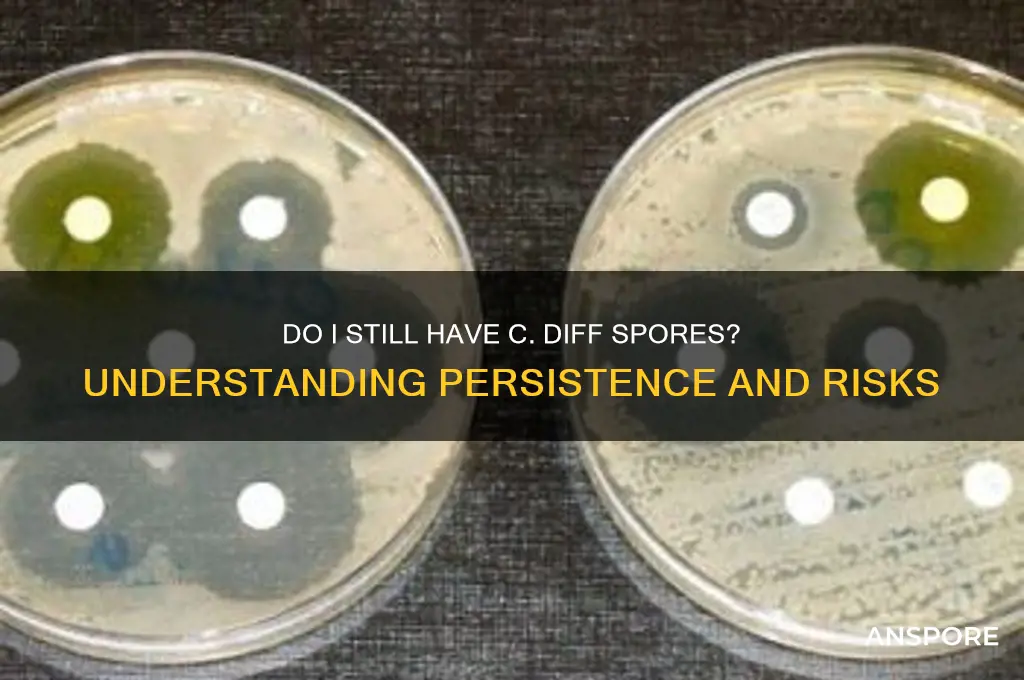
If you've previously been diagnosed with *Clostridioides difficile* (C. diff) infection, it’s natural to wonder whether you still carry the spores, even after successful treatment. C. diff spores are highly resilient and can persist in the environment and the gastrointestinal tract for extended periods, sometimes even years. While many people eliminate the bacteria and spores after completing antibiotics and recovering, others may remain asymptomatic carriers, meaning they harbor the spores without showing symptoms. Factors like a weakened immune system, recurrent infections, or continued exposure to healthcare settings can increase the likelihood of retaining spores. To determine if you still have C. diff spores, a healthcare provider may recommend a stool test or other diagnostic methods. It’s important to discuss your concerns with a medical professional, as they can provide personalized advice and guidance on managing potential risks or preventing transmission to others.
| Characteristics | Values |
|---|---|
| Persistence | C. diff spores can survive in the environment for months to years, especially in dry conditions. |
| Resistance | Highly resistant to alcohol-based sanitizers, most routine cleaning agents, and antibiotics. |
| Transmission | Spread via fecal-oral route, often through contaminated surfaces, hands, or healthcare settings. |
| Detection | Spores are not routinely detected by standard stool tests; specialized tests like toxin assays or PCR are needed. |
| Symptoms | Presence of spores alone does not cause symptoms; active infection with toxin-producing bacteria leads to diarrhea, abdominal pain, etc. |
| Treatment | Spores themselves are not treated; active infection is treated with specific antibiotics (e.g., vancomycin, fidaxomicin). |
| Recurrence Risk | Spores can remain in the gut, increasing the risk of recurrent C. diff infection, especially after antibiotic use. |
| Prevention | Hand hygiene with soap and water, thorough environmental cleaning with spore-killing agents (e.g., bleach), and infection control measures. |
| Immunity | No long-term immunity; reinfection is possible even after successful treatment. |
| Testing | If symptomatic, testing for C. diff toxins or genes (PCR) is recommended; asymptomatic carriers are not routinely tested. |
Explore related products
What You'll Learn
- Testing for C. diff Spores: Methods to detect persistent spores in stool or environment after treatment
- Recurrence Risks: Factors increasing chances of C. diff infection returning post-treatment
- Environmental Survival: How long C. diff spores can survive on surfaces or in surroundings
- Preventing Reinfection: Strategies to avoid re-exposure to C. diff spores after recovery
- Long-Term Effects: Potential health impacts of lingering C. diff spores in the body

Testing for C. diff Spores: Methods to detect persistent spores in stool or environment after treatment
Persistent *Clostridioides difficile* (C. diff) spores can linger in the gut or environment long after symptoms resolve, posing a risk of recurrence or transmission. Detecting these spores is crucial for assessing treatment efficacy and preventing reinfection. Several methods are available to identify C. diff spores in stool or environmental samples, each with unique advantages and limitations.
Toxigenic Culture Remains the Gold Standard
The most definitive method for detecting viable C. diff spores is toxigenic culture. This involves incubating a stool sample in a selective medium, such as cycloserine-cefoxitin-fructose agar (CCFA), to encourage spore germination and bacterial growth. After 24–48 hours, suspect colonies are tested for toxin production using assays like cell cytotoxicity neutralization or PCR for toxin genes (*tcdA* and *tcdB*). While highly specific, this method requires 48–72 hours for results and skilled laboratory personnel. It’s ideal for confirming active infection but less practical for rapid screening.
PCR-Based Tests Offer Speed but Lack Spore Specificity
Polymerase chain reaction (PCR) assays detect C. diff DNA in stool samples within hours, making them a popular choice for initial diagnosis. However, PCR cannot distinguish between vegetative cells, spores, or even residual DNA from dead bacteria. A positive PCR result post-treatment may indicate persistent spores, but it could also reflect non-viable remnants. Combining PCR with toxin detection (e.g., PCR for *tcdB* plus toxin A/B immunoassay) improves accuracy but still doesn’t confirm spore viability.
Environmental Sampling Requires Specialized Techniques
Detecting C. diff spores in the environment (e.g., hospital surfaces, equipment) is more challenging. Traditional methods like swabbing followed by culture are often insufficient due to spore hardiness and low concentrations. Enhanced techniques, such as spore-specific PCR or spore enrichment protocols (e.g., heating samples to 80°C for 10 minutes to kill vegetative cells), improve detection rates. Fluorescent in situ hybridization (FISH) or ATP bioluminescence can rapidly assess surface contamination but lack C. diff specificity.
Emerging Methods: Spore-Specific Markers and Molecular Tools
Research is advancing spore-specific detection methods. For instance, PCR assays targeting spore-associated genes (e.g., *spo0A*) or spore coat proteins offer promise. Additionally, metagenomic sequencing can identify C. diff spores in complex samples, though cost and complexity limit clinical use. Point-of-care tests, such as lateral flow immunoassays for spore antigens, are under development but not yet widely available.
Practical Considerations for Patients and Clinicians
For individuals concerned about persistent spores, stool testing post-treatment should focus on toxigenic culture or toxin detection, as PCR alone may yield false positives. Environmental decontamination requires spore-specific disinfectants (e.g., chlorine-based cleaners at 1,000–5,000 ppm) and thorough cleaning protocols. Patients should continue hand hygiene and isolate contaminated items until spores are eliminated. Regular follow-up with healthcare providers ensures timely detection of recurrence, especially in high-risk groups (e.g., elderly, immunocompromised).
In summary, detecting C. diff spores requires tailored methods depending on the sample type and context. While no single test is perfect, combining culture, molecular, and environmental approaches provides a comprehensive strategy to address persistent spores effectively.
Mixing Spores in Mushroom Grow Bags: Tips and Best Practices
You may want to see also

Recurrence Risks: Factors increasing chances of C. diff infection returning post-treatment
Recurrence of *Clostridioides difficile* (C. diff) infection is a significant concern, with up to 35% of patients experiencing a relapse after initial treatment. Understanding the factors that increase the likelihood of recurrence is crucial for prevention and management. One primary risk factor is the persistence of C. diff spores in the gut, which can remain dormant and reactivate under favorable conditions. These spores are highly resistant to antibiotics and environmental stressors, making them difficult to eradicate completely. Even after successful treatment, the presence of spores can lead to reinfection if the gut microbiome remains imbalanced or if the immune system is compromised.
Age plays a critical role in recurrence risk, with individuals over 65 facing higher chances due to age-related changes in gut flora and immune function. Older adults often have reduced microbial diversity, which can hinder the recovery of a healthy gut microbiome post-treatment. Additionally, prolonged antibiotic use, a common trigger for initial C. diff infection, further disrupts the gut ecosystem, creating an environment conducive to spore survival. For this demographic, healthcare providers may consider extended or tapered antibiotic regimens, such as a 10- to 14-day course of oral vancomycin followed by a gradual dose reduction, to minimize recurrence.
Another significant factor is the severity of the initial infection. Patients with severe or fulminant C. diff disease, characterized by symptoms like fever, elevated white blood cell count, and megacolon, are more likely to experience recurrence. This is partly because severe infections cause greater damage to the gut lining, allowing spores to persist and multiply more easily. In such cases, fecal microbiota transplantation (FMT) has emerged as a highly effective treatment option, with success rates exceeding 90% in resolving recurrent infections. FMT restores a healthy gut microbiome by introducing beneficial bacteria from a donor, thereby reducing the risk of spore reactivation.
Immunosuppression, whether due to underlying conditions like HIV or medications such as corticosteroids, also increases recurrence risk. A weakened immune system struggles to control C. diff spore germination and bacterial overgrowth, making relapse more probable. Patients in this category should be closely monitored post-treatment, and proactive measures like probiotic supplementation (e.g., *Saccharomyces boulardii* at a dose of 500 mg twice daily) may be recommended to support gut health. However, probiotics should be used cautiously, as their efficacy varies, and they are not a substitute for proven treatments.
Finally, environmental and behavioral factors contribute to recurrence. Hospitalization or residence in long-term care facilities increases exposure to C. diff spores, as these settings often harbor the bacterium. Poor hand hygiene and contaminated surfaces further elevate the risk of reinfection. Patients should adhere to strict hygiene practices, including frequent handwashing with soap and water (not alcohol-based sanitizers, which are ineffective against spores), and avoid unnecessary antibiotic use. For those with recurrent infections, household disinfection using chlorine-based cleaners (e.g., 1:10 dilution of bleach in water) can help reduce environmental spore reservoirs.
In summary, recurrence of C. diff infection is influenced by a combination of biological, environmental, and behavioral factors. Addressing these risks requires a multifaceted approach, including tailored treatment strategies, microbiome restoration, and vigilant hygiene practices. By understanding and mitigating these factors, patients and healthcare providers can significantly reduce the likelihood of relapse and improve long-term outcomes.
Exploring Interplanetary Warfare in Spore: Strategies and Possibilities
You may want to see also

Environmental Survival: How long C. diff spores can survive on surfaces or in surroundings
C. diff spores are remarkably resilient, capable of surviving on surfaces for weeks to months, depending on environmental conditions. These spores, the dormant form of *Clostridioides difficile*, are resistant to routine cleaning agents, including alcohol-based sanitizers, which makes them a persistent threat in healthcare settings and even in homes. Understanding their survival duration is crucial for implementing effective disinfection strategies to prevent transmission.
Temperature and humidity play a significant role in spore longevity. Studies show that C. diff spores can survive longer in cooler, drier environments, with some research indicating viability for up to 5 months on surfaces like countertops, doorknobs, and medical equipment. In contrast, warmer, more humid conditions may reduce survival time but still allow spores to persist for several weeks. This adaptability underscores the need for targeted cleaning protocols, particularly in high-risk areas.
Effective disinfection requires specific agents, such as chlorine-based cleaners (e.g., bleach solutions with 1:10 dilution of 5–6% sodium hypochlorite) or spore-specific disinfectants. These should be applied for at least 10 minutes to ensure spore inactivation. For non-porous surfaces, mechanical cleaning followed by disinfection is essential, as organic matter can protect spores from chemical agents. In healthcare settings, terminal cleaning protocols after C. diff infections are critical to breaking the chain of transmission.
Practical tips for home environments include using bleach-based cleaners on high-touch surfaces, washing fabrics in hot water with bleach, and ensuring proper hand hygiene with soap and water (not hand sanitizer). Regular cleaning of frequently touched items, such as phones, remote controls, and kitchen utensils, can further reduce spore persistence. For immunocompromised individuals or those with recurrent infections, consulting a healthcare provider for personalized environmental management strategies is advisable.
Comparatively, while C. diff spores outlast many other pathogens on surfaces, their survival is not indefinite. Consistent, evidence-based cleaning practices can significantly reduce their presence. The key takeaway is that environmental management is as important as medical treatment in controlling C. diff infections, emphasizing the need for vigilance in both healthcare and home settings.
Detecting Mold Spores: A Comprehensive Guide to Air Quality Testing
You may want to see also
Explore related products
$167.21 $180.21

Preventing Reinfection: Strategies to avoid re-exposure to C. diff spores after recovery
C. diff spores can persist in the environment for months, making re-exposure a significant concern after recovery. These resilient spores are resistant to many disinfectants and can survive on surfaces, clothing, and even skin. Understanding their tenacity is the first step in crafting a strategy to prevent reinfection.
Unlike other pathogens, C. diff spores don't require a living host to remain viable, allowing them to lurk in seemingly clean environments.
Disinfection Strategies: Bleach remains the gold standard for killing C. diff spores. A solution of 1 part bleach to 9 parts water (approximately 10% bleach) is effective. Apply this solution to all surfaces in the home, paying particular attention to high-touch areas like doorknobs, light switches, and bathroom fixtures. Allow the bleach solution to sit for at least 10 minutes before wiping it away. For items that can't be bleached, consider using a spore-killing disinfectant specifically labeled as effective against C. diff.
Regular laundry with hot water and bleach is crucial for clothing, bedding, and towels.
Hand Hygiene: Meticulous handwashing is paramount. Wash hands thoroughly with soap and warm water for at least 20 seconds after using the bathroom, before eating, and after any contact with potentially contaminated surfaces. Alcohol-based hand sanitizers are ineffective against C. diff spores, so rely on soap and water.
Environmental Awareness: Be mindful of potential spore reservoirs. Avoid sharing personal items like towels, washcloths, or utensils. If you have pets, ensure their living areas are regularly cleaned and disinfected. Consider using disposable gloves when cleaning areas potentially contaminated with fecal matter.
Dietary Considerations: Probiotics can help restore a healthy gut microbiome, which is crucial for preventing C. diff overgrowth. Discuss probiotic supplementation with your doctor, as specific strains may be more beneficial than others. A diet rich in fiber can also promote a healthy gut environment.
Long-Term Vigilance: Even after recovery, remain vigilant. If you experience any symptoms of C. diff infection, such as diarrhea, abdominal pain, or fever, seek medical attention immediately. Early detection and treatment are crucial to prevent complications and reduce the risk of spreading the infection. Remember, preventing reinfection is a multi-pronged approach requiring diligence in disinfection, hygiene, and environmental awareness. By implementing these strategies, you can significantly reduce your risk of re-exposure to C. diff spores and safeguard your health.
Can You See Truffle Spores? Unveiling the Mystery of Fungal Reproduction
You may want to see also

Long-Term Effects: Potential health impacts of lingering C. diff spores in the body
Lingering *Clostridioides difficile* (C. diff) spores in the body can act as silent reservoirs, potentially reactivating infection under the right conditions. Unlike active bacteria, spores are dormant and highly resistant to antibiotics and the body’s immune defenses. This resilience allows them to persist in the gut for months or even years, particularly in individuals with compromised immunity, frequent antibiotic use, or altered gut microbiota. While not always symptomatic, these dormant spores pose a risk of recurrence, especially when the gut environment shifts—such as after a course of antibiotics or during periods of stress. Understanding this dynamic is critical for managing long-term health risks associated with C. diff.
The presence of lingering C. diff spores can lead to recurrent infections, a significant concern for vulnerable populations. Studies show that up to 30% of individuals experience a recurrence within 8 weeks of initial treatment, often due to spore reactivation. Each recurrence increases the likelihood of further episodes, creating a cycle that can severely impact quality of life. For older adults, those with chronic illnesses, or individuals on prolonged antibiotic regimens, the risk is particularly heightened. Recurrent C. diff infections are not only physically debilitating but also emotionally taxing, often requiring aggressive treatment strategies like fecal microbiota transplantation (FMT) to restore gut balance.
Beyond recurrent infections, lingering C. diff spores may contribute to long-term gut dysbiosis, a condition where the gut microbiome remains imbalanced. This imbalance can lead to chronic gastrointestinal symptoms such as diarrhea, abdominal pain, and bloating, even in the absence of active infection. Prolonged dysbiosis has been linked to broader health issues, including malnutrition, weakened immune function, and increased susceptibility to other pathogens. For instance, a disrupted gut microbiome can impair nutrient absorption, leading to deficiencies in vitamins B12 and D, which are critical for energy and bone health. Addressing dysbiosis often requires dietary modifications, probiotics, and, in severe cases, FMT to reintroduce beneficial bacteria.
Another potential long-term effect of lingering C. diff spores is their impact on mental health. Chronic gastrointestinal symptoms and the fear of recurrence can lead to anxiety, depression, and reduced overall well-being. A 2020 study published in *Gut Microbes* found that individuals with recurrent C. diff infections reported significantly higher levels of anxiety and depression compared to those without a history of the infection. This psychological toll underscores the need for holistic management strategies that include mental health support alongside medical treatment. For those experiencing persistent symptoms, consulting a gastroenterologist and a mental health professional can provide a comprehensive approach to care.
Practical steps to mitigate the risks of lingering C. diff spores include maintaining a balanced diet rich in fiber and fermented foods to support gut health, avoiding unnecessary antibiotics, and practicing rigorous hand hygiene to prevent reinfection. For individuals with recurrent infections, emerging therapies like spore-targeted antibiotics (e.g., ridinilazole) and vaccines under development offer hope for more effective management. Monitoring for symptoms and regular follow-ups with healthcare providers are essential for early detection and intervention. While C. diff spores can be persistent, proactive measures can significantly reduce their long-term impact on health.
Breathing C. Diff Spores: Risks, Prevention, and Air Safety Tips
You may want to see also
Frequently asked questions
C. diff spores can persist in the body for weeks to months after treatment, even if symptoms have resolved. They are highly resistant and can survive in the environment and gut, increasing the risk of recurrence.
Yes, C. diff spores can be shed in stool even after symptoms disappear, making it possible to spread the infection to others. Proper hygiene, including handwashing with soap and water, is crucial to prevent transmission.
While treatment can eliminate the active infection, C. diff spores may remain in the gut or environment indefinitely. Some individuals may become asymptomatic carriers, meaning they harbor spores without showing symptoms but can still spread the bacteria.