Resting spores, often produced by certain bacteria and fungi as a survival mechanism in harsh environmental conditions, are generally not considered infectious in their dormant state. These spores are metabolically inactive and highly resistant to adverse conditions such as desiccation, extreme temperatures, and chemicals. While they can persist in the environment for extended periods, they typically do not pose an immediate infection risk unless they germinate and revert to their active, vegetative form. However, under favorable conditions, resting spores can reactivate, potentially leading to infection if they are pathogenic. Understanding the distinction between their dormant and active states is crucial for assessing their role in disease transmission and implementing effective control measures.
| Characteristics | Values |
|---|---|
| Infectiousness | Resting spores themselves are generally not infectious. They are a dormant, resilient form of certain bacteria (e.g., Clostridioides difficile) and fungi, designed for survival in harsh conditions, not for immediate infection. |
| Activation | Resting spores become infectious only after germination, which requires specific environmental triggers (e.g., warmth, moisture, nutrients). |
| Disease Transmission | Once germinated, the resulting active bacteria or fungi can cause infection if they enter a susceptible host. |
| Survival | Resting spores can survive for extended periods (years to decades) in adverse conditions (e.g., heat, desiccation, chemicals). |
| Examples | Clostridioides difficile (causes antibiotic-associated diarrhea), Bacillus anthracis (causes anthrax), fungal spores (e.g., Aspergillus). |
| Public Health Concern | Resting spores are a concern in healthcare settings due to their persistence on surfaces and resistance to disinfection. |
| Prevention | Effective cleaning, disinfection, and infection control practices are crucial to prevent spore germination and infection. |
Explore related products
What You'll Learn

Resting spore definition and characteristics
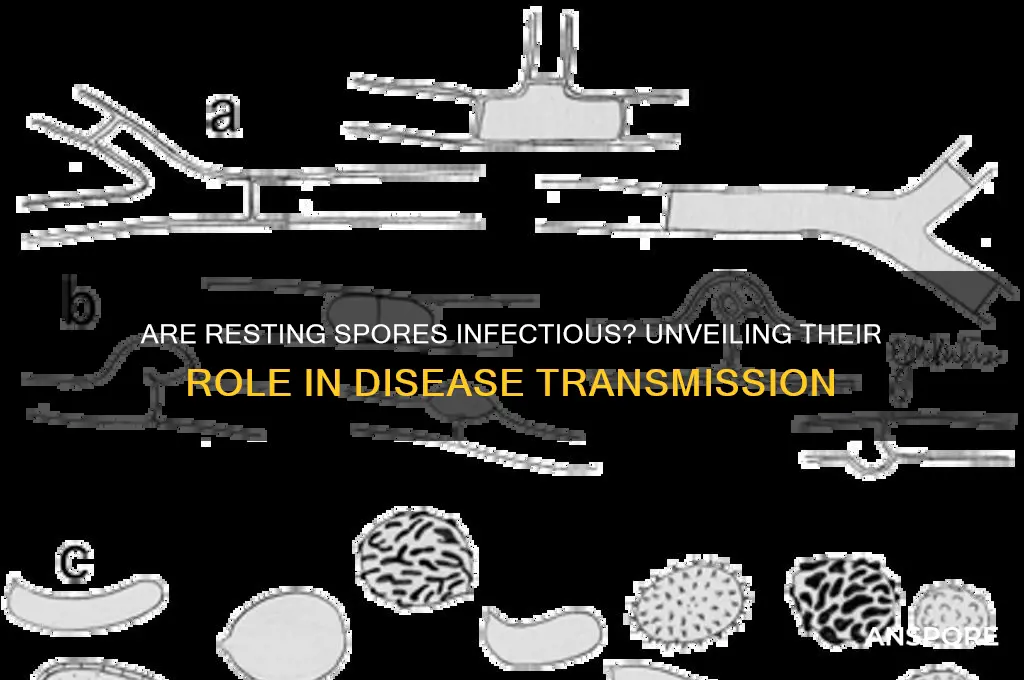
Resting spores are a survival mechanism employed by certain bacteria and fungi, allowing them to endure harsh environmental conditions. Unlike their active counterparts, these spores are metabolically dormant, ceasing most cellular processes to conserve energy. This dormancy is triggered by stressors such as nutrient depletion, extreme temperatures, or desiccation. For instance, *Bacillus anthracis*, the bacterium causing anthrax, forms resting spores that can persist in soil for decades, awaiting favorable conditions to reactivate.
Understanding the characteristics of resting spores is crucial for assessing their infectious potential. These spores are highly resistant to physical and chemical agents, including heat, radiation, and disinfectants, due to their thick, protective outer layers. This resilience enables them to survive in diverse environments, from hospital surfaces to natural soil. However, their dormant state means they are not actively infectious until they germinate. Germination requires specific triggers, such as warmth, moisture, and nutrients, which signal the spore to resume metabolic activity and revert to its vegetative form.
From a practical standpoint, preventing the germination of resting spores is key to managing their infectious risk. For example, in healthcare settings, thorough cleaning with spore-specific disinfectants like hydrogen peroxide or chlorine-based solutions is essential. In agricultural contexts, crop rotation and soil treatment can reduce the presence of fungal resting spores, such as those of *Claviceps purpurea*, which causes ergot disease in grains. Additionally, public health measures, like proper waste disposal and water treatment, can limit the spread of spore-forming pathogens like *Clostridium difficile*.
Comparatively, resting spores differ from other microbial survival forms, such as cysts or biofilms, in their level of dormancy and resistance. While cysts remain metabolically active at a low level, resting spores are completely dormant, making them more resilient but less immediately hazardous. Biofilms, on the other hand, provide a protective matrix for active cells, whereas spores are solitary structures. This distinction highlights why resting spores are often associated with latent infections, such as tetanus from *Clostridium tetani*, which can manifest long after initial exposure to contaminated soil or wounds.
In conclusion, resting spores are not inherently infectious in their dormant state but pose a significant risk once they germinate. Their remarkable durability and ability to persist in adverse conditions necessitate targeted strategies for prevention and control. By understanding their definition and characteristics, individuals and industries can implement effective measures to mitigate the threat of spore-related infections, ensuring safer environments and healthier outcomes.
Fern Spores: Mitosis or Meiosis? Unraveling the Reproduction Mystery
You may want to see also

Infectivity potential of resting spores
Resting spores, often produced by bacteria and fungi, are renowned for their resilience in harsh conditions. These dormant forms can survive extreme temperatures, desiccation, and chemical exposure, making them a significant concern in various environments, from healthcare settings to food production. However, their infectivity potential is not uniform; it depends on factors like species, environmental triggers, and host susceptibility. Understanding this potential is crucial for implementing effective control measures.
Consider *Clostridioides difficile*, a bacterium that forms resting spores capable of causing severe intestinal infections. These spores can persist on surfaces for months, and as few as 10 spores are sufficient to establish infection in susceptible individuals, particularly those with compromised gut microbiota. In healthcare settings, rigorous disinfection protocols, such as using chlorine-based cleaners, are essential to inactivate these spores. For instance, a 10% bleach solution (5,000 ppm chlorine) is recommended for surfaces contaminated with *C. difficile* spores, with a contact time of at least 10 minutes.
In contrast, fungal resting spores, such as those of *Aspergillus* species, exhibit varying infectivity based on host immunity. Immunocompromised individuals, including those undergoing chemotherapy or living with HIV, are at higher risk of developing aspergillosis from inhaling these spores. For example, agricultural workers exposed to *Aspergillus* spores in moldy hay or grain are advised to wear N95 respirators to reduce inhalation risk. Practical tips include maintaining indoor humidity below 50% to discourage fungal growth and promptly addressing water damage in buildings.
Comparatively, bacterial resting spores like those of *Bacillus anthracis* (causative agent of anthrax) pose a unique threat due to their aerosolization potential. Inhalation of as few as 8,000–50,000 spores can lead to inhalational anthrax, a condition with a high mortality rate if untreated. This highlights the importance of biosecurity measures in laboratories and agricultural settings. For instance, autoclaving at 121°C for 30 minutes is effective in destroying these spores, ensuring safe disposal of contaminated materials.
In conclusion, the infectivity potential of resting spores varies widely, influenced by species-specific traits and environmental conditions. Tailored strategies, such as targeted disinfection, personal protective equipment, and environmental controls, are essential to mitigate risks. Whether in healthcare, agriculture, or industrial settings, understanding these nuances enables proactive management of spore-related threats.
Does Bleach Kill Mold Spores? Uncovering the Truth Behind the Myth
You may want to see also

Environmental triggers for spore activation
Resting spores, often dormant and resilient, can remain inactive for years until specific environmental cues awaken them. These triggers are not random but precise, signaling optimal conditions for growth and survival. Understanding these cues is crucial for managing spore-related risks, whether in healthcare, agriculture, or environmental science.
Analytical Perspective:
Spore activation is a finely tuned response to environmental changes. Key triggers include shifts in temperature, humidity, nutrient availability, and pH levels. For instance, *Bacillus anthracis* spores, responsible for anthrax, require a temperature range of 25–37°C and a moisture level above 90% relative humidity to germinate. Similarly, fungal spores like *Aspergillus* respond to glucose concentrations as low as 0.1% in their environment. These thresholds act as biological switches, ensuring spores awaken only when conditions favor their proliferation. Ignoring these triggers in controlled environments, such as hospitals or food storage facilities, can lead to unintended spore activation and potential outbreaks.
Instructive Approach:
To prevent spore activation, monitor and manipulate environmental factors systematically. Maintain indoor humidity below 60% to inhibit fungal spore germination, and store perishable goods at temperatures under 4°C to suppress bacterial spore activity. For high-risk areas like laboratories, use HEPA filters to reduce airborne spore counts and regularly sanitize surfaces with spore-killing agents like hydrogen peroxide (3–6% concentration). In agriculture, rotate crops to disrupt soil-borne spore cycles and avoid over-fertilization, which can provide excess nutrients that trigger germination. These proactive measures create environments hostile to spore activation.
Comparative Insight:
Unlike bacterial spores, fungal spores often require light exposure for activation. For example, *Cladosporium* spores germinate faster under blue light (450–495 nm), while *Alternaria* spores respond to red light (620–750 nm). This photobiological response highlights the diversity of triggers across species. In contrast, bacterial spores like *Clostridium botulinum* are more sensitive to oxygen levels, germinating only in anaerobic conditions. Recognizing these species-specific triggers allows for targeted interventions, such as using UV-C light (254 nm) to inactivate fungal spores in HVAC systems or employing oxygen barriers in food packaging to prevent bacterial spore growth.
Descriptive Narrative:
Imagine a forest floor after a wildfire: the heat has scarred the land, yet within the soil, dormant fungal spores await their cue. As rain soaks the earth, raising moisture levels, and nutrients from ash enrich the soil, these spores sense their moment. Within hours, they germinate, sending hyphae into the soil to decompose debris and regenerate the ecosystem. This natural process illustrates how environmental triggers—moisture, nutrients, and temperature—orchestrate spore activation in harmony with ecological needs. Such resilience underscores the importance of respecting these triggers, whether in preserving ecosystems or preventing spore-related hazards.
Persuasive Argument:
Ignoring environmental triggers for spore activation is not just negligent—it’s dangerous. In healthcare settings, failing to control humidity and temperature can turn sterile environments into breeding grounds for pathogens like *Clostridioides difficile*. In agriculture, overlooking soil conditions can lead to crop losses from fungal blights. Even in homes, damp walls and poor ventilation invite mold spores to colonize, posing health risks to occupants. By prioritizing environmental monitoring and mitigation, we can preempt spore activation, safeguarding health, productivity, and infrastructure. The cost of prevention is minimal compared to the consequences of inaction.
Psychrotrophic Spore Formers: Heat Resistance and Food Safety Concerns
You may want to see also
Explore related products

Health risks associated with resting spores
Resting spores, often dormant and resilient, are not inherently infectious in their dormant state. However, their ability to survive harsh conditions—such as extreme temperatures, desiccation, and chemical exposure—poses significant health risks when they germinate under favorable conditions. For instance, *Clostridioides difficile* spores can persist in hospital environments for months, germinating in the gut to cause severe diarrhea and colitis, particularly in individuals over 65 or those on prolonged antibiotic therapy. Understanding the triggers for spore germination is crucial, as it transforms these seemingly inert structures into active pathogens capable of causing disease.
One of the most critical health risks associated with resting spores is their role in foodborne illnesses. Spores from bacteria like *Bacillus cereus* and *Clostridium perfringens* can contaminate food products, surviving cooking processes due to their heat resistance. When ingested, these spores germinate in the intestinal tract, producing toxins that lead to symptoms such as nausea, vomiting, and abdominal cramps. To mitigate this risk, food handlers should adhere to strict hygiene protocols, including reheating food to at least 75°C (167°F) to ensure spore destruction. Additionally, storing food below 4°C (39°F) can prevent spore germination, though it does not eliminate them.
In healthcare settings, resting spores of *Aspergillus* fungi present a severe threat to immunocompromised patients, such as those undergoing chemotherapy or organ transplants. These spores, ubiquitous in indoor and outdoor environments, can infiltrate hospital ventilation systems and settle in patient rooms. Once inhaled, they germinate in the lungs, causing invasive aspergillosis, a condition with a mortality rate exceeding 50% in high-risk groups. Hospitals must implement HEPA filtration systems and regularly monitor air quality to reduce spore concentrations. Patients should also be educated on avoiding construction sites or areas with visible mold growth, where spore counts are typically higher.
Another overlooked risk is the presence of resting spores in soil and water, particularly in agricultural and recreational settings. *Tetanus* spores, for example, are commonly found in soil and can enter the body through puncture wounds, germinating in anaerobic conditions to produce tetanospasmin, a potent neurotoxin. Vaccination remains the most effective preventive measure, with the CDC recommending tetanus boosters every 10 years for adults. For wound management, thorough cleaning with soap and water, followed by application of a topical antiseptic, can reduce the risk of spore germination and infection.
Finally, the health risks of resting spores extend to occupational hazards, particularly for workers in industries like agriculture, construction, and waste management. Prolonged exposure to spore-laden dust can lead to respiratory conditions such as hypersensitivity pneumonitis or farmer’s lung. Employers should provide personal protective equipment, including N95 respirators, and ensure proper ventilation in workspaces. Workers should also practice good hygiene, such as showering and changing clothes after exposure to potentially contaminated environments. By addressing these specific risks, individuals and organizations can minimize the dangers posed by resting spores in various contexts.
Pollen Spores vs. Eggs: Unraveling the Botanical Mystery
You may want to see also

Methods to prevent spore-related infections
Resting spores, such as those produced by bacteria like *Clostridioides difficile* and fungi like *Aspergillus*, can survive harsh conditions and remain dormant for years, posing a significant infection risk when activated. Preventing spore-related infections requires a multi-faceted approach targeting both environmental control and personal protection.
Environmental Decontamination: The Foundation of Prevention
Spores resist common disinfectants like alcohol-based cleaners, necessitating specialized methods. For healthcare settings, chlorine-based solutions (e.g., 5,000–10,000 ppm sodium hypochlorite) are effective against bacterial spores, but require contact times of 10–30 minutes. Hydrogen peroxide vapor systems and UV-C light are increasingly used for terminal room disinfection, achieving >99.99% spore reduction. In homes, mold spore control involves fixing leaks, maintaining humidity below 50%, and using HEPA filters to trap airborne particles.
Personal Protective Measures: Breaking the Transmission Chain
In high-risk environments, such as construction sites or healthcare facilities, wearing N95 respirators prevents inhalation of airborne spores. For skin protection, gloves and gowns act as barriers, particularly when handling contaminated materials. Hand hygiene remains critical but must use spore-active agents like chlorhexidine gluconate (4%) or chlorine-based handwashes, as alcohol sanitizers are ineffective against spores.
Pharmaceutical Interventions: Targeted and Prophylactic Strategies
Antifungal drugs like posaconazole (dosage: 300 mg/day for adults) or voriconazole (400 mg twice daily) are used prophylactically in immunocompromised patients at risk of *Aspergillus* infection. For *C. difficile*, fidaxomicin (200 mg twice daily for 10 days) is spore-suppressing, reducing recurrence rates by 15% compared to vancomycin. Vaccines, though still in development, hold promise for preventing spore-forming pathogens like *Bacillus anthracis*.
Behavioral and Occupational Practices: Reducing Exposure
In agriculture and construction, wetting soil or debris before disturbance minimizes spore aerosolization. Workers should shower and change clothes post-exposure to avoid carrying spores home. Food safety protocols, such as pressure-cooking (15 psi for 20–30 minutes) or autoclaving (121°C for 15–30 minutes), destroy spores in canned goods, preventing botulism.
By combining environmental, personal, pharmaceutical, and behavioral strategies, spore-related infections can be effectively mitigated, even in high-risk settings. Each method addresses a specific vulnerability in the spore lifecycle, from dormancy to activation, ensuring comprehensive protection.
Do Gram-Negative Bacteria Form Spores? Unraveling the Microbial Mystery
You may want to see also
Frequently asked questions
Resting spores are generally not infectious to humans. They are dormant forms of microorganisms, such as bacteria or fungi, and do not actively cause disease unless they germinate under favorable conditions.
Resting spores can infect plants or animals if they germinate and resume growth under suitable environmental conditions. For example, fungal resting spores can cause plant diseases when they activate.
Resting spores can remain viable for extended periods, sometimes years or decades, but they are not infectious until they germinate and return to an active, growing state.
Resting spores can be a concern in food safety, particularly for heat-resistant bacterial spores like *Clostridium botulinum*. While not infectious in their dormant state, they can germinate and produce toxins if conditions allow.































