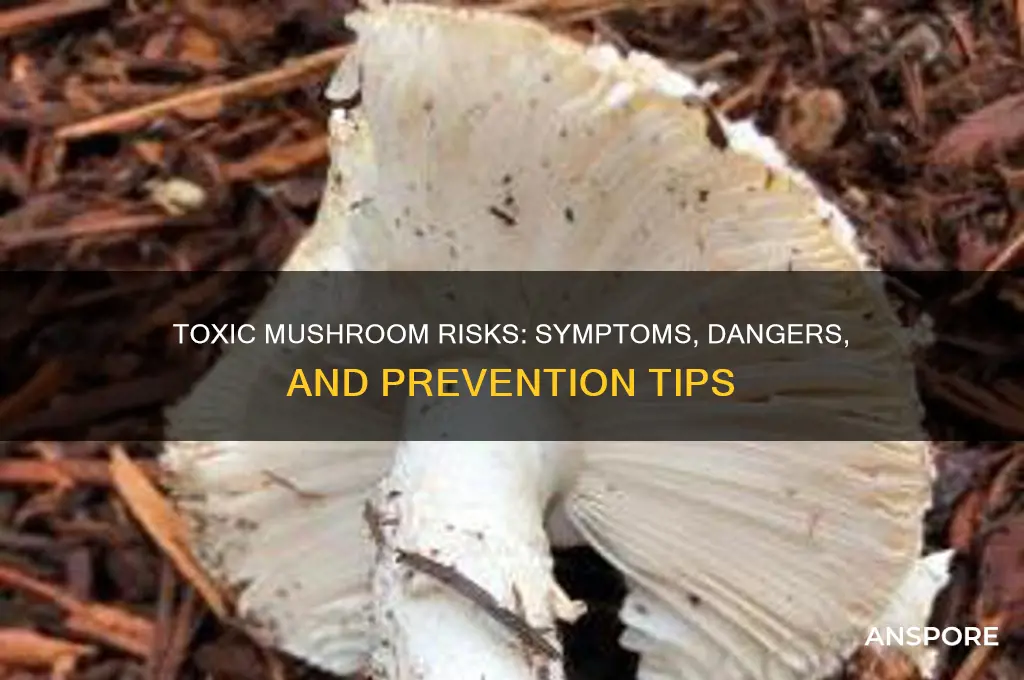
Consuming an unsafe mushroom can lead to severe health consequences, ranging from mild gastrointestinal discomfort to life-threatening conditions. Symptoms often include nausea, vomiting, diarrhea, and abdominal pain, but certain toxic species, like the Death Cap (*Amanita phalloides*), can cause liver and kidney failure, requiring immediate medical attention. Misidentification of mushrooms is a common risk, as many poisonous varieties resemble edible ones. Delayed treatment can result in organ damage, coma, or even death. Always consult a mycologist or use reliable guides before foraging, and when in doubt, avoid consumption entirely.
| Characteristics | Values |
|---|---|
| Gastrointestinal Symptoms | Nausea, vomiting, diarrhea, abdominal pain, and cramps (often within 6-24 hours of ingestion). |
| Neurological Effects | Hallucinations, confusion, seizures, muscle spasms, and altered mental state. |
| Liver Damage | Acute liver failure, jaundice, and elevated liver enzymes (common in Amanita species poisoning). |
| Kidney Damage | Acute kidney injury, reduced urine output, and electrolyte imbalances. |
| Cardiovascular Effects | Irregular heartbeat, low blood pressure, and cardiovascular collapse. |
| Respiratory Distress | Difficulty breathing, respiratory failure (rare but life-threatening). |
| Long-Term Effects | Chronic liver or kidney damage, neurological deficits, and increased risk of organ failure. |
| Fatality Risk | Death can occur within days, especially with highly toxic species like Amanita phalloides. |
| Onset of Symptoms | Varies by mushroom type: some cause symptoms within hours, others may take days. |
| Treatment | Gastric decontamination, activated charcoal, supportive care, and in severe cases, liver transplantation. |
| Prevention | Avoid consuming wild mushrooms unless identified by an expert mycologist. |
Explore related products
What You'll Learn
- Severe gastrointestinal distress: Nausea, vomiting, diarrhea, and abdominal pain can occur within hours of ingestion
- Organ damage: Toxic mushrooms can harm the liver, kidneys, or heart, leading to long-term issues
- Neurological symptoms: Hallucinations, confusion, seizures, or coma may result from certain mushroom toxins
- Allergic reactions: Rashes, swelling, or difficulty breathing can happen in sensitive individuals
- Fatal poisoning: Some mushrooms contain deadly toxins, causing multi-organ failure and death if untreated

Severe gastrointestinal distress: Nausea, vomiting, diarrhea, and abdominal pain can occur within hours of ingestion
The human body is remarkably efficient at signaling when something is amiss, and severe gastrointestinal distress is one of its most urgent alarms. Within hours of ingesting an unsafe mushroom, the digestive system can launch into a full-scale rebellion. Nausea often strikes first, a queasy foreboding that something toxic has entered the body. This is swiftly followed by vomiting, the body’s attempt to expel the offending substance. Diarrhea and abdominal pain soon join the chorus, as the intestines react to the toxin’s presence. This rapid onset is a hallmark of many poisonous mushrooms, such as those containing amatoxins (found in the *Amanita* genus), which can cause irreversible damage if not treated promptly.
Consider the case of a hiker who mistook a Death Cap (*Amanita phalloides*) for an edible button mushroom. Within 6–24 hours, they experienced intense nausea and vomiting, followed by severe abdominal cramps and watery diarrhea. These symptoms are not merely uncomfortable—they are a sign of liver and kidney damage in progress. The toxins in such mushrooms inhibit protein synthesis in cells, leading to organ failure if left untreated. For children, the elderly, or those with compromised immune systems, even a small amount (as little as 50 grams) can be life-threatening. Immediate medical attention, including activated charcoal administration and supportive care, is critical to mitigate the effects.
To avoid this scenario, always adhere to the rule: never consume a wild mushroom unless it has been positively identified by an expert. Even experienced foragers make mistakes, as many toxic species closely resemble edible ones. For instance, the Jack-O’-Lantern mushroom (*Omphalotus olearius*) glows in the dark and is often confused with chanterelles, but it causes severe gastrointestinal distress within 30 minutes to 4 hours of ingestion. If symptoms occur, note the time of ingestion, save any leftover mushroom material for identification, and seek emergency care immediately. Delaying treatment can turn a painful experience into a fatal one.
Practical prevention is key. Educate yourself on the common toxic mushrooms in your region, such as the Destroying Angel (*Amanita bisporigera*) in North America or the Fool’s Webcap (*Cortinarius orellanus*) in Europe. Carry a reliable field guide or use trusted apps like iNaturalist, but remember, technology is not infallible. If in doubt, throw it out. Foraging workshops led by mycologists can also sharpen your identification skills. In the kitchen, always cook wild mushrooms thoroughly, as some toxins are heat-sensitive. However, cooking does not neutralize all toxins, so proper identification remains paramount.
In conclusion, severe gastrointestinal distress is not merely a discomfort but a critical warning sign of potential organ damage. Understanding the timeline, symptoms, and risks associated with toxic mushrooms empowers individuals to act swiftly and responsibly. Whether you’re a forager, a curious hiker, or a home cook, prioritizing caution over curiosity can save lives. When it comes to mushrooms, the old adage holds true: better safe than sorry.
Whipping Cream in Mushroom Soup: A Creamy Substitute or Mistake?
You may want to see also

Organ damage: Toxic mushrooms can harm the liver, kidneys, or heart, leading to long-term issues
Toxic mushrooms contain potent toxins that can inflict severe, sometimes irreversible damage to vital organs. Among the most notorious are amanitin-containing species like the Death Cap (*Amanita phalloidis*), which disrupt cellular function and lead to acute liver failure within 24–48 hours of ingestion. Even a single bite—as little as 30 grams—can be fatal without immediate medical intervention. The liver, responsible for detoxifying the body, becomes overwhelmed, leading to symptoms like jaundice, abdominal pain, and, in severe cases, hepatic necrosis. This underscores the critical importance of accurate identification before consuming wild mushrooms.
The kidneys, too, are vulnerable to mushroom toxins, particularly those found in species like the Fool’s Webcap (*Cortinarius orellanus*). Orellanine, the toxin in these mushrooms, causes delayed renal failure, often manifesting 3–14 days after ingestion. Symptoms include dark urine, fatigue, and swelling, as the kidneys lose their ability to filter waste. Unlike liver damage, which can sometimes be managed with transplants or antidotes like silibinin, kidney damage from these toxins is often permanent, requiring lifelong dialysis or transplantation. This highlights the need for awareness, especially among foragers who mistake toxic species for edible ones.
Cardiac complications, though less common, are equally alarming. Mushrooms like the Yellow Stainers (*Agaricus xanthodermus*) contain toxins that can induce tachycardia, hypotension, and arrhythmias, particularly in children or individuals with pre-existing heart conditions. While these effects are typically transient, repeated exposure or large doses can exacerbate underlying cardiac issues. For instance, a 2019 case study reported a 52-year-old man experiencing severe bradycardia after consuming misidentified mushrooms, requiring emergency pacemaker implantation. Such incidents emphasize the importance of seeking medical attention immediately if mushroom poisoning is suspected.
Preventing organ damage from toxic mushrooms begins with education and caution. Always consult a mycologist or use a reputable field guide when foraging, and avoid consuming mushrooms unless 100% certain of their identity. Cooking does not neutralize most mushroom toxins, so visual inspection alone is insufficient. If ingestion occurs, note the mushroom’s appearance and contact a poison control center or hospital immediately. Early treatment—such as activated charcoal to reduce toxin absorption or specific antidotes like N-acetylcysteine for amanitin poisoning—can mitigate damage. Remember: when in doubt, throw it out. The risks far outweigh the curiosity.
Cream of Mushroom Substitutes: Healthy and Tasty Alternatives for Your Recipes
You may want to see also

Neurological symptoms: Hallucinations, confusion, seizures, or coma may result from certain mushroom toxins
Mushroom toxins can wreak havoc on the nervous system, triggering a cascade of neurological symptoms that range from disorienting to life-threatening. Among the most notorious are those caused by psilocybin-containing mushrooms, often sought for their hallucinogenic effects. However, even a slight misidentification can lead to ingestion of toxic species like *Amanita muscaria* or *Conocybe filaris*, which produce similar hallucinations but with dangerous side effects. These toxins interfere with neurotransmitter function, leading to altered perception, vivid hallucinations, and profound confusion. Unlike controlled doses in medical settings, wild mushrooms deliver unpredictable amounts, increasing the risk of severe reactions.
The onset of neurological symptoms can be rapid, often within 30 minutes to 2 hours after ingestion, depending on the toxin and dosage. Confusion and disorientation are typically the first signs, as the brain struggles to process sensory information. Seizures may follow, particularly in children or individuals with lower body mass, as their systems are more susceptible to toxin overload. For instance, amatoxins found in *Amanita phalloides* (Death Cap) initially cause gastrointestinal distress but can progress to seizures and coma within 24–48 hours due to liver failure and subsequent encephalopathy. Immediate medical intervention is critical, as delays can lead to irreversible brain damage.
Hallucinations induced by mushroom toxins differ from those caused by synthetic drugs, often described as more intense and uncontrollable. Users report distorted time perception, visual and auditory distortions, and a loss of self-awareness. While some may find these experiences intriguing, they are inherently risky due to the lack of control over the toxin’s effects. For instance, a single *Amanita muscaria* cap contains enough muscimol to induce hallucinations, but consuming two or more can lead to respiratory depression and coma. This fine line between a "trip" and a medical emergency underscores the danger of self-experimentation with wild mushrooms.
Preventing neurological complications begins with accurate identification and avoidance of toxic species. Foraging without expert guidance is strongly discouraged, as even experienced collectors occasionally make fatal mistakes. If ingestion occurs, immediate steps include inducing vomiting (if advised by poison control) and seeking emergency care. Hospitals may administer activated charcoal to limit toxin absorption or provide benzodiazepines to control seizures. Long-term recovery depends on prompt treatment, with survivors of severe poisoning often requiring months of rehabilitation to address cognitive and motor deficits. When it comes to mushrooms, the adage holds true: better safe than sorry.
Enhance Your Psilocybe Mushroom Journey: Foods and Substances to Explore
You may want to see also
Explore related products

Allergic reactions: Rashes, swelling, or difficulty breathing can happen in sensitive individuals
Even a tiny bite of the wrong mushroom can trigger a full-blown allergic reaction in susceptible individuals. Unlike the gradual onset of poisoning symptoms, allergic reactions are swift and often intense. Within minutes to hours of ingestion, the body's immune system, mistaking mushroom proteins as harmful invaders, launches a defensive attack. This overreaction manifests as a spectrum of symptoms, ranging from mild skin irritations to life-threatening anaphylaxis.
Understanding these reactions is crucial, as they can mimic other mushroom-related illnesses, leading to misdiagnosis and delayed treatment.
Imagine a scenario: a forager, confident in their identification skills, consumes a mushroom they believe to be safe. Shortly after, they experience itching, hives, and swelling around the mouth and face. This is a classic example of an IgE-mediated allergic reaction, where the body produces antibodies against specific mushroom allergens. These antibodies trigger the release of histamine, a chemical responsible for the characteristic itching, redness, and swelling. While uncomfortable, these symptoms are usually manageable with antihistamines. However, in severe cases, the reaction can progress to anaphylaxis, a medical emergency characterized by difficulty breathing, a drop in blood pressure, and loss of consciousness.
Prompt administration of epinephrine (adrenaline) is crucial in such situations.
It's important to note that allergic reactions to mushrooms are not solely dependent on the species consumed. Individual sensitivity plays a significant role. Some people may react to even trace amounts of certain mushrooms, while others can consume larger quantities without issue. Factors like age, overall health, and previous exposure to allergens can influence susceptibility. Children, for instance, are more prone to developing allergies due to their developing immune systems.
Prevention is key when it comes to mushroom allergies. For those with known sensitivities, strict avoidance is essential. This includes not only wild mushrooms but also cultivated varieties, as cross-reactivity between species is common. Reading food labels carefully and inquiring about ingredients when dining out are crucial practices. Carrying an epinephrine auto-injector (e.g., EpiPen) is a lifesaving measure for individuals at risk of anaphylaxis.
Finally, if any allergic symptoms occur after consuming mushrooms, seeking immediate medical attention is paramount.
Mixing Psychedelics: Risks of Combining Acid and Mushrooms Explained
You may want to see also

Fatal poisoning: Some mushrooms contain deadly toxins, causing multi-organ failure and death if untreated
Mushrooms, often celebrated for their culinary versatility, harbor a darker side: some species contain toxins potent enough to cause fatal poisoning. Among the most notorious are the Death Cap (*Amanita phalloides*) and the Destroying Angel (*Amanita bisporigera*), which produce amatoxins—deadly compounds that evade detection by taste or smell. Ingesting even a small portion, roughly 50 grams of a Death Cap, can lead to severe toxicity in adults. Children are at higher risk due to their lower body weight, with as little as 20 grams proving lethal. These toxins are heat-stable, meaning cooking does not neutralize their danger, making misidentification a potentially fatal mistake.
The insidious nature of amatoxin poisoning lies in its delayed onset. Symptoms may not appear for 6 to 24 hours after ingestion, lulling victims into a false sense of security. Initial signs include gastrointestinal distress—vomiting, diarrhea, and abdominal pain—which can be mistaken for food poisoning. However, within 24 to 72 hours, the toxins wreak havoc on internal organs, primarily the liver and kidneys. This leads to multi-organ failure, characterized by jaundice, seizures, and coma. Without immediate medical intervention, the mortality rate exceeds 50%, even in otherwise healthy individuals.
Treatment for amatoxin poisoning is a race against time. Gastric lavage (stomach pumping) and activated charcoal may be administered to reduce toxin absorption, but their effectiveness diminishes as hours pass. Intravenous fluids and medications like silibinin, an antidote derived from milk thistle, can slow liver damage. In severe cases, a liver transplant may be the only lifesaving option. However, access to such interventions is limited, and the window for successful treatment is narrow. Prevention, therefore, is paramount: never consume wild mushrooms unless identified by a certified mycologist.
The risk of fatal mushroom poisoning underscores the importance of education and caution. Foraging without expertise is akin to playing Russian roulette with nature. Even experienced foragers occasionally misidentify species, as many toxic mushrooms resemble edible varieties. For instance, the Death Cap closely mimics the Paddy Straw mushroom (*Volvariella volvacea*), a popular edible species. Carrying a field guide, using spore print tests, and cross-referencing multiple identification features can reduce risk, but absolute certainty requires laboratory analysis. When in doubt, throw it out—a simple rule that could save a life.
In a world where wild harvesting is increasingly popular, the dangers of toxic mushrooms cannot be overstated. Fatal poisoning is not a theoretical risk but a documented reality, with cases reported globally each year. Awareness campaigns and accessible resources, such as poison control hotlines, play a critical role in mitigating this threat. Ultimately, the allure of foraging must be balanced with respect for the potential consequences. No meal is worth risking multi-organ failure or death—a stark reminder that nature’s bounty demands both curiosity and caution.
Can You Smoke Mushrooms? Exploring the Risks and Realities
You may want to see also
Frequently asked questions
Immediate symptoms can include nausea, vomiting, diarrhea, abdominal pain, and cramps, often appearing within 20 minutes to 4 hours after ingestion.
Yes, certain toxic mushrooms, like the Death Cap (Amanita phalloides), contain potent toxins that can cause liver and kidney failure, leading to death if not treated promptly.
Unsafe mushrooms can be either poisonous or psychoactive. Poisonous mushrooms cause physical harm, while psychoactive mushrooms (like Psilocybin mushrooms) induce hallucinations but are generally not life-threatening.
Seek medical help immediately, even if symptoms are mild or haven’t appeared yet. Delayed treatment can lead to severe complications or organ damage.
No, cooking or boiling does not neutralize most mushroom toxins. Toxic mushrooms remain dangerous regardless of preparation methods. Always avoid consuming unidentified mushrooms.