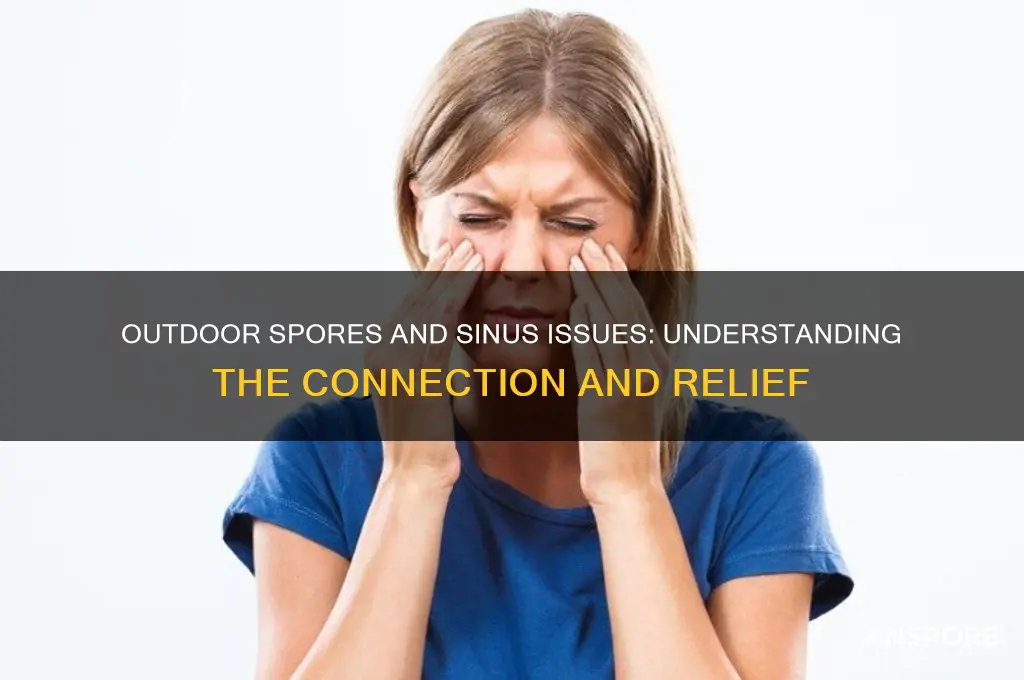
Outdoor spores, such as pollen, mold, and fungal particles, can significantly impact sinus health, particularly for individuals with allergies or sensitivities. These microscopic particles are ubiquitous in the environment, especially during certain seasons or in damp, humid conditions. When inhaled, they can irritate the nasal passages and sinuses, triggering symptoms like sneezing, congestion, runny nose, and facial pressure. For those with conditions like allergic rhinitis or sinusitis, exposure to outdoor spores can exacerbate inflammation and discomfort. Understanding the relationship between outdoor spores and sinus issues is essential for managing symptoms and seeking appropriate preventive measures or treatments.
| Characteristics | Values |
|---|---|
| Outdoor Spores and Sinus Issues | Outdoor spores, particularly from molds, fungi, and pollen, can irritate the sinuses in sensitive individuals. |
| Common Symptoms | Sneezing, nasal congestion, runny nose, itchy eyes, sinus pressure, and headaches. |
| Affected Individuals | People with allergies, asthma, sinusitis, or a weakened immune system are more susceptible. |
| Types of Spores | Mold spores (e.g., Alternaria, Cladosporium), fungal spores, and pollen from grasses, trees, and weeds. |
| Seasonal Impact | Spores are more prevalent in warm, humid weather, typically during spring, summer, and fall. |
| Prevention Measures | Stay indoors during high spore counts, use air purifiers, keep windows closed, and wear masks outdoors. |
| Medical Advice | Consult an allergist for testing, consider antihistamines, nasal corticosteroids, or immunotherapy. |
| Environmental Factors | Damp environments, decaying leaves, and outdoor composting can increase spore exposure. |
| Long-Term Effects | Chronic sinusitis or exacerbation of existing respiratory conditions if exposure is prolonged. |
| Latest Research | Studies suggest climate change may increase spore counts, potentially worsening sinus-related issues. |
Explore related products
What You'll Learn

Common Outdoor Spores Identified
Outdoor spores are ubiquitous, and their impact on sinus health varies depending on the type and concentration. Among the most common outdoor spores are those from Alternaria, a fungus often found in soil, plants, and organic debris. This spore is a well-documented allergen, with studies showing that sensitivity to Alternaria can lead to sinus inflammation, particularly in individuals with pre-existing allergies or asthma. For example, a 2018 study published in the *Journal of Allergy and Clinical Immunology* found that exposure to Alternaria spores correlated with increased sinus symptoms in 60% of allergic participants. To minimize exposure, consider wearing a mask during outdoor activities in damp or windy conditions, as these spores thrive in such environments.
Another prevalent outdoor spore is Cladosporium, which is commonly found on decaying plant material and in the air. Unlike Alternaria, Cladosporium is less likely to cause severe sinus issues in most people but can still trigger mild irritation or congestion in sensitive individuals. Interestingly, its presence peaks during late summer and early fall, coinciding with seasonal allergy flare-ups. A practical tip for reducing indoor Cladosporium levels is to use a HEPA air purifier, especially in bedrooms, as this can significantly lower spore counts and improve sinus comfort.
Aspergillus spores, while less allergenic than Alternaria, are noteworthy for their ability to colonize damp environments, such as compost piles or rotting wood. Prolonged exposure to high concentrations of Aspergillus can lead to sinus infections, particularly in immunocompromised individuals. For instance, a case study in *Clinical Microbiology Reviews* highlighted a patient who developed chronic sinusitis after repeated exposure to Aspergillus-infested soil. To avoid this, limit time spent in areas with visible mold or mildew, and ensure proper ventilation in basements or sheds where these spores may accumulate.
Lastly, Penicillium spores, often associated with indoor mold, are also found outdoors in soil and decaying vegetation. While primarily known for their role in food spoilage, outdoor Penicillium can irritate sinuses, especially when inhaled in large quantities. A 2020 study in *Environmental Health Perspectives* suggested that outdoor Penicillium levels above 1,000 spores per cubic meter of air increased the risk of sinus symptoms by 25%. To mitigate this, monitor local spore counts through allergy forecast apps and plan outdoor activities accordingly, particularly during rainy seasons when Penicillium thrives.
Understanding these common outdoor spores and their specific characteristics empowers individuals to take proactive steps in managing sinus health. By identifying peak seasons, high-risk environments, and practical mitigation strategies, one can significantly reduce the bothersome effects of these spores on the sinuses.
Using a Controller for Spore on Steam: Compatibility and Setup Guide
You may want to see also

Symptoms of Sinus Irritation
Outdoor spores, such as pollen and mold, are ubiquitous in the environment and can significantly impact sinus health. When inhaled, these microscopic particles often trigger a cascade of symptoms that signal sinus irritation. The first noticeable sign is typically nasal congestion, where the sinuses become swollen and inflamed, making breathing difficult. This congestion is your body’s immediate response to foreign invaders, attempting to block their entry deeper into the respiratory system. For individuals with sensitivities, this reaction can be swift and intense, especially during peak spore seasons like spring and fall.
Beyond congestion, sinus irritation often manifests as persistent sneezing and itching in the nasal passages. These symptoms occur as the body tries to expel the irritants, but they can be both uncomfortable and disruptive to daily life. For instance, children and adults alike may experience frequent sneezing fits, particularly in the morning or after spending time outdoors. To mitigate this, allergists recommend limiting outdoor activities during high-spore-count hours, typically mid-morning and early evening, and using saline nasal sprays to flush out irritants.
Another hallmark of spore-induced sinus irritation is postnasal drip, a condition where excess mucus accumulates at the back of the throat. This can lead to coughing, sore throat, and even nausea, especially in older adults or those with pre-existing respiratory conditions. Drinking warm fluids and using a humidifier can help thin the mucus, providing temporary relief. However, if symptoms persist for more than a week, consulting a healthcare provider is advisable, as prolonged irritation may lead to sinus infections.
In severe cases, outdoor spores can cause facial pain or pressure, particularly around the eyes, forehead, and cheeks. This discomfort arises from inflamed sinus cavities and can be exacerbated by bending over or lying down. Over-the-counter pain relievers like ibuprofen (200–400 mg every 4–6 hours) can alleviate pain, but it’s crucial to address the root cause. Antihistamines, such as cetirizine (10 mg daily for adults), can reduce inflammation and block the body’s allergic response, offering more sustained relief.
Finally, sinus irritation from outdoor spores often coincides with fatigue and reduced productivity. The body’s constant effort to combat irritants drains energy, leaving individuals feeling tired and unfocused. Prioritizing indoor air quality by using HEPA filters and keeping windows closed during high-spore seasons can significantly reduce exposure. For those with chronic sensitivities, immunotherapy, such as allergy shots, may be a long-term solution to desensitize the immune system to specific spores. Recognizing these symptoms early and taking proactive measures can prevent minor irritation from escalating into more serious health issues.
Spore-Forming Rods in Water: Are They Harmful to Dogs?
You may want to see also

Seasonal Spores and Sinus Impact
Outdoor spores, particularly those from fungi and pollen, are a significant yet often overlooked trigger for sinus issues during specific seasons. These microscopic particles become airborne in higher concentrations during spring and fall, coinciding with fungal growth and plant pollination cycles. For individuals with sensitive sinuses or allergies, this seasonal surge can lead to inflammation, congestion, and discomfort. Understanding the types of spores prevalent in your region and their peak seasons is the first step in mitigating their impact on your sinus health.
Analyzing the relationship between seasonal spores and sinus symptoms reveals a clear pattern. Fungal spores, such as those from Alternaria and Cladosporium, are most abundant in late summer and early fall, while pollen from trees, grasses, and weeds dominates spring and early summer. Exposure to these spores can cause allergic rhinitis, characterized by sneezing, itching, and nasal congestion. For those with sinusitis, the inflammation can worsen, leading to facial pain, headaches, and reduced sense of smell. Monitoring local spore counts through weather apps or allergy forecasts can help individuals prepare for high-risk days.
To minimize the impact of seasonal spores on your sinuses, consider implementing practical measures. During high-spore seasons, keep windows closed, especially in the early morning and evening when spore counts are highest. Use high-efficiency particulate air (HEPA) filters in your home to reduce indoor spore levels. For outdoor activities, wear a mask to limit inhalation of spores, particularly in areas with dense vegetation. Nasal rinses with saline solution can also help clear spores from the sinuses, reducing irritation and inflammation.
Comparing the effectiveness of various interventions highlights the importance of a multi-faceted approach. While antihistamines and decongestants provide symptomatic relief, they do not address the root cause of spore-induced sinus issues. Immunotherapy, such as allergy shots or sublingual tablets, can desensitize the immune system to specific spores over time, offering long-term relief. However, this treatment requires a commitment of several years and is most effective for individuals with identified spore allergies. Combining medication with environmental controls yields the best outcomes for managing seasonal spore-related sinus problems.
In conclusion, seasonal spores pose a tangible threat to sinus health, but proactive measures can significantly reduce their impact. By staying informed about local spore trends, adopting protective habits, and exploring targeted treatments, individuals can navigate high-spore seasons with greater comfort. For those with persistent or severe symptoms, consulting an allergist or ENT specialist is crucial for personalized management strategies. With the right approach, seasonal spores need not dictate the quality of your sinus health.
Can Mold Spores Hurt You? Understanding Health Risks and Prevention
You may want to see also
Explore related products

Preventive Measures for Relief
Outdoor spores, particularly mold and pollen, can significantly irritate the sinuses, leading to symptoms like congestion, sneezing, and headaches. To mitigate their impact, consider these preventive measures tailored for relief.
Step 1: Monitor Daily Pollen and Mold Counts
Check local weather forecasts or allergy apps for daily spore levels. Plan outdoor activities for times when counts are lowest, typically after rain or in the late afternoon. If counts are high, limit exposure by staying indoors with windows closed, especially during peak seasons like spring and fall.
Step 2: Use Nasal Rinses Regularly
Saline nasal rinses, such as those administered with a neti pot or squeeze bottle, flush out spores and irritants trapped in the sinuses. Use distilled or sterile water and a pre-mixed saline solution. Adults can rinse once or twice daily, while children over age 2 may benefit from a gentler, pediatrician-approved approach. Always clean the rinse device thoroughly to prevent contamination.
Step 3: Invest in Air Purification
HEPA air purifiers capture airborne spores, reducing indoor exposure. Place units in bedrooms and living areas, ensuring they’re sized appropriately for the room. For example, a 200 sq. ft. room requires a purifier with a CADR (Clean Air Delivery Rate) of at least 150. Change filters every 6–12 months for optimal performance.
Step 4: Modify Outdoor Habits
After spending time outside, change clothes and shower to remove spores from skin and hair. Wash bedding weekly in hot water to eliminate accumulated allergens. If gardening or doing yard work, wear an N95 mask to minimize spore inhalation, particularly during mold-prone activities like raking leaves or mowing lawns.
Step 5: Consider Over-the-Counter Remedies
Antihistamines (e.g., loratadine 10 mg daily for adults) and nasal corticosteroids (e.g., fluticasone 1–2 sprays per nostril daily) can preemptively reduce sinus inflammation. For adults with persistent symptoms, consult a healthcare provider for personalized options. Children under 12 should only use medications under medical guidance, with dosages adjusted for age and weight.
By combining these strategies, individuals can create a multi-layered defense against outdoor spores, minimizing sinus discomfort and improving overall quality of life. Consistency is key—implement these measures proactively, not just when symptoms arise.
Can Acid Reflux Cause Sporotrichosis in the Mouth?
You may want to see also

When to Seek Medical Help
Outdoor spores, particularly mold and pollen, can trigger sinus irritation, but not all reactions warrant medical attention. Mild symptoms like occasional sneezing or a runny nose often resolve with over-the-counter antihistamines (e.g., cetirizine 10 mg daily) or nasal saline rinses. However, persistent symptoms lasting over two weeks, such as thick nasal discharge, facial pain, or fever, suggest a sinus infection requiring medical evaluation. Adults over 65 or individuals with weakened immune systems should monitor symptoms closely, as they are more susceptible to complications.
Recognizing when symptoms escalate is crucial. If over-the-counter decongestants (e.g., pseudoephedrine 120 mg every 12 hours) provide no relief after 3–5 days, or if symptoms worsen—such as severe headache, tooth pain, or vision changes—seek immediate medical care. These could indicate a bacterial sinus infection or rare but serious conditions like orbital cellulitis. Children exhibiting irritability, high fever, or difficulty breathing also require prompt attention, as their sinuses are more vulnerable to infection.
For those with pre-existing conditions like asthma or allergies, outdoor spores can exacerbate symptoms, leading to sinusitis or bronchial inflammation. If you notice increased wheezing, shortness of breath, or nighttime coughing despite using prescribed inhalers (e.g., albuterol as needed), consult a healthcare provider. Allergy testing may be recommended to identify specific triggers, allowing for targeted immunotherapy or medication adjustments.
Prevention plays a key role in managing spore-related sinus issues. Practical steps include using HEPA air filters indoors, wearing masks during outdoor activities in high-pollen seasons, and monitoring local spore counts via weather apps. If symptoms persist despite these measures, a medical professional may prescribe corticosteroid nasal sprays (e.g., fluticasone 2 sprays per nostril daily) or oral steroids for severe cases. Early intervention can prevent chronic sinusitis and improve quality of life.
How Do Birds Nest Ferns Reproduce? Unveiling Their Spore-Based Life Cycle
You may want to see also
Frequently asked questions
Yes, outdoor spores like mold, pollen, and fungi can irritate the sinuses, leading to symptoms such as congestion, sneezing, and sinus pressure, especially in sensitive individuals.
Common culprits include mold spores, pollen from grasses, trees, and weeds, and fungal spores. These are more prevalent in damp, humid environments and during certain seasons.
Stay indoors on high pollen or mold count days, keep windows closed, use air purifiers, and wear masks when outdoors during peak spore seasons.
Yes, sinus irritation from outdoor spores often indicates a spore allergy or sensitivity, which can be confirmed through allergy testing.
Prolonged exposure to outdoor spores can inflame the sinuses, potentially leading to sinusitis (sinus infection), especially in individuals with pre-existing sinus conditions or weakened immune systems.