Types of harmful spores | Bacterial spores (e.g., Clostridium botulinum, Bacillus anthracis), fungal spores (e.g., Aspergillus, Candida), and mold spores. |
| Common illnesses caused by spores | Food poisoning (botulism), anthrax, aspergillosis, allergic reactions, respiratory issues, and infections in immunocompromised individuals. |
| Routes of exposure | Inhalation, ingestion (contaminated food/water), and skin contact. |
| Risk factors | Weakened immune system, pre-existing respiratory conditions, occupational exposure (e.g., agriculture, construction), and poor hygiene. |
| Prevention measures | Proper food handling, avoiding spore-rich environments, using protective gear (masks, gloves), maintaining clean living spaces, and staying up-to-date on vaccinations (e.g., anthrax vaccine). |
| Treatment | Antibiotics (bacterial infections), antifungal medications, allergy medications, and supportive care depending on the illness. |
| Environmental factors | Spores thrive in damp, humid conditions, and can be found in soil, decaying organic matter, and indoor environments with poor ventilation. |
| Detection methods | Air quality tests, food testing, and medical diagnostics (e.g., blood tests, imaging). |
| Latest research | Ongoing studies on spore resistance to disinfectants, climate change impacts on spore distribution, and development of targeted therapies for spore-related illnesses. |
Explore related products
What You'll Learn
- Inhalation Risks: Breathing in certain spores can lead to respiratory infections or allergic reactions
- Food Contamination: Spores in food cause illnesses like botulism if ingested
- Skin Infections: Direct contact with spores may cause fungal skin conditions
- Immune System Impact: Weakened immunity increases susceptibility to spore-related illnesses
- Environmental Exposure: Mold spores in damp areas trigger allergies and respiratory issues

Inhalation Risks: Breathing in certain spores can lead to respiratory infections or allergic reactions
Breathing in certain spores can expose you to pathogens like *Aspergillus* or *Histoplasma*, which thrive in environments such as moldy buildings or disturbed soil. These microscopic particles, when inhaled, can bypass your body’s initial defenses—like nasal hairs and mucus—and lodge deep in your respiratory tract. For individuals with compromised immune systems, this can lead to severe infections such as aspergillosis, a condition where fungal growth invades lung tissue. Even healthy individuals may experience symptoms like coughing, chest pain, or fever if exposed to high concentrations of these spores.
Consider the case of histoplasmosis, caused by inhaling spores of *Histoplasma capsulatum* from bird or bat droppings. This infection often mimics the flu but can progress to chronic lung disease in vulnerable populations, such as the elderly or those with HIV/AIDS. Studies show that prolonged exposure to spore-laden environments, like construction sites or caves, increases risk. For instance, a single hour of disturbing contaminated soil can release up to 10,000 spores per cubic meter of air, far exceeding safe inhalation thresholds.
To minimize inhalation risks, take proactive steps in high-risk areas. When working in dusty or moldy spaces, wear an N95 respirator to filter out spores. Ensure proper ventilation by using exhaust fans or opening windows. If you suspect spore contamination, avoid sweeping or vacuuming, as these actions aerosolize particles, increasing inhalation risk. Instead, mist the area with water to weigh down spores before cleaning. For those with respiratory conditions like asthma, consult a healthcare provider for personalized protection strategies.
Comparing spore inhalation to other respiratory hazards highlights its unique challenges. Unlike pollen or dust, spores can germinate inside the body, leading to systemic infections. While pollen allergies typically cause sneezing or itching, spore-induced reactions can include severe inflammation or fibrosis. This distinction underscores the importance of targeted prevention. For example, air purifiers with HEPA filters effectively capture spores but are less useful for gaseous pollutants, making them a smart investment for spore-prone environments.
Finally, recognize that not all spores are harmful, but knowing the source is critical. Indoor mold spores from *Stachybotrys* (black mold) can trigger allergic reactions or worsen asthma, while outdoor spores like *Alternaria* are common culprits in seasonal allergies. Monitoring indoor humidity below 50% and promptly fixing leaks can prevent mold growth. Outdoors, avoid disturbing soil or debris in areas known for fungal presence, especially during dry, windy conditions. Awareness and simple precautions can significantly reduce the risk of spore-related respiratory issues.
Using Grub Control with Milky Spore: Compatibility and Best Practices
You may want to see also

Food Contamination: Spores in food cause illnesses like botulism if ingested
Spores, the dormant survival structures of certain bacteria, can persist in food even under harsh conditions, posing a significant health risk if ingested. Unlike active bacteria, spores are highly resistant to heat, drying, and chemicals, making them difficult to eliminate through conventional cooking or processing methods. This resilience allows them to survive in a variety of foods, including canned goods, honey, and home-preserved items. When these spores find themselves in an environment conducive to growth, such as the low-oxygen conditions inside a sealed jar or the warm, nutrient-rich environment of the human gut, they can germinate into active bacteria, producing toxins that cause severe illness.
One of the most notorious illnesses caused by spore-forming bacteria is botulism, primarily associated with *Clostridium botulinum*. This bacterium produces a potent neurotoxin that can lead to paralysis and even death if left untreated. Infants are particularly vulnerable to botulism from consuming honey contaminated with *C. botulinum* spores, as their digestive systems are not yet developed enough to prevent spore germination. Adults are more likely to contract botulism from improperly canned or preserved foods, where spores have survived the canning process and multiplied in the absence of oxygen. Symptoms of botulism include blurred vision, difficulty swallowing, and muscle weakness, typically appearing within 12 to 36 hours of ingestion.
Preventing spore-related foodborne illnesses requires strict adherence to food safety practices. For home canning, always follow tested recipes and processing times from reliable sources like the USDA or National Center for Home Food Preservation. Pressure canning is essential for low-acid foods, as it reaches the high temperatures (240°F/116°C) needed to destroy spores. Avoid tasting or consuming food from swollen, leaky, or foul-smelling containers, as these are signs of bacterial growth. For infants under 12 months, never feed them honey, as it can harbor *C. botulinum* spores that their immature immune systems cannot handle.
Comparatively, while spores themselves are not harmful, their ability to transform into toxin-producing bacteria under specific conditions makes them a critical food safety concern. Unlike pathogens like *Salmonella* or *E. coli*, which are typically destroyed by thorough cooking, spores require extreme measures to eliminate. This distinction highlights the importance of understanding the unique risks posed by spore-forming bacteria and tailoring food handling practices accordingly. For instance, boiling water (212°F/100°C) is insufficient to destroy *C. botulinum* spores, whereas pressure canning effectively neutralizes them.
In conclusion, spores in food are a silent threat that can lead to severe illnesses like botulism if not managed properly. By understanding their behavior and implementing targeted prevention strategies, such as proper canning techniques and avoiding high-risk foods for vulnerable populations, individuals can significantly reduce the risk of spore-related contamination. Awareness and vigilance are key to ensuring that these resilient structures do not turn a meal into a dangerous health hazard.
Do Gymnosperms Produce Spores? Unraveling Their Unique Reproduction Methods
You may want to see also

Skin Infections: Direct contact with spores may cause fungal skin conditions
Spores, often microscopic and resilient, can linger on surfaces, fabrics, and even in the air, waiting for the right conditions to activate. When these dormant structures come into contact with your skin, they can trigger fungal infections, particularly in warm, moist environments where they thrive. Athlete’s foot, jock itch, and ringworm are common examples, caused by fungi like *Trichophyton* and *Epidermophyton*. These infections often start as itchy, red patches but can escalate to blisters, cracking, or discolored skin if left untreated. Understanding how spores behave and how to prevent their activation is key to protecting your skin.
To minimize the risk of spore-induced skin infections, adopt a proactive hygiene routine. After using public facilities like gyms or pools, wash your skin thoroughly with soap and dry it completely, especially between toes and folds where moisture accumulates. Wear breathable fabrics like cotton and change out of damp clothing promptly. For shared spaces, use protective barriers such as flip-flops in showers or your own yoga mat. If you suspect exposure, over-the-counter antifungal creams containing clotrimazole or miconazole can be effective for mild cases, but consult a healthcare provider if symptoms persist beyond two weeks or worsen.
Children and older adults are particularly vulnerable to spore-related skin infections due to developing or weakened immune systems. For kids, educate them on not sharing personal items like towels or brushes, which can harbor spores. For seniors, regular skin inspections and maintaining proper hydration can prevent cracks where spores might enter. In communal living settings, like schools or nursing homes, disinfect high-touch surfaces frequently and encourage hand hygiene to reduce spore transmission.
Comparing spore-related skin infections to bacterial or viral conditions highlights the importance of targeted treatment. While antibiotics are ineffective against fungi, antifungal medications work by disrupting cell membranes or inhibiting growth. Natural remedies like tea tree oil or garlic have antifungal properties but should complement, not replace, medical treatments. Unlike viral infections, fungal conditions are often curable with consistent care, but recurrence is common if spores remain in the environment. Regularly cleaning and disinfecting personal items and living spaces can break this cycle.
Finally, recognizing the signs of a spore-induced skin infection early can prevent complications. Look for persistent itching, unusual rashes, or skin that feels scaly or inflamed. If over-the-counter treatments fail, a dermatologist can prescribe stronger medications like oral terbinafine or topical ciclopirox. For those with chronic conditions like diabetes or compromised immunity, prompt medical attention is crucial to avoid severe infections. By staying informed and vigilant, you can keep spore-related skin issues at bay and maintain healthy, resilient skin.
Are Spore Syringes Legal in the UK? A Comprehensive Guide
You may want to see also
Explore related products

Immune System Impact: Weakened immunity increases susceptibility to spore-related illnesses
Spores, often dormant and resilient, can remain inert until conditions favor their growth. However, for individuals with compromised immune systems, these microscopic structures pose a significant threat. Weakened immunity, whether due to medical conditions like HIV/AIDS, cancer treatments, or autoimmune disorders, disrupts the body’s ability to recognize and neutralize spore-borne pathogens. This vulnerability increases the risk of infections such as aspergillosis, caused by *Aspergillus* spores, or histoplasmosis, triggered by *Histoplasma capsulatum*. Even common mold spores, harmless to most, can lead to severe respiratory issues in immunocompromised individuals.
Consider the case of aspergillosis, a fungal infection primarily affecting the lungs. Healthy individuals inhale *Aspergillus* spores daily without consequence, as their immune systems swiftly eliminate them. In contrast, those with weakened immunity may develop invasive aspergillosis, where the fungus proliferates unchecked, leading to symptoms like fever, chest pain, and coughing up blood. Treatment often involves antifungal medications such as voriconazole, but success rates drop significantly in immunocompromised patients. For instance, studies show that individuals undergoing chemotherapy or organ transplants face a mortality rate of up to 50% from this infection.
Practical steps can mitigate risks for those with weakened immunity. First, maintain indoor humidity below 50% to discourage mold growth, as spores thrive in damp environments. Use HEPA filters to reduce airborne spore counts, especially in bedrooms and living areas. Avoid activities like gardening or visiting dusty environments, where spore exposure is high. For high-risk individuals, healthcare providers may recommend prophylactic antifungal medications, particularly during neutropenic phases of cancer treatment. Regular monitoring for early signs of infection, such as persistent cough or unexplained fever, is crucial for timely intervention.
Comparatively, the impact of spores on immunocompromised individuals highlights the body’s reliance on a robust immune response. While healthy individuals may clear spore-related pathogens effortlessly, those with weakened defenses face a disproportionate burden. This disparity underscores the importance of tailored preventive measures and medical vigilance. For example, patients with chronic lung diseases like COPD, though not immunocompromised, still face elevated risks due to impaired lung function, emphasizing the need for context-specific precautions.
In conclusion, weakened immunity transforms spores from benign entities into potential threats. Understanding this dynamic empowers individuals and caregivers to adopt targeted strategies, from environmental modifications to medical interventions. By addressing susceptibility at its root, it’s possible to reduce the incidence of spore-related illnesses and improve outcomes for those most at risk. Awareness and proactive measures are key to navigating this hidden danger.
Does Staphylococcus Aureus Form Spores? Unraveling the Myth
You may want to see also

Environmental Exposure: Mold spores in damp areas trigger allergies and respiratory issues
Mold spores are ubiquitous in damp environments, lurking in basements, bathrooms, and even behind wallpaper. These microscopic particles thrive in moisture-rich conditions, often going unnoticed until their presence becomes a health hazard. When inhaled, mold spores can act as allergens, irritating the respiratory system and triggering a cascade of symptoms. For individuals with pre-existing allergies or asthma, exposure to mold spores can exacerbate conditions, leading to coughing, sneezing, and difficulty breathing. Even those without allergies may experience discomfort, as prolonged exposure can cause irritation and inflammation in the airways.
Consider the case of a family living in an older home with a leaky roof. Over time, moisture seeps into the walls, creating the perfect breeding ground for mold. Unaware of the hidden danger, they continue their daily lives until one member begins experiencing persistent nasal congestion and itchy eyes. A thorough inspection reveals mold growth behind the wallpaper, and air quality tests confirm elevated spore counts. This scenario underscores the importance of addressing moisture issues promptly to prevent mold proliferation and subsequent health risks.
Preventing mold-related illnesses starts with controlling indoor humidity levels. The Environmental Protection Agency (EPA) recommends maintaining indoor humidity below 60%, ideally between 30% and 50%. Use dehumidifiers in damp areas, ensure proper ventilation in bathrooms and kitchens, and promptly fix leaks in roofs, pipes, or windows. Regularly inspect areas prone to moisture, such as crawl spaces and basements, and clean visible mold with a solution of one cup of bleach per gallon of water. For extensive mold growth, consult professionals to avoid spreading spores during removal.
Children, the elderly, and immunocompromised individuals are particularly vulnerable to mold-related health issues. In schools, for instance, poorly maintained HVAC systems can circulate mold spores, leading to outbreaks of respiratory symptoms among students. A study published in the *Journal of Allergy and Clinical Immunology* found that children exposed to mold in the home were 2.4 times more likely to develop asthma. Similarly, elderly individuals with weakened immune systems may experience more severe reactions, including fungal infections in the lungs. Tailoring prevention strategies to these at-risk groups is essential for safeguarding public health.
While mold spores are a natural part of the environment, their concentration indoors can pose significant health risks. By understanding the link between damp conditions and mold growth, individuals can take proactive steps to mitigate exposure. From monitoring humidity levels to addressing water damage promptly, these measures not only protect respiratory health but also contribute to a safer, healthier living environment. Awareness and action are key to preventing mold spores from becoming silent triggers of illness.
Are Mushroom Spores Classified as Beasts in Worldbox?
You may want to see also
Frequently asked questions
Yes, inhaling certain spores, such as those from mold or fungi like Aspergillus, can cause respiratory issues, allergies, or infections, especially in individuals with weakened immune systems.
No, not all spores are harmful. Many spores, like those from plants or harmless fungi, are benign. However, some, such as those from toxic molds or bacteria like anthrax, can cause illness.
Yes, spores from bacteria like Clostridium botulinum (which causes botulism) or Bacillus cereus can survive cooking and produce toxins in food, leading to food poisoning if consumed.
To protect yourself, maintain good indoor air quality to prevent mold growth, avoid disturbing areas with visible mold, cook and store food properly, and seek medical advice if exposed to known harmful spores.