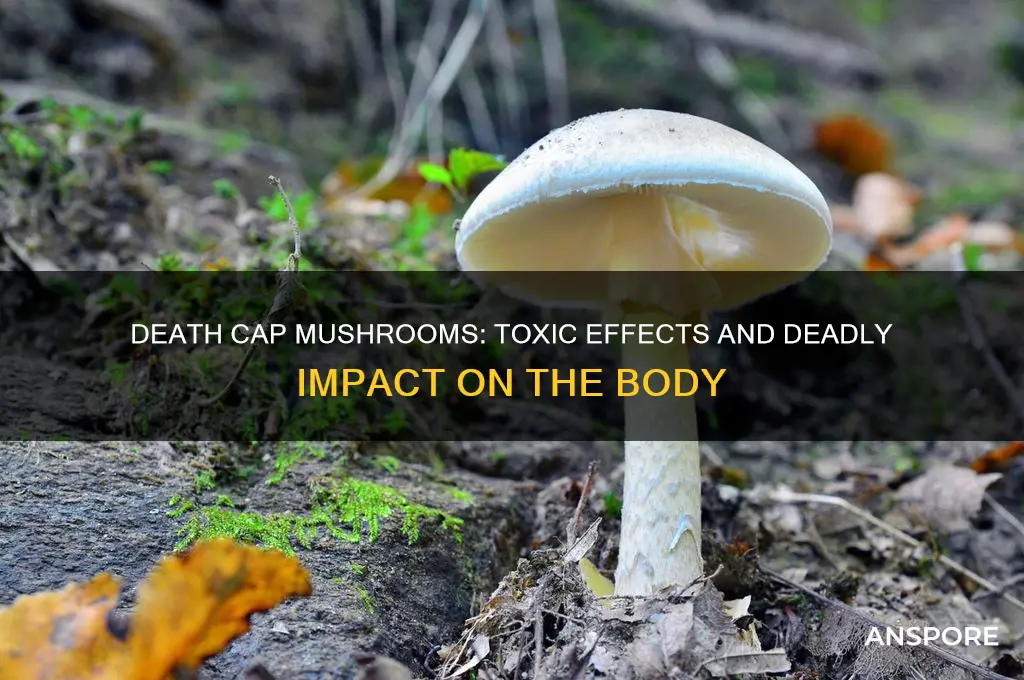
The death cap mushroom, scientifically known as *Amanita phalloides*, is one of the most poisonous fungi in the world, responsible for the majority of fatal mushroom poisonings globally. When ingested, its toxins, primarily amatoxins, silently wreak havoc on the body, often with a delayed onset of symptoms that can initially mimic food poisoning. Within 6 to 24 hours, severe gastrointestinal distress, including vomiting, diarrhea, and abdominal pain, occurs as the toxins begin to destroy liver and kidney cells. If left untreated, the damage progresses to acute liver and kidney failure, leading to symptoms like jaundice, confusion, seizures, and eventually coma. Despite its innocuous appearance, the death cap’s potent toxins can be life-threatening, making prompt medical intervention, including liver transplantation in severe cases, crucial for survival.
| Characteristics | Values |
|---|---|
| Toxic Compounds | Amatoxins (e.g., alpha-amanitin, beta-amanitin) |
| Initial Symptoms | Delayed onset (6–24 hours); gastrointestinal distress (vomiting, diarrhea, abdominal pain) |
| Liver Damage | Severe hepatotoxicity; destruction of liver cells (hepatocytes) |
| Kidney Damage | Potential nephrotoxicity in severe cases |
| Symptom Progression | Initial recovery phase (24–72 hours), followed by rapid deterioration (liver failure, coagulopathy, encephalopathy) |
| Fatality Rate | 10–50% without treatment; higher without liver transplant |
| Treatment | Supportive care, activated charcoal, silibinin (milk thistle extract), liver transplant in severe cases |
| Long-term Effects | Chronic liver damage or failure in survivors; potential need for lifelong monitoring |
| Misidentification Risk | Often mistaken for edible mushrooms (e.g., straw mushrooms, puffballs) |
| Geographic Distribution | Worldwide, commonly found in Europe, North America, and Australia |
| Seasonal Occurrence | Typically appears in summer and autumn |
Explore related products
What You'll Learn
- Rapid Onset Symptoms: Nausea, vomiting, diarrhea, and abdominal pain begin 6-24 hours after ingestion
- Liver Damage: Toxins destroy liver cells, leading to acute liver failure within 2-3 days
- Kidney Failure: Toxins also damage kidneys, causing acute kidney injury and electrolyte imbalances
- Neurological Effects: Confusion, seizures, and coma may occur due to toxin-induced brain dysfunction
- Fatal Outcome: Without treatment, death cap poisoning is often fatal within 5-7 days

Rapid Onset Symptoms: Nausea, vomiting, diarrhea, and abdominal pain begin 6-24 hours after ingestion
The rapid onset symptoms following ingestion of death cap mushrooms (*Amanita phalloid*) are a critical indicator of poisoning and require immediate attention. Within 6 to 24 hours after consumption, the body begins to exhibit severe gastrointestinal distress as the toxins, primarily alpha-amanitin, start to take effect. The first symptom is often nausea, an overwhelming sensation of discomfort in the stomach that signals the body’s attempt to expel the toxin. This is quickly followed by vomiting, which can be persistent and forceful, leading to dehydration and electrolyte imbalances if not managed promptly. These symptoms are the body’s initial defense mechanisms, but they also mark the beginning of a dangerous progression.
As the toxins continue to circulate, diarrhea develops, often severe and watery, further contributing to fluid loss and electrolyte depletion. This symptom is not merely uncomfortable but can rapidly lead to dehydration, which exacerbates the body’s stress and complicates recovery. The combination of vomiting and diarrhea can leave the individual weak, dizzy, and unable to retain fluids, making it crucial to seek medical intervention immediately. Ignoring these symptoms or delaying treatment can lead to life-threatening complications.
Abdominal pain is another hallmark of this phase, often described as intense and cramp-like, radiating throughout the stomach area. This pain is caused by the toxin’s direct damage to the liver and gastrointestinal tract, as alpha-amanitin begins to disrupt cellular function and cause tissue necrosis. The pain may be constant or come in waves, making it difficult for the individual to find relief. It is a clear sign that the toxin is actively harming vital organs, and the severity of the pain often correlates with the amount of mushroom ingested.
These rapid onset symptoms are not just uncomfortable—they are a warning that the body is under attack. The gastrointestinal distress is the first visible manifestation of the toxin’s systemic effects, which will soon progress to more severe organ damage if untreated. It is imperative to recognize these symptoms early and seek emergency medical care, as prompt treatment can significantly improve the chances of survival. Delaying action during this phase can lead to irreversible damage and increase the risk of fatal outcomes.
Exploring the Intriguing World of Psychedelic Mushrooms
You may want to see also

Liver Damage: Toxins destroy liver cells, leading to acute liver failure within 2-3 days
The death cap mushroom, scientifically known as *Amanita phalloides*, contains potent toxins that wreak havoc on the human body, with the liver being one of the primary targets. The toxins responsible for liver damage are primarily amatoxins, which are cyclic octapeptides that are highly resistant to digestion and heat. Once ingested, these toxins are rapidly absorbed into the bloodstream and transported to the liver, where they exert their destructive effects. Amatoxins specifically target liver cells, binding to RNA polymerase II, an enzyme crucial for protein synthesis. This binding disrupts cellular function, leading to the rapid breakdown of liver cells.
Within hours of ingestion, the toxins begin to destroy hepatocytes, the primary functional cells of the liver. This cellular destruction triggers a cascade of events, including inflammation and the release of enzymes into the bloodstream. As more liver cells are damaged, the organ’s ability to perform essential functions—such as detoxifying the blood, metabolizing nutrients, and producing bile—becomes severely compromised. The initial symptoms of liver damage, such as nausea, vomiting, and abdominal pain, often appear 6 to 24 hours after consumption, misleadingly resembling a stomach bug. However, these symptoms are a precursor to the more severe consequences of toxin exposure.
As the toxins continue to ravage the liver, the damage progresses to acute liver failure, typically within 2 to 3 days of ingestion. Acute liver failure is a life-threatening condition characterized by the rapid loss of liver function. Symptoms at this stage include jaundice (yellowing of the skin and eyes), confusion, and coagulation disorders due to the liver’s inability to produce clotting factors. The liver’s role in filtering toxins from the blood is also severely impaired, allowing harmful substances to accumulate in the body. Without immediate medical intervention, such as a liver transplant or supportive care, acute liver failure caused by death cap mushroom poisoning is often fatal.
The severity of liver damage depends on the amount of toxin ingested and the timing of treatment. Even small quantities of the death cap mushroom can be deadly, as amatoxins are extremely potent. Early intervention, including gastric decontamination, administration of activated charcoal, and supportive care, can mitigate some of the damage. However, the toxins’ rapid onset and the liver’s limited regenerative capacity in the acute phase make this poisoning particularly dangerous. Monitoring liver enzymes, such as alanine transaminase (ALT) and aspartate transaminase (AST), is crucial in assessing the extent of liver damage and guiding treatment.
In summary, the toxins in death cap mushrooms directly and rapidly destroy liver cells, leading to acute liver failure within 2 to 3 days of ingestion. This process is characterized by the disruption of cellular function, inflammation, and the loss of essential liver functions. The progression from initial symptoms to life-threatening liver failure is swift, underscoring the importance of immediate medical attention in suspected cases of death cap mushroom poisoning. Awareness of these dangers and prompt action are critical to preventing fatal outcomes.
Psilocybin Mushroom Therapy: A Natural Treatment Option
You may want to see also

Kidney Failure: Toxins also damage kidneys, causing acute kidney injury and electrolyte imbalances
The death cap mushroom, scientifically known as *Amanita phalloides*, contains potent toxins that wreak havoc on the human body, with one of the most severe consequences being kidney failure. The primary toxins responsible for this damage are amatoxins, which are cyclic octapeptides that the body readily absorbs after ingestion. Once in the bloodstream, these toxins target vital organs, including the kidneys, leading to acute kidney injury (AKI). Amatoxins directly damage the renal tubular cells, which are essential for filtering waste and maintaining fluid balance. This cellular destruction disrupts the kidneys' ability to function properly, causing a rapid decline in kidney performance.
Acute kidney injury resulting from death cap mushroom poisoning is a life-threatening condition that manifests within 24 to 72 hours after ingestion. Symptoms of kidney failure include decreased urine output, swelling in the legs or face due to fluid retention, and fatigue. As the kidneys fail, waste products and toxins accumulate in the bloodstream, leading to a condition called azotemia. This buildup of toxins further exacerbates the damage to other organs, creating a dangerous cycle of systemic failure. Without prompt medical intervention, AKI can progress to chronic kidney disease or complete kidney failure, requiring dialysis or a kidney transplant.
Electrolyte imbalances are another critical consequence of kidney damage caused by death cap mushroom toxins. The kidneys play a crucial role in regulating electrolytes such as sodium, potassium, and calcium. When the kidneys are compromised, they cannot maintain the delicate balance of these essential minerals. Hyperkalemia (elevated potassium levels) is a common complication, which can lead to dangerous heart rhythm abnormalities, muscle weakness, and even cardiac arrest. Similarly, imbalances in sodium and calcium levels can cause neurological symptoms, seizures, and further organ dysfunction. These electrolyte disturbances compound the toxicity of amatoxins, making the condition even more severe.
Treatment for kidney failure induced by death cap mushroom poisoning is multifaceted and time-sensitive. Immediate medical attention is crucial, often involving gastric decontamination to remove any remaining toxins from the stomach. Intravenous fluids are administered to support kidney function and flush out toxins, while medications may be used to stabilize electrolyte imbalances. In severe cases, continuous renal replacement therapy (CRRT), a form of dialysis, may be necessary to temporarily take over the kidneys' function. Additionally, silibinin, an antidote derived from milk thistle, has shown promise in reducing the absorption of amatoxins and mitigating kidney damage when administered early.
Prevention remains the most effective strategy to avoid the devastating effects of death cap mushroom poisoning. Proper identification of mushrooms before consumption is critical, as death caps closely resemble edible species. Public education and awareness campaigns can help reduce accidental ingestion. For those who suspect poisoning, seeking medical help immediately—even before symptoms appear—can significantly improve outcomes. Understanding the mechanisms by which death cap toxins cause kidney failure underscores the importance of swift action and highlights the deadly potential of this seemingly innocuous fungus.
The Size of Coral Mushrooms: How Big Do They Grow?
You may want to see also
Explore related products

Neurological Effects: Confusion, seizures, and coma may occur due to toxin-induced brain dysfunction
The neurological effects of death cap mushroom (Amanita phalloides) poisoning are among the most alarming and life-threatening consequences of ingestion. These effects stem from the potent toxins present in the mushroom, primarily amatoxins, which disrupt cellular function and target vital organs, including the brain. Within 6 to 24 hours after consumption, individuals may begin to experience confusion, a hallmark of toxin-induced brain dysfunction. This confusion arises as amatoxins cross the blood-brain barrier, interfering with neuronal activity and impairing cognitive processes. The brain’s ability to regulate thought, memory, and awareness becomes compromised, leading to disorientation, difficulty concentrating, and altered mental states.
As the toxins continue to wreak havoc on the brain, more severe neurological symptoms can emerge, including seizures. Amatoxins disrupt the delicate balance of electrolytes and neurotransmitters in the brain, leading to abnormal electrical activity. This abnormal activity manifests as seizures, which can range from mild twitching to full-body convulsions. Seizures are a critical indicator of severe poisoning and require immediate medical intervention to prevent further brain damage or complications. The occurrence of seizures underscores the profound impact of death cap toxins on the central nervous system and highlights the urgency of treatment.
In the most severe cases of death cap mushroom poisoning, toxin-induced brain dysfunction can progress to a coma. As amatoxins continue to damage brain cells and disrupt metabolic processes, the brain’s ability to maintain consciousness is lost. A coma is a state of profound unconsciousness from which the individual cannot be awakened, and it signifies critical failure of brain function. This condition is often accompanied by other systemic failures, such as liver and kidney damage, further complicating the prognosis. The onset of a coma is a medical emergency and demands intensive care, including life support measures, to sustain vital functions.
The neurological effects of death cap mushroom poisoning are not only rapid but also insidious, often worsening despite the initial improvement in gastrointestinal symptoms. This is because amatoxins have a delayed but devastating impact on the brain, even as the body appears to recover from early symptoms like nausea and diarrhea. The progression from confusion to seizures and potentially coma underscores the importance of early diagnosis and treatment. Without prompt medical intervention, including supportive care and, in some cases, liver transplantation, the neurological damage caused by death cap toxins can be irreversible, leading to long-term cognitive impairment or death.
Preventing death cap mushroom poisoning is crucial, as the neurological effects are both severe and challenging to treat. Education about proper mushroom identification and avoidance of wild mushroom consumption is essential, especially in regions where death caps are prevalent. If ingestion is suspected, immediate medical attention is critical, even if symptoms seem mild. Early administration of activated charcoal, intravenous fluids, and medications to protect the liver can mitigate the toxin’s effects and reduce the risk of neurological complications. Awareness and swift action are key to preventing the devastating neurological consequences of death cap mushroom poisoning.
Mellow Mushroom Bread: Is It Dairy-Free?
You may want to see also

Fatal Outcome: Without treatment, death cap poisoning is often fatal within 5-7 days
The death cap mushroom, scientifically known as *Amanita phalloides*, is one of the most poisonous fungi in the world. Its toxins, primarily alpha-amanitin, target the liver and kidneys, leading to severe organ damage. Without treatment, death cap poisoning is often fatal within 5-7 days, making it a medical emergency that requires immediate attention. The toxin disrupts cellular RNA synthesis, causing irreversible harm to vital organs. This rapid progression underscores the importance of recognizing symptoms early and seeking medical intervention.
The initial symptoms of death cap poisoning, such as nausea, vomiting, and diarrhea, often appear 6-24 hours after ingestion, leading many to mistake it for a harmless stomach bug. However, this phase is deceptive, as the toxin continues to wreak havoc internally. By the time symptoms like jaundice, abdominal pain, and confusion manifest, typically 2-3 days after ingestion, the liver and kidneys are already severely compromised. Without treatment, this stage marks the beginning of the final decline, as organ failure sets in, often leading to death within 5-7 days.
The alpha-amanitin toxin is particularly insidious because it is not broken down by the body and continues to cause damage over several days. As liver function deteriorates, toxins accumulate in the bloodstream, leading to hepatic encephalopathy—a condition where the brain is affected by liver failure. This results in symptoms like disorientation, seizures, and coma. Without intervention, these neurological symptoms progress rapidly, contributing to the fatal outcome within the 5-7 day timeframe. The kidneys, too, fail due to toxin-induced damage, further accelerating the body's shutdown.
Treatment for death cap poisoning includes gastric decontamination, activated charcoal, and supportive care, but the most critical intervention is often a liver transplant in severe cases. However, without access to such treatment, the prognosis is grim. The body's inability to recover from the toxin's effects means that multiple organ failure becomes inevitable. Dehydration, electrolyte imbalances, and septic shock can also occur, compounding the risk of death. The swift and relentless nature of death cap poisoning highlights why prevention—avoiding misidentification of mushrooms—is paramount.
In summary, the death cap mushroom's toxins inflict catastrophic damage to the liver and kidneys, leading to a cascade of organ failure. Without treatment, the timeline from ingestion to death is alarmingly short, typically 5-7 days. Early symptoms may seem benign, but they mask the internal destruction caused by alpha-amanitin. As the body's vital organs cease to function, the outcome is almost always fatal. This underscores the critical need for public awareness about the dangers of wild mushroom consumption and the importance of prompt medical care in suspected poisoning cases.
Beef Stroganoff: Does It Include Mushrooms?
You may want to see also
Frequently asked questions
Initial symptoms typically appear 6–24 hours after ingestion and include severe abdominal pain, vomiting, diarrhea, and dehydration. These symptoms may falsely suggest a simple stomach bug, but they are the first signs of the mushroom's toxic effects on the body.
The death cap mushroom contains toxins like amatoxins, which destroy liver and kidney cells. Amatoxins inhibit RNA polymerase II, a crucial enzyme for protein synthesis, leading to organ failure. Without prompt medical intervention, this can result in coma, multi-organ failure, and death within days.
Treatment includes gastric decontamination, activated charcoal, and supportive care like IV fluids and medications. In severe cases, a liver transplant may be necessary. Survival depends on the amount ingested and how quickly treatment begins. With early intervention, survival rates are around 70–90%, but delays significantly worsen the prognosis.