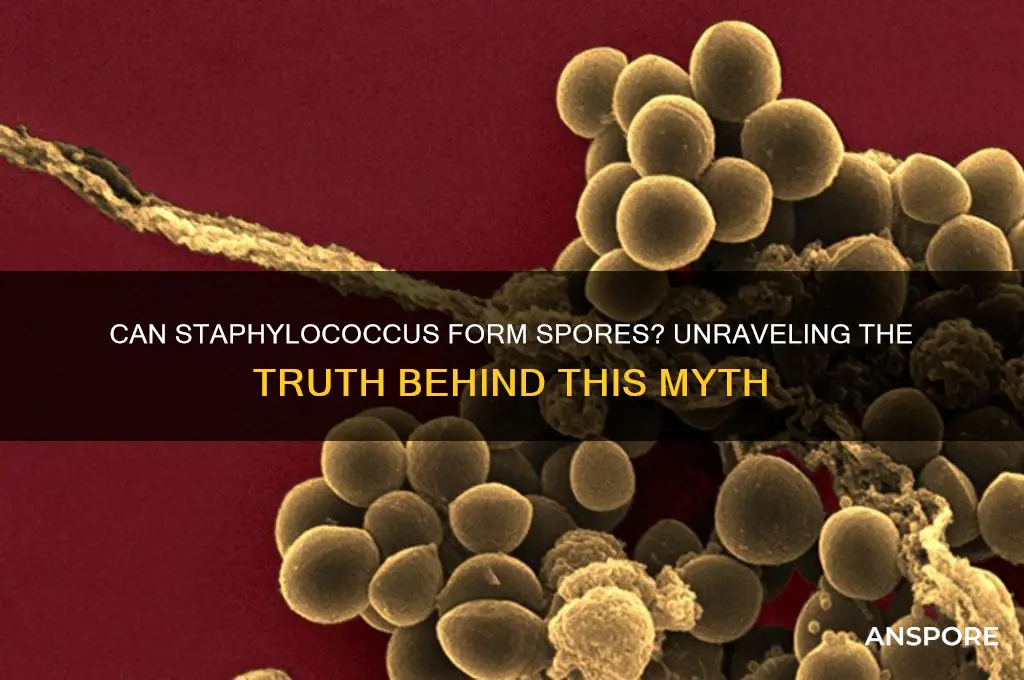
Staphylococcus, a genus of Gram-positive bacteria commonly found on the skin and mucous membranes of humans and animals, is known for its ability to cause a range of infections, from mild skin conditions to severe systemic diseases. However, unlike some other bacterial species such as Clostridium or Bacillus, Staphylococcus does not form spores. Sporulation is a survival mechanism that allows certain bacteria to withstand harsh environmental conditions by entering a dormant, highly resistant state. Since Staphylococcus lacks this capability, it relies on other strategies, such as biofilm formation and antibiotic resistance, to survive in diverse environments. Understanding the absence of spore formation in Staphylococcus is crucial for developing effective treatment and prevention strategies against staphylococcal infections.
| Characteristics | Values |
|---|---|
| Can Staphylococcus form spores? | No |
| Reason | Staphylococcus species are classified as non-spore-forming bacteria. |
| Cell Type | Gram-positive cocci (spherical bacteria) |
| Reproduction | Asexual reproduction via binary fission |
| Survival Mechanism | Can form biofilms and persist in harsh conditions without spore formation |
| Relevance | Important in clinical settings as a common cause of infections, but does not pose the additional challenge of spore-related persistence |
| Notable Species | Staphylococcus aureus, Staphylococcus epidermidis (both non-spore-forming) |
| Scientific Consensus | Universally accepted that Staphylococcus does not produce spores |
Explore related products
What You'll Learn
- Staphylococcus Species Overview: Briefly describe Staphylococcus genus, focusing on common species like S. aureus
- Sporulation Process: Explain the general process of spore formation in bacteria, contrasting with Staphylococcus
- Staphylococcus Sporulation Ability: Clarify if Staphylococcus can form spores, supported by scientific evidence
- Survival Mechanisms: Discuss alternative survival strategies of Staphylococcus, such as biofilm formation
- Clinical Implications: Highlight the impact of spore absence in Staphylococcus on infection treatment and control

Staphylococcus Species Overview: Briefly describe Staphylococcus genus, focusing on common species like S. aureus
Staphylococcus, a genus of Gram-positive bacteria, is ubiquitous in nature, colonizing the skin and mucous membranes of humans and animals. Among its 40 recognized species, *Staphylococcus aureus* stands out as the most clinically significant. Unlike spore-forming bacteria such as *Clostridium difficile*, *Staphylococcus* species do not produce spores, relying instead on robust biofilm formation and antibiotic resistance mechanisms for survival. This non-spore-forming characteristic is critical in understanding their persistence in healthcare settings and their susceptibility to specific disinfection methods.
Consider the implications of *S. aureus* in clinical practice. This species is notorious for causing skin infections, pneumonia, and food poisoning, often exacerbated by its ability to produce toxins like enterotoxins and exfoliative toxins. Methicillin-resistant *S. aureus* (MRSA), a strain resistant to beta-lactam antibiotics, poses a significant public health challenge. Without spore formation, *S. aureus* relies on genetic adaptability, such as acquiring resistance genes via mobile genetic elements, to thrive in hostile environments. This underscores the importance of targeted antimicrobial stewardship and infection control measures.
From a comparative perspective, the absence of spore formation in *Staphylococcus* contrasts sharply with spore-forming pathogens like *Bacillus anthracis*. While spores enable long-term survival in adverse conditions, *Staphylococcus* species depend on their ability to colonize hosts and exploit nutrient-rich environments. For instance, *S. epidermidis*, another common species, is a leading cause of catheter-related bloodstream infections due to its biofilm-forming capabilities. Understanding these differences informs the selection of disinfection strategies—spore-killing agents like autoclaving are unnecessary for *Staphylococcus*, but thorough cleaning and antimicrobial agents remain essential.
Practically, preventing *Staphylococcus* infections involves simple yet effective measures. Hand hygiene with alcohol-based sanitizers (at least 60% ethanol or isopropanol) reduces transmission, particularly in healthcare settings. For skin infections, topical antibiotics like mupirocin (2% ointment applied thrice daily for 5–10 days) are often prescribed. In food handling, maintaining temperatures below 4°C (39°F) inhibits *S. aureus* growth, while thorough cooking destroys preformed toxins. These targeted interventions highlight the importance of addressing *Staphylococcus*’s unique survival strategies in the absence of spore formation.
In conclusion, the *Staphylococcus* genus, exemplified by *S. aureus*, thrives without spore formation by leveraging biofilms, toxin production, and antibiotic resistance. This distinction shapes clinical management and infection control strategies, emphasizing the need for environment-specific interventions. By focusing on its non-spore-forming nature, healthcare providers and the public can effectively mitigate the risks posed by these pervasive bacteria.
Can Bacterial Spores Multiply? Unveiling Their Dormant Survival Mechanism
You may want to see also

Sporulation Process: Explain the general process of spore formation in bacteria, contrasting with Staphylococcus
Spore formation, or sporulation, is a survival mechanism employed by certain bacteria to endure harsh environmental conditions. This process involves a series of intricate cellular changes, culminating in the creation of a highly resistant spore. Typically, sporulation occurs in gram-positive bacteria like *Bacillus* and *Clostridium*, which, under nutrient deprivation or other stressors, initiate a genetic program to form spores. The process begins with the replication of the bacterial chromosome, followed by the assembly of a spore structure within the mother cell. This structure, known as the forespore, is encased in multiple protective layers, including a thick peptidoglycan cortex and a proteinaceous coat, which confer resistance to heat, desiccation, and chemicals. Unlike these spore-forming bacteria, *Staphylococcus* lacks the genetic machinery for sporulation, relying instead on other mechanisms like biofilm formation to survive adverse conditions.
To understand the contrast, consider the sporulation process in *Bacillus subtilis*, a well-studied model organism. When nutrients are scarce, a sigma factor (σ^H) activates genes responsible for sporulation. The cell then undergoes asymmetric division, creating a smaller forespore and a larger mother cell. The mother cell engulfs the forespore, which matures as the mother cell degrades its own DNA and synthesizes protective layers. This results in a spore capable of remaining dormant for years. In contrast, *Staphylococcus* species, such as *S. aureus*, do not undergo sporulation. Instead, they produce persistent cells or small colony variants (SCVs) under stress, which are metabolically dormant but not as resilient as spores. SCVs, for instance, can survive antibiotic treatment but lack the extreme durability of bacterial spores.
From a practical standpoint, the inability of *Staphylococcus* to form spores has significant implications in healthcare and food safety. While spore-forming bacteria like *Clostridium botulinum* require extreme conditions (e.g., 121°C for 15 minutes) for sterilization, *Staphylococcus* is more easily eradicated by standard pasteurization (72°C for 15 seconds). However, its ability to form biofilms on medical devices poses a persistent challenge. For example, *S. epidermidis* biofilms on catheters are resistant to antibiotics and host defenses, necessitating device removal. Understanding these differences highlights the importance of tailored strategies for controlling bacterial survival mechanisms.
A comparative analysis reveals why *Staphylococcus* does not sporulate. Unlike *Bacillus* or *Clostridium*, *Staphylococcus* lacks the *spo* genes essential for sporulation. Instead, it employs strategies like toxin production (e.g., staphylococcal enterotoxin) and antibiotic resistance (e.g., MRSA) to thrive in hostile environments. For instance, *S. aureus* can survive on dry surfaces for weeks, not due to sporulation, but because of its robust cell wall and ability to enter a dormant state. This distinction is crucial in clinical settings, where spore-forming bacteria require spore-specific disinfectants (e.g., hydrogen peroxide at 6% concentration), while *Staphylococcus* is effectively controlled with alcohol-based sanitizers.
In conclusion, while sporulation is a remarkable survival strategy for some bacteria, *Staphylococcus* relies on alternative mechanisms to endure stress. This difference underscores the need for targeted approaches in infection control and disinfection. For example, in food processing, spore-forming bacteria demand high-temperature treatments, whereas *Staphylococcus* is effectively eliminated by milder methods. Clinicians and researchers must remain vigilant, as the absence of sporulation in *Staphylococcus* does not diminish its threat—its adaptability and resilience continue to challenge healthcare systems worldwide.
Can Spores Survive in Honey? Unveiling the Sweet Preservation Mystery
You may want to see also

Staphylococcus Sporulation Ability: Clarify if Staphylococcus can form spores, supported by scientific evidence
Staphylococcus, a genus of Gram-positive bacteria commonly found on human skin and mucous membranes, is known for its ability to cause a range of infections, from minor skin conditions to life-threatening diseases. One question that often arises in microbiological discussions is whether Staphylococcus can form spores, a survival mechanism employed by some bacteria to withstand harsh environmental conditions. Scientific evidence unequivocally indicates that Staphylococcus does not form spores. Unlike spore-forming bacteria such as *Bacillus* and *Clostridium*, which produce endospores to survive extreme temperatures, desiccation, and chemicals, Staphylococcus relies on other strategies for persistence, such as biofilm formation and antibiotic resistance.
To understand why Staphylococcus lacks sporulation ability, it’s essential to examine its genetic makeup. Sporulation is a complex process regulated by specific genes, such as those in the *spo* operon found in *Bacillus subtilis*. Genomic analyses of Staphylococcus species, including *Staphylococcus aureus* and *Staphylococcus epidermidis*, reveal the absence of these sporulation-related genes. This genetic deficiency is a key factor in Staphylococcus’ inability to form spores. Instead, Staphylococcus has evolved alternative mechanisms, such as producing persistent cells (also known as "persister cells") that can survive antibiotic treatment by entering a dormant state without forming spores.
From a practical standpoint, the non-sporulating nature of Staphylococcus has significant implications for infection control and treatment. Since spores are not produced, standard disinfection methods, such as heat or chemical sterilants, are generally effective against Staphylococcus. For example, autoclaving at 121°C for 15 minutes or using 70% ethanol for surface disinfection can reliably eliminate Staphylococcus cells. However, its ability to form biofilms on medical devices, such as catheters and implants, poses a unique challenge, as biofilms provide a protective matrix that resists antimicrobial agents. Understanding this distinction—between sporulation and biofilm formation—is crucial for healthcare professionals designing infection prevention strategies.
Comparatively, the absence of sporulation in Staphylococcus contrasts sharply with spore-forming pathogens like *Clostridioides difficile*, which can survive for months in hospital environments. This difference highlights the importance of tailoring disinfection protocols to the specific survival mechanisms of the target organism. For instance, while spores require specialized methods like spore-specific disinfectants or prolonged heat treatment, Staphylococcus can be effectively controlled with routine cleaning practices. This knowledge underscores the need for accurate microbial identification and targeted interventions in clinical settings.
In conclusion, while Staphylococcus is a resilient pathogen, its inability to form spores simplifies its management compared to spore-forming bacteria. Scientific evidence, including genomic studies and experimental observations, confirms the absence of sporulation in Staphylococcus. By focusing on its alternative survival strategies, such as biofilm formation and antibiotic resistance, healthcare providers and researchers can develop more effective strategies to combat Staphylococcus-related infections. This clarity not only advances our understanding of microbial behavior but also informs practical approaches to infection control and treatment.
Lysol Spray vs. Spores: Effective Solution or Myth?
You may want to see also
Explore related products

Survival Mechanisms: Discuss alternative survival strategies of Staphylococcus, such as biofilm formation
Staphylococcus, unlike some bacterial species such as Clostridium and Bacillus, does not form spores. This absence of sporulation necessitates the development of alternative survival mechanisms to endure harsh environmental conditions. One of the most remarkable strategies employed by Staphylococcus is biofilm formation, a complex process that allows these bacteria to thrive in diverse settings, from hospital surfaces to human tissues. Biofilms are structured communities of bacteria encased in a self-produced extracellular matrix, which provides protection against antibiotics, host immune responses, and environmental stressors. For instance, Staphylococcus aureus biofilms are a leading cause of chronic infections, such as those associated with medical devices like catheters and prosthetics, where they can persist for months or even years.
To understand the significance of biofilm formation, consider the step-by-step process involved. First, planktonic (free-floating) Staphylococcus cells attach to a surface, often triggered by environmental cues like nutrient availability or surface charge. This initial attachment is reversible but quickly transitions to irreversible adhesion as the bacteria produce extracellular polymeric substances (EPS), including polysaccharides, proteins, and DNA. The EPS matrix not only anchors the bacteria but also facilitates cell-to-cell communication via quorum sensing, enabling coordinated behavior. As the biofilm matures, it develops a three-dimensional structure with channels for nutrient exchange and waste removal, resembling a microbial city. This organization enhances survival by creating microenvironments that protect bacteria from external threats.
While biofilm formation is a primary survival mechanism, Staphylococcus employs other strategies to endure adverse conditions. Phenotypic switching, for example, allows subpopulations of cells to adopt different phenotypes, such as small colony variants (SCVs). SCVs are slow-growing, highly persistent cells that can evade host immune responses and exhibit increased tolerance to antibiotics. This switching is particularly relevant in chronic infections, where SCVs can revert to the wild-type phenotype when conditions improve, ensuring long-term survival. Another strategy is persister cell formation, where a small fraction of the bacterial population enters a dormant, antibiotic-tolerant state. Persister cells are not mutants but phenotypic variants that can "wake up" and resume growth once the threat subsides, contributing to recurrent infections.
Comparatively, the survival mechanisms of Staphylococcus highlight its adaptability in the absence of sporulation. While spore-forming bacteria like Bacillus subtilis rely on a dormant, highly resistant form to survive extreme conditions, Staphylococcus leverages community-based strategies like biofilms and individual-level adaptations like SCVs and persister cells. This diversity of approaches underscores the bacterium's evolutionary success in colonizing and persisting in various niches. For healthcare professionals, understanding these mechanisms is crucial for developing effective treatment strategies. For example, disrupting biofilm formation through enzymes that degrade EPS or inhibiting quorum sensing could enhance the efficacy of antibiotics in treating Staphylococcus infections.
In practical terms, preventing Staphylococcus survival mechanisms requires a multifaceted approach. In clinical settings, rigorous disinfection protocols are essential to eliminate biofilms on surfaces and medical devices. Patients with implanted devices should be monitored for signs of infection, as biofilms can form within hours of device insertion. For individuals at risk, such as those with compromised immune systems or chronic conditions, proactive measures like wound care and antibiotic stewardship can reduce the likelihood of persistent infections. Additionally, research into novel therapies, such as anti-biofilm agents and persister cell-targeting drugs, offers hope for combating these resilient bacteria. By targeting their survival strategies, we can mitigate the impact of Staphylococcus in both healthcare and community settings.
Are Fern Spores Haploid? Unraveling the Mystery of Fern Reproduction
You may want to see also

Clinical Implications: Highlight the impact of spore absence in Staphylococcus on infection treatment and control
Staphylococcus, a genus of bacteria commonly associated with skin infections and food poisoning, lacks the ability to form spores. This biological limitation significantly influences clinical strategies for treating and controlling staphylococcal infections. Unlike spore-forming bacteria such as Clostridium difficile, which can survive harsh conditions and resist many disinfectants, Staphylococcus relies on its vegetative form for survival. This absence of spores simplifies certain aspects of infection management but also presents unique challenges in healthcare settings.
From a treatment perspective, the inability of Staphylococcus to form spores means that standard antibiotics and antiseptics are generally effective in eradicating the bacteria. For instance, methicillin-resistant *Staphylococcus aureus* (MRSA) infections are typically treated with antibiotics like vancomycin or daptomycin, which target the bacterial cell wall or membrane. Since spores are not present, there is no need for specialized treatments that penetrate dormant, resistant structures. However, the rise of antibiotic resistance in Staphylococcus strains underscores the importance of judicious antibiotic use and adherence to prescribed dosages, such as 15–20 mg/kg of vancomycin every 8–12 hours for severe infections in adults.
Infection control measures also benefit from the spore-free nature of Staphylococcus. Routine disinfection protocols using alcohol-based hand sanitizers (at least 60% ethanol or isopropanol) and quaternary ammonium compounds effectively eliminate vegetative staphylococci from surfaces and hands. This contrasts with spore-forming pathogens, which often require sporicidal agents like bleach or hydrogen peroxide for effective decontamination. For example, in healthcare facilities, daily cleaning of high-touch surfaces with alcohol wipes can significantly reduce staphylococcal transmission, particularly in intensive care units where patients are at higher risk.
However, the absence of spores does not eliminate the risk of persistent staphylococcal contamination. Biofilms, which are communities of bacteria encased in a protective matrix, pose a significant challenge in clinical settings. Staphylococcus can form biofilms on medical devices like catheters and prosthetics, rendering them resistant to antibiotics and disinfectants. To address this, healthcare providers must employ strategies such as using antimicrobial-coated devices and ensuring rigorous sterilization of reusable equipment. For instance, soaking catheters in a 0.2% chlorhexidine solution for 10 minutes before insertion can reduce biofilm formation.
In summary, the spore absence in Staphylococcus simplifies treatment and disinfection but necessitates targeted approaches to combat biofilm-related infections. Clinicians and infection control specialists must remain vigilant, combining evidence-based antibiotic use with proactive measures to prevent staphylococcal colonization and transmission. By understanding these nuances, healthcare systems can optimize patient outcomes and minimize the burden of staphylococcal infections.
Peziza Spores: Understanding Their Haploid or Diploid Nature Explained
You may want to see also
Frequently asked questions
No, Staphylococcus species are non-spore-forming bacteria.
Knowing that Staphylococcus does not form spores is crucial for understanding its survival mechanisms and designing effective disinfection methods, as spore-forming bacteria require more aggressive sterilization techniques.
Yes, some bacteria like Clostridium and Bacillus are spore-forming, but they are distinct from Staphylococcus in terms of genus and characteristics.
While Staphylococcus cannot form spores, it can develop resistance to antibiotics through mechanisms like genetic mutations, making it a significant concern in healthcare settings.