Candida, a genus of yeasts, commonly exists in the human body as part of the natural microbiota, particularly in the gastrointestinal tract, mouth, and genital areas. Its primary mode of reproduction is through budding, a process where a small daughter cell forms as an outgrowth from the parent cell and eventually detaches. While Candida does produce spores under certain environmental conditions, such as in response to stress or nutrient deprivation, this is not its primary method of reproduction inside the human body. Understanding whether Candida reproduces via budding or sporulation within the body is crucial for comprehending its role in health and disease, as well as for developing effective treatments for candidiasis, an infection caused by overgrowth of this fungus.
| Characteristics | Values |
|---|---|
| Form Inside Body | Candida primarily exists in its yeast (budding) form inside the human body. |
| Spore Formation | Candida does not typically form spores inside the human body; spore formation is more common in the environment. |
| Budding Process | Candida reproduces asexually through budding, where a small daughter cell forms on the parent cell and eventually detaches. |
| Environmental Spores | In the environment, some Candida species (e.g., Candida albicans) can form chlamydospores under specific conditions, but this is not relevant to its behavior inside the body. |
| Clinical Relevance | The yeast form is the primary concern in infections like candidiasis, as it adheres to tissues and can invade host cells. |
| Morphological Transition | Candida can switch between yeast and hyphal forms (a process called dimorphism), but spores are not part of this transition inside the body. |
| Immune Response | The immune system targets the yeast and hyphal forms, not spores, as spores are not typically present internally. |
| Treatment Focus | Antifungal treatments target the yeast and hyphal forms, as these are the active infectious agents inside the body. |
What You'll Learn
- Candida Reproduction Methods: Understanding how Candida reproduces inside the body, either through spores or budding
- Spore Formation in Candida: Investigating if Candida forms spores as a survival mechanism within the body
- Budding Process in Candida: Examining the budding process as the primary method of Candida replication in the body
- Environmental Factors Affecting Reproduction: How body conditions influence Candida's choice between spore formation and budding
- Clinical Implications of Reproduction: The impact of Candida's reproductive methods on diagnosis, treatment, and infection management

Candida Reproduction Methods: Understanding how Candida reproduces inside the body, either through spores or budding
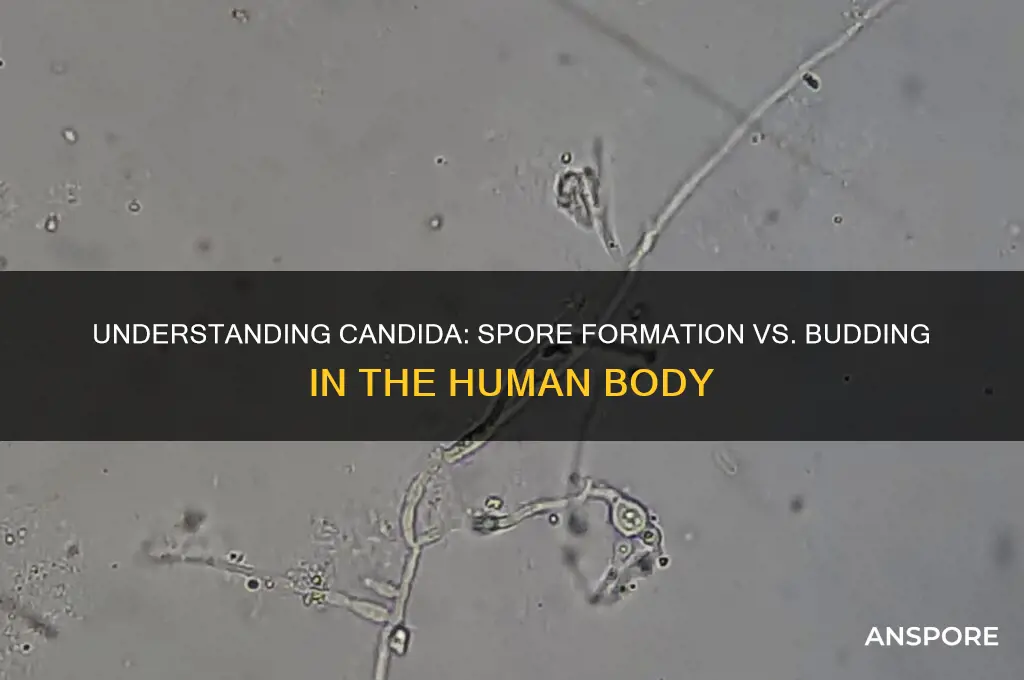
Candida, a genus of yeasts, is a common inhabitant of the human body, often residing in the gastrointestinal tract, mouth, and genital areas without causing harm. However, under certain conditions, it can overgrow, leading to infections such as candidiasis. Understanding how Candida reproduces inside the body is crucial for managing and preventing these infections. Candida primarily reproduces through a process called budding, where a small outgrowth (bud) forms on the parent cell, eventually detaching to become a new cell. This method allows Candida to multiply rapidly in favorable environments, such as warm, moist areas with ample nutrients. While Candida is not known to produce spores inside the human body, it can form spores under specific laboratory conditions, which are more resistant to harsh environments.
Budding is the predominant method of Candida reproduction in vivo, making it a key focus in clinical settings. During budding, the parent cell undergoes asymmetric division, creating a smaller daughter cell that remains attached until it matures. This process is highly efficient, enabling Candida to adapt quickly to changes in its environment, such as shifts in pH, temperature, or nutrient availability. For instance, in immunocompromised individuals or those with disrupted microbiota, Candida can exploit these conditions to proliferate unchecked, leading to systemic or localized infections. Understanding this mechanism is essential for developing antifungal treatments that target the budding process, such as echinocandins, which inhibit cell wall synthesis during budding.
While Candida does not typically form spores inside the human body, its ability to do so under certain conditions raises questions about its survival strategies. Spores, or chlamydospores, are thick-walled, dormant structures that can withstand extreme conditions, such as heat, dryness, and antifungal agents. These spores are more commonly observed in environmental settings, such as soil or decaying organic matter, where Candida exists outside the host. However, the potential for spore formation highlights Candida’s resilience and adaptability, underscoring the need for comprehensive treatment approaches that address both active and dormant forms. For example, combining antifungal medications with immune-boosting strategies may be more effective in eradicating persistent Candida infections.
Practical management of Candida overgrowth involves addressing the underlying conditions that promote its reproduction. For individuals prone to recurrent infections, maintaining a balanced diet low in sugars and refined carbohydrates can deprive Candida of its primary energy source. Probiotics, particularly strains like Lactobacillus acidophilus, can help restore a healthy gut microbiota, reducing the space and resources available for Candida to thrive. Additionally, antifungal medications such as fluconazole (typically prescribed at 150–300 mg orally for uncomplicated infections) can be used to target active Candida cells. However, long-term use of antifungals should be monitored to prevent resistance and disrupt the natural microbial balance.
In conclusion, Candida’s primary method of reproduction inside the body is budding, a rapid and efficient process that enables its proliferation in favorable conditions. While spore formation is not a concern in vivo, understanding Candida’s full reproductive capabilities is vital for effective management. By targeting budding through antifungal treatments, maintaining a healthy lifestyle, and supporting the immune system, individuals can mitigate the risk of Candida overgrowth and its associated complications. This knowledge empowers both healthcare providers and patients to adopt proactive strategies for preventing and treating candidiasis.
Mastering Big Spore Galactic Adventures: Creative Tips for Epic Expansions
You may want to see also

Spore Formation in Candida: Investigating if Candida forms spores as a survival mechanism within the body
Candida, a genus of yeasts, is commonly known for its role in human health, both as a commensal organism and a potential pathogen. While Candida primarily reproduces through budding, a process where a small daughter cell forms on the parent cell and eventually detaches, the question of whether it forms spores as a survival mechanism within the body remains a topic of scientific inquiry. Spores, typically associated with fungi, are highly resistant structures that enable survival in harsh conditions. However, Candida’s ability to form spores in the human body is not well-documented, prompting further investigation into its survival strategies.
To understand Candida’s survival mechanisms, it’s essential to distinguish between spore formation and other adaptive behaviors. Unlike fungi such as Aspergillus or Penicillium, Candida species like *Candida albicans* are not known to produce true spores. Instead, they rely on budding, biofilm formation, and phenotypic switching to adapt to changing environments. Biofilms, for instance, are complex communities of cells encased in a protective matrix that enhances resistance to antifungal agents and host immune responses. This raises the question: if Candida doesn’t form spores, how does it endure hostile conditions within the body?
One hypothesis is that Candida may adopt spore-like characteristics under extreme stress, though evidence remains inconclusive. Some studies suggest that certain Candida species can enter a quiescent state, reducing metabolic activity to withstand antifungal treatments or immune attacks. For example, *Candida albicans* can transition to a filamentous form, which may resemble a survival strategy akin to sporulation. However, this is not the same as true spore formation, which involves a distinct cellular restructuring not observed in Candida.
Clinically, understanding Candida’s survival mechanisms is crucial for managing infections, particularly in immunocompromised individuals. Antifungal treatments like fluconazole (typical dosage: 200–400 mg/day for adults) target actively replicating cells but may be less effective against dormant or biofilm-embedded Candida. Combining antifungals with biofilm-disrupting agents or immunomodulatory therapies could improve treatment outcomes. For instance, incorporating enzymes like DNase to degrade biofilm matrices or using echinocandins (e.g., caspofungin, 50–70 mg/day loading dose) to inhibit cell wall synthesis may enhance efficacy.
In conclusion, while Candida does not form spores as a survival mechanism within the body, its ability to adapt through budding, biofilm formation, and phenotypic switching underscores its resilience. Further research into these mechanisms could lead to targeted therapies that address Candida’s adaptive strategies, improving patient outcomes in both superficial and systemic infections. Practical tips for prevention include maintaining good hygiene, avoiding excessive antibiotic use, and monitoring blood glucose levels, as hyperglycemia can promote Candida overgrowth.
Unlocking Nano Sponsorships: A Step-by-Step Guide to Securing Micro-Deals
You may want to see also

Budding Process in Candida: Examining the budding process as the primary method of Candida replication in the body
Candida, a genus of yeasts, primarily replicates within the human body through a process known as budding. This asexual method of reproduction is both efficient and rapid, allowing Candida to thrive in various environments, including the gastrointestinal tract, oral cavity, and vaginal mucosa. Unlike spore formation, which is more commonly associated with fungi like Aspergillus or Penicillium, Candida’s budding process is its dominant mechanism for growth and dissemination. Understanding this process is crucial for managing candidiasis, as it highlights how quickly the organism can colonize and adapt within the host.
The budding process begins with the formation of a small outgrowth, or bud, on the parent cell. This bud gradually increases in size, developing its own nucleus and cellular components. Once the bud reaches maturity, it separates from the parent cell, becoming a new, independent cell. This cycle repeats continuously, enabling Candida populations to expand exponentially under favorable conditions. Factors such as warmth, moisture, and nutrient availability accelerate this process, which is why Candida often flourishes in mucosal tissues. For instance, in the oral cavity, the temperature and nutrient-rich environment of saliva provide ideal conditions for budding.
Clinically, the budding process has significant implications for treatment strategies. Antifungal medications like fluconazole (typically prescribed at 150–300 mg orally for vaginal candidiasis) target the cell wall and membrane synthesis, disrupting the budding cycle. However, Candida’s rapid replication can lead to drug resistance, particularly with prolonged or inappropriate use of antifungals. Patients with compromised immune systems, such as those with HIV/AIDS or undergoing chemotherapy, are at higher risk of recurrent infections due to the organism’s ability to bud unchecked. Monitoring Candida’s growth patterns and adjusting treatment accordingly is essential for effective management.
Comparatively, spore formation—a process where fungi produce dormant, resilient structures—is not a feature of Candida’s lifecycle inside the human body. While some fungi use spores to survive harsh conditions, Candida relies on its ability to bud continuously, adapting to the host environment rather than retreating into a dormant state. This distinction is critical for diagnosis and treatment, as it underscores the need to target active, replicating cells rather than dormant structures. For example, in cases of invasive candidiasis, early detection and intervention are vital to prevent systemic spread through budding.
In practical terms, individuals can reduce Candida overgrowth by maintaining a balanced environment in the body. This includes dietary modifications, such as reducing sugar intake (as Candida feeds on glucose), and promoting gut health through probiotics (e.g., Lactobacillus strains, typically taken at 10–20 billion CFUs daily). Good hygiene practices, particularly in areas prone to candidiasis like the mouth and genital region, can also limit the conditions conducive to budding. For recurrent infections, consulting a healthcare provider for tailored antifungal therapy and monitoring is essential to break the cycle of replication. By understanding and addressing the budding process, individuals can effectively manage Candida’s presence and prevent complications.
Do Cycads Have Spores? Unveiling Their Unique Reproduction Methods
You may want to see also

Environmental Factors Affecting Reproduction: How body conditions influence Candida's choice between spore formation and budding
Candida, a genus of yeasts, primarily reproduces through budding under favorable conditions, but it can also form spores when stressed. This reproductive duality is not random; it’s a response to environmental cues within the host body. Factors such as pH levels, nutrient availability, temperature, and immune system activity act as signals that Candida interprets to decide between these reproductive strategies. Understanding these triggers can shed light on how Candida adapts to survive and thrive in diverse bodily environments.
Consider the role of pH in Candida’s reproductive choices. The human body maintains different pH levels across tissues—blood is slightly alkaline (pH 7.35–7.45), while the gastrointestinal tract varies from acidic (stomach, pH 1.5–3.5) to neutral (small intestine, pH 6–7.4). Candida albicans, the most common species, favors budding in neutral to slightly acidic environments, such as the oral cavity (pH 6.7–7.3). However, in more acidic conditions, like the vagina (pH 3.8–4.5), Candida may shift toward spore formation as a protective mechanism. This adaptability allows it to withstand harsher environments and increase its chances of survival.
Nutrient availability is another critical factor. Candida thrives on simple sugars, which are abundant in the human gut. When glucose levels are high, Candida prioritizes budding, a rapid asexual reproduction method that allows it to quickly colonize an area. Conversely, in nutrient-depleted environments, such as during fasting or in certain immune responses, Candida may resort to spore formation. Spores are metabolically dormant and more resistant to stress, enabling Candida to persist until conditions improve. For instance, a diet low in refined sugars and high in fiber can reduce glucose availability, potentially discouraging budding and favoring spore formation.
The immune system’s role cannot be overlooked. Macrophages and neutrophils, key players in the immune response, can phagocytose Candida cells. In response, Candida may form spores, which are more resistant to immune cells’ killing mechanisms. Additionally, inflammatory cytokines released during an immune response can trigger stress pathways in Candida, promoting spore formation. For individuals with compromised immune systems, such as those on immunosuppressive medications or with HIV/AIDS, Candida may exploit the reduced immune pressure to bud unchecked, leading to overgrowth and infection.
Practical tips for managing Candida’s reproductive choices include maintaining a balanced pH through diet and hygiene. Probiotic-rich foods like yogurt can help stabilize vaginal and gut pH, discouraging spore formation. Reducing sugar intake limits the fuel Candida needs for budding, while antifungal supplements like caprylic acid or oregano oil can target both budding cells and spores. Monitoring environmental factors—such as pH, diet, and immune health—empowers individuals to influence Candida’s reproductive strategy, potentially reducing its pathogenic potential.
Neisseria Meningitidis: Understanding Its Structure and Sporulation Potential
You may want to see also

Clinical Implications of Reproduction: The impact of Candida's reproductive methods on diagnosis, treatment, and infection management
Candida's dual reproductive strategies—budding and, in some species, sporulation—significantly influence its clinical management. Budding, the primary method, allows rapid proliferation within host tissues, contributing to acute infections like thrush or invasive candidiasis. Sporulation, though less common in vivo, enables survival in harsh conditions, complicating eradication. Understanding these mechanisms is critical for tailoring diagnostic and therapeutic approaches to Candida infections.
Diagnostically, the distinction between budding and sporulation impacts detection methods. Microscopic examination of clinical samples often reveals yeast cells with budding daughter cells, confirming active infection. However, spores, if present, may evade standard culture techniques due to their dormant state. Advanced molecular diagnostics, such as PCR assays targeting Candida-specific genes, can improve detection rates, especially in cases where spores are suspected. For instance, in immunocompromised patients with recurrent infections, identifying sporulation could explain treatment resistance and guide more aggressive interventions.
Treatment strategies must account for Candida's reproductive adaptability. Antifungal agents like fluconazole (150–300 mg/day for adults) target actively replicating cells but may be less effective against spores. Echinocandins, such as caspofungin (70 mg loading dose followed by 50 mg/day), inhibit cell wall synthesis during budding, making them effective for acute infections. However, spores' dormant nature necessitates prolonged therapy or combination regimens to prevent relapse. For example, in invasive candidiasis, a 14-day course of echinocandins followed by oral fluconazole for maintenance can address both budding yeast and potential spores.
Infection management requires a proactive approach to mitigate Candida's reproductive advantages. In healthcare settings, strict hygiene protocols, including handwashing and disinfection of medical devices, reduce transmission of budding cells. For at-risk populations, such as neonates or diabetics, monitoring for early signs of infection (e.g., oral lesions or elevated serum biomarkers) allows prompt intervention. Additionally, dietary modifications, like reducing sugar intake to limit Candida's nutrient supply, can complement pharmacotherapy. For instance, probiotics containing Lactobacillus strains (10^9–10^10 CFU/day) may restore microbial balance and inhibit Candida overgrowth.
Comparatively, Candida's reproductive methods highlight the need for personalized treatment plans. While budding drives acute infections requiring immediate antifungal therapy, sporulation demands sustained management to prevent chronic or recurrent disease. Clinicians must consider patient factors—immunosuppression, comorbidities, and infection history—when selecting treatments. For example, in a 65-year-old diabetic with recurrent vulvovaginal candidiasis, a combination of topical clotrimazole (500 mg suppository nightly for 7 days) and systemic fluconazole (150 mg weekly for 6 months) could address both active budding and latent spores. This tailored approach maximizes efficacy while minimizing resistance and recurrence.
Mastering Spore's Complexity Mode: Tips to Expand Your Creations
You may want to see also
Frequently asked questions
Candida primarily reproduces by budding inside the body. It does not form spores as part of its normal life cycle in humans.
No, Candida species do not form spores in the human body. They reproduce asexually through budding, even in different environments within the body.
Budding is an asexual reproduction method where a new cell grows out of the parent cell, while spore formation is a method used by some fungi to survive harsh conditions, which Candida does not utilize.
Yes, Candida’s rapid budding process can contribute to its overgrowth, especially when the immune system is compromised or the balance of microorganisms in the body is disrupted.
No, none of the Candida species commonly found in humans, such as Candida albicans, form spores inside the body. They exclusively reproduce through budding.







