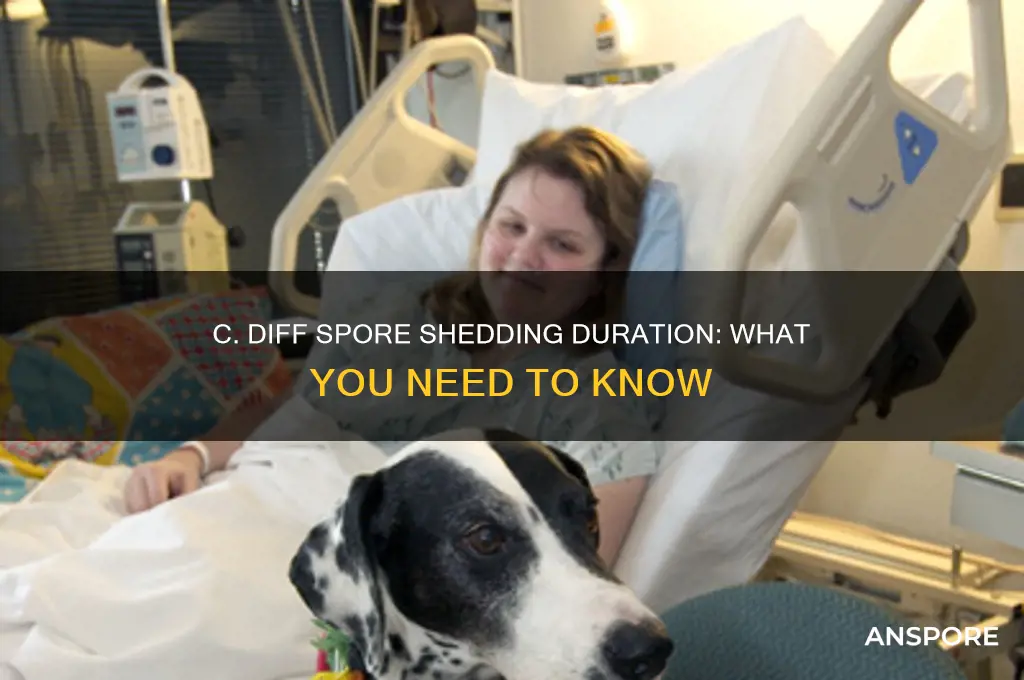
*Clostridioides difficile* (C. diff) is a bacterial infection that can cause severe diarrhea and other gastrointestinal symptoms, often following antibiotic use. One of the most concerning aspects of C. diff is its ability to produce spores, which are highly resistant to environmental conditions and can persist on surfaces for extended periods. After recovering from a C. diff infection, individuals may continue to shed spores in their stool, raising questions about how long they remain contagious. Understanding the duration of spore shedding is crucial for preventing the spread of the infection to others, especially in healthcare settings. Factors such as the severity of the infection, treatment effectiveness, and individual immune response can influence how long a person sheds spores. Typically, spore shedding can continue for several weeks after symptoms resolve, though some studies suggest it may persist for months in certain cases. Proper hygiene, environmental disinfection, and adherence to infection control measures are essential during this period to minimize transmission risks.
| Characteristics | Values |
|---|---|
| Duration of Spores Shedding | Up to several weeks to months after infection or treatment completion |
| Factors Affecting Shedding Duration | Severity of infection, immune status, antibiotic use, and treatment efficacy |
| Spores Detection Post-Treatment | Spores can be detected in stool for weeks to months after symptoms resolve |
| Infectivity of Shed Spores | Spores are highly resistant and can remain infectious in the environment |
| Risk of Transmission | Shedding spores increases risk of transmission to others |
| Prevention Measures | Hand hygiene, environmental cleaning, and isolation precautions |
| Testing for Spores | Stool tests (e.g., PCR or toxin assays) can detect spores post-treatment |
| Reinfection Risk | Prolonged shedding increases risk of recurrence or reinfection |
| Immune System Role | A weakened immune system may prolong shedding duration |
| Environmental Survival | Spores can survive on surfaces for weeks to months |
Explore related products
What You'll Learn

Duration of spore shedding post-treatment
After completing treatment for *Clostridioides difficile* (C. diff), patients often wonder how long they will continue to shed spores. Understanding this duration is crucial for preventing transmission and ensuring a safe environment for others. Research indicates that spore shedding can persist for several weeks to months post-treatment, even after symptoms have resolved. This variability depends on factors such as the severity of infection, the effectiveness of treatment, and individual immune response. For instance, a study published in the *Journal of Infection* found that 50% of patients still shed spores four weeks after treatment, while some continued to do so for up to 12 weeks.
Analyzing the data, it becomes clear that the type of treatment plays a significant role in spore shedding duration. Standard antibiotic regimens, such as oral vancomycin (125 mg every 6 hours for 10–14 days) or fidaxomicin (200 mg twice daily for 10 days), typically reduce symptoms within a week. However, spore shedding often outlasts clinical improvement. Fecal microbiota transplantation (FMT), an alternative treatment, has shown promise in reducing shedding duration by restoring gut microbiota balance more rapidly. Patients undergoing FMT may experience shorter shedding periods compared to those on antibiotics alone, though individual responses vary.
Practical tips can help minimize the risk of transmission during the shedding period. First, maintain rigorous hand hygiene, using soap and water instead of alcohol-based sanitizers, as spores are resistant to alcohol. Second, disinfect high-touch surfaces with chlorine-based cleaners, which are effective against C. diff spores. Third, avoid sharing personal items and ensure proper laundry practices, washing contaminated items separately with hot water and bleach. For healthcare settings, isolating patients with C. diff and adhering to contact precautions are essential until spore shedding ceases.
Comparing post-treatment shedding durations across age groups reveals interesting trends. Older adults, particularly those over 65, tend to shed spores for longer periods due to weakened immune systems and comorbidities. In contrast, younger, healthier individuals may clear spores more quickly. Pediatric cases often show shorter shedding durations, possibly due to less complex microbiota and robust immune responses. However, children in daycare or school settings require careful monitoring to prevent outbreaks, as they are more likely to contaminate environments through poor hygiene practices.
In conclusion, the duration of spore shedding post-treatment for C. diff varies widely, influenced by treatment type, age, and individual health status. While symptoms may resolve quickly, spores can persist for weeks to months, necessitating prolonged precautions. By understanding these factors and implementing practical measures, patients and caregivers can effectively manage the risk of transmission and protect vulnerable populations. Regular follow-up testing, such as stool toxin or PCR assays, can help determine when shedding has ceased, providing peace of mind and ensuring a safe return to normal activities.
Do You Need an EA Account to Play Spore? Explained
You may want to see also

Factors affecting prolonged spore shedding
The duration of spore shedding after a *Clostridioides difficile* (C. diff) infection varies widely, influenced by a complex interplay of factors. Understanding these factors is crucial for managing the risk of transmission and recurrence. From the severity of the initial infection to the nuances of antibiotic use, each element plays a distinct role in prolonging spore shedding. Here’s a breakdown of the key factors and their implications.
Severity of Infection and Immune Response: A more severe C. diff infection often correlates with prolonged spore shedding. Patients with severe diarrhea, fever, or complications like pseudomembranous colitis may shed spores for weeks to months. Conversely, those with mild infections typically clear spores faster. The immune system’s response is equally critical; immunocompromised individuals, such as those on chemotherapy or with HIV, may shed spores for extended periods due to reduced ability to eliminate the bacteria. For example, studies show that patients with neutropenia may shed spores for up to 6 months post-treatment, compared to 2–4 weeks in immunocompetent individuals.
Antibiotic Use and Microbiome Disruption: Antibiotics are a double-edged sword in C. diff infections. While they treat the infection, they also disrupt the gut microbiome, creating an environment conducive to spore persistence. Prolonged or repeated antibiotic use, especially with broad-spectrum agents like clindamycin or fluoroquinolones, can extend shedding duration. For instance, a patient treated with a 10-day course of metronidazole may shed spores for 4–6 weeks, whereas someone on a 14-day course of vancomycin might shed for 6–8 weeks. Restoring gut flora with probiotics or fecal microbiota transplantation (FMT) can shorten shedding time, but timing and dosage are critical—probiotics containing *Lactobacillus* or *Saccharomyces boulardii* should be started within 48 hours of antibiotic completion for optimal efficacy.
Age and Comorbidities: Older adults, particularly those over 65, are at higher risk for prolonged spore shedding due to age-related immune decline and increased comorbidities. Conditions like diabetes, chronic kidney disease, or inflammatory bowel disease further exacerbate this risk. For example, a 70-year-old with diabetes may shed spores for 10–12 weeks, compared to 4–6 weeks in a healthy 40-year-old. Practical tips for this demographic include strict hand hygiene, isolating the patient during active shedding, and regular environmental disinfection with chlorine-based cleaners (1:10 dilution of bleach) to reduce spore transmission.
Recurrent Infections and Strain Virulence: Recurrent C. diff infections, defined as two or more episodes within 8 weeks, significantly prolong spore shedding. Each recurrence increases the likelihood of becoming a chronic shedder, with some patients shedding spores for years. Hypervirulent strains, such as NAP1/BI/027, produce more spores and toxins, further extending shedding duration. For recurrent cases, tapered or pulsed vancomycin regimens (e.g., 125 mg every 2–3 days for 2 weeks) or FMT are recommended. FMT, with a success rate of 90% in resolving recurrent infections, can drastically reduce shedding time, often within 2–4 weeks post-procedure.
Environmental and Behavioral Factors: Environmental persistence of C. diff spores and poor hygiene practices contribute to prolonged shedding. Spores can survive on surfaces for months, reinfecting the host or spreading to others. Patients who fail to wash hands properly with soap and water (not hand sanitizer, which is ineffective against spores) or share personal items increase their shedding duration. Practical measures include using disposable gloves when cleaning, laundering linens in hot water (60°C or higher), and avoiding proton pump inhibitors (PPIs) unless medically necessary, as PPIs alter gut pH and may prolong spore viability.
In summary, prolonged spore shedding after C. diff is influenced by infection severity, immune status, antibiotic use, age, comorbidities, strain virulence, and environmental factors. Tailored interventions, such as microbiome restoration, targeted antibiotic regimens, and stringent hygiene practices, can mitigate shedding duration and reduce transmission risk. Awareness of these factors empowers patients and healthcare providers to manage C. diff more effectively.
Do Bacteria Form Resting Spores? Unveiling Microbial Survival Strategies
You may want to see also

Risk of recurrence and shedding
Clostridioides difficile (C. diff) infections are notorious for their recurrence, with up to 30% of patients experiencing a second episode after initial treatment. This risk is closely tied to the organism’s ability to produce resilient spores, which can persist in the environment and the gastrointestinal tract. Shedding of these spores continues even after symptoms resolve, creating a prolonged window for reinfection or transmission. Understanding the dynamics of spore shedding is critical for managing recurrence risk and preventing spread.
Analyzing the timeline of spore shedding reveals a complex interplay between treatment efficacy and individual factors. Studies indicate that C. diff spores can be detected in stool samples for weeks to months after successful treatment, with one study finding spores in 50% of patients three months post-therapy. Age, immune status, and antibiotic use influence shedding duration; older adults and immunocompromised individuals may shed spores for longer periods. For instance, a 70-year-old patient with a history of prolonged antibiotic use might continue shedding spores for up to six months, compared to a younger, healthier individual who may clear spores within eight weeks.
To mitigate recurrence risk, practical steps include stringent hand hygiene, environmental disinfection, and dietary modifications. Patients should use soap and water, as alcohol-based sanitizers are ineffective against spores. Surfaces in the home, particularly bathrooms, should be cleaned with bleach-based solutions (1:10 dilution of household bleach). Probiotics, such as *Saccharomyces boulardii* or multi-strain formulations, have shown promise in restoring gut flora and reducing recurrence, though consultation with a healthcare provider is essential. For example, a 60-year-old patient might be advised to take 500 mg of *S. boulardii* twice daily for four weeks post-treatment.
Comparatively, fecal microbiota transplantation (FMT) offers a more aggressive but highly effective approach for recurrent cases. By reintroducing a healthy microbial community, FMT achieves cure rates exceeding 90%. However, it carries risks, including infection transmission, and should be reserved for patients with multiple recurrences. For instance, a 55-year-old with two prior C. diff episodes might undergo FMT via colonoscopy, followed by monitoring for spore clearance through weekly stool tests.
In conclusion, managing the risk of recurrence and shedding requires a multifaceted strategy tailored to individual needs. From extended spore detection timelines to targeted interventions like probiotics and FMT, each approach addresses the unique challenges posed by C. diff. By combining vigilance, evidence-based treatments, and patient education, healthcare providers can significantly reduce the burden of this persistent infection.
Where to Buy Milky Spore in Canada: A Comprehensive Guide
You may want to see also
Explore related products

Preventing spore transmission during shedding
Shedding *C. diff* spores can last weeks to months after symptoms resolve, making transmission prevention critical during this period. Unlike active infection, spore shedding often occurs without symptoms, creating a stealthy risk for vulnerable populations like the elderly or immunocompromised. Understanding this timeline underscores the need for targeted hygiene practices to interrupt spore spread.
Hand hygiene reigns supreme. Alcohol-based hand sanitizers, though effective against many pathogens, are ineffective against *C. diff* spores. Instead, use soap and warm water for at least 40-60 seconds, especially after using the bathroom and before handling food or touching surfaces. This mechanical action physically removes spores, preventing hand-to-mouth transmission.
Pro Tip: Keep nails short and avoid wearing artificial nails, as spores can harbor beneath them.
Environmental disinfection is key. *C. diff* spores are resilient, surviving on surfaces for months. Use EPA-registered disinfectants labeled as "sporicidal" to clean high-touch areas like doorknobs, light switches, and bathroom surfaces. Pay particular attention to areas near the toilet, as spores are shed in feces. * Frequency Matters: Clean high-touch surfaces daily, and after any known exposure to fecal material.
Laundry Considerations: Wash soiled linens separately in hot water (160°F/71°C) with bleach or a bleach alternative. Dry thoroughly on high heat.
Isolation precautions may be necessary. In healthcare settings or households with vulnerable individuals, temporary isolation may be recommended during the shedding period. This involves using a dedicated bathroom, if possible, and minimizing contact with others until spore shedding subsides. * Communication is Crucial: Inform caregivers, family members, and healthcare providers about your recent *C. diff* infection to ensure appropriate precautions are taken.
Remember: Preventing spore transmission during shedding is a multi-pronged approach. By combining rigorous hand hygiene, thorough environmental disinfection, and, when necessary, isolation precautions, you can significantly reduce the risk of spreading *C. diff* to others.
Can You Kill Botulism Spores? Effective Methods and Safety Tips
You may want to see also

Testing for active spore shedding
After a *Clostridioides difficile* (C. diff) infection, determining how long you shed spores is crucial for preventing transmission. Testing for active spore shedding is a key step in this process, but it’s not as straightforward as a single test. Unlike active infection, which is detected through toxin or PCR tests, spore shedding requires specific methods to identify the presence of viable spores in stool. Here’s what you need to know.
Steps for Testing Active Spore Shedding:
- Stool Sample Collection: Collect a fresh stool sample in a sterile container. Ensure the sample is handled carefully to avoid contamination, as spores are highly resilient and can survive outside the body.
- Culture-Based Testing: The gold standard for detecting active spore shedding is a spore-specific culture. This involves incubating the stool sample in a selective medium that encourages spore germination and bacterial growth. If *C. diff* spores are present, they will grow into colonies, confirming shedding.
- Molecular Testing (PCR): While PCR tests detect *C. diff* DNA, they cannot differentiate between viable spores and non-viable remnants. However, combining PCR with culture methods can provide a more comprehensive assessment.
- Frequency of Testing: Repeat testing at intervals (e.g., weekly) to monitor shedding duration. Studies suggest shedding can persist for weeks to months after symptoms resolve, but individual timelines vary.
Cautions and Limitations:
Practical Tips for Patients:
If you’re concerned about shedding spores, focus on infection control measures: wash hands with soap and water (not just sanitizer), disinfect surfaces with spore-killing agents (e.g., bleach solution), and avoid sharing personal items. For healthcare workers or those in high-risk settings, consult an infectious disease specialist to determine if testing is necessary.
Playing Spore Without an Account: What You Need to Know
You may want to see also
Frequently asked questions
Shedding of *C. difficile* spores can continue for several weeks to months after infection, even after symptoms resolve. Studies suggest shedding may persist for up to 6 weeks or longer in some cases.
Yes, you can still shed and potentially spread *C. difficile* spores after completing treatment, as the spores can remain in your stool for weeks or months.
There is no simple test to determine when shedding stops. It’s recommended to practice good hygiene, such as frequent handwashing, until at least 2 weeks after symptoms resolve, though shedding may continue longer.
A negative stool test indicates the bacteria or toxin is not detectable at that time, but it does not guarantee you’ve stopped shedding spores. Spores can persist even if the test is negative.