Fungal spores, microscopic reproductive units produced by fungi, are ubiquitous in the environment and can have significant impacts on human health. While many fungi are harmless or even beneficial, certain species release spores that, when inhaled or come into contact with the skin, can trigger a range of health issues. For individuals with compromised immune systems, allergies, or pre-existing respiratory conditions, fungal spores may exacerbate symptoms or lead to severe infections such as aspergillosis or candidiasis. Additionally, prolonged exposure to mold spores in indoor environments has been linked to respiratory problems, allergic reactions, and even mental health issues. Understanding the role of fungal spores in human health is crucial for developing strategies to mitigate their adverse effects and promote public well-being.
| Characteristics | Values |
|---|---|
| Can fungal spores influence human health? | Yes |
| Mechanism of Influence | 1. Allergic Reactions: Spores can trigger asthma, allergic rhinitis, and hypersensitivity pneumonitis. 2. Infectious Diseases: Some spores can cause infections, especially in immunocompromised individuals (e.g., aspergillosis, candidiasis, cryptococcosis). 3. Toxigenic Effects: Certain fungi produce mycotoxins (e.g., aflatoxins, ochratoxins) that can contaminate food and cause acute or chronic toxicity. 4. Inflammatory Responses: Spores can induce inflammation in the respiratory tract and other tissues. |
| Common Fungal Spores of Concern | Aspergillus, Penicillium, Cladosporium, Alternaria, Candida, Cryptococcus, Stachybotrys (black mold) |
| At-Risk Populations | Immunocompromised individuals, asthma patients, individuals with chronic respiratory conditions, infants, elderly, and those with occupational exposure (e.g., farmers, construction workers) |
| Environmental Sources | Indoor environments (damp buildings, HVAC systems), outdoor air, soil, decaying organic matter, contaminated food |
| Prevention and Control | 1. Moisture Control: Prevent mold growth by fixing leaks and reducing humidity. 2. Ventilation: Improve air circulation in indoor spaces. 3. Personal Protective Equipment (PPE): Use masks and gloves in high-risk environments. 4. Regular Cleaning: Remove mold and fungal growth promptly. 5. Food Safety: Avoid consuming moldy food and store food properly. |
| Health Impact Severity | Ranges from mild allergic reactions to life-threatening infections (e.g., invasive aspergillosis) |
| Global Health Burden | Significant, especially in regions with poor housing conditions, agricultural exposure, and high humidity |
| Research and Monitoring | Ongoing studies to understand spore dispersal, mycotoxin exposure, and development of antifungal therapies |
Explore related products
What You'll Learn
- Fungal spore allergies and respiratory issues in susceptible individuals
- Indoor mold exposure linked to chronic health problems
- Fungal infections from spore inhalation in immunocompromised people
- Toxic spores causing systemic illnesses like aflatoxicosis
- Beneficial fungal spores in probiotics and gut health

Fungal spore allergies and respiratory issues in susceptible individuals
Fungal spores are ubiquitous in the environment, and for susceptible individuals, they can trigger a cascade of allergic reactions and respiratory issues. These microscopic particles, often inhaled unknowingly, can lead to symptoms ranging from mild nasal congestion to severe asthma exacerbations. Understanding the mechanisms behind these reactions is crucial for effective management and prevention.
Consider the case of *Alternaria alternata*, a common fungal spore found in outdoor environments, particularly in damp areas. Studies show that sensitivity to this spore is prevalent in up to 70% of individuals with mold allergies. When inhaled, *Alternaria* spores can provoke an immune response, causing airway inflammation and constriction. For asthmatics, this can result in wheezing, shortness of breath, and even life-threatening attacks. A 2019 study published in *The Journal of Allergy and Clinical Immunology* found that exposure to *Alternaria* spores increased the risk of asthma exacerbations by 30% in susceptible populations. Practical tips for reducing exposure include keeping indoor humidity below 50%, using air purifiers with HEPA filters, and avoiding outdoor activities during high spore count seasons, typically late summer and early fall.
Analyzing the role of fungal spores in respiratory health reveals a complex interplay between environmental exposure and individual susceptibility. Unlike pollen allergies, which are often seasonal, fungal spore allergies can persist year-round, especially in regions with high humidity or in water-damaged buildings. Indoor fungal growth, often hidden behind walls or under carpets, can release spores continuously, posing a chronic risk. For children and the elderly, whose immune systems are more vulnerable, prolonged exposure can lead to recurrent respiratory infections or chronic sinusitis. A proactive approach involves regular inspection of homes for mold, prompt repair of leaks, and professional mold remediation when necessary.
Persuasively, it’s essential to recognize that fungal spore allergies are not merely a nuisance but a significant public health concern. Misdiagnosis or neglect can lead to long-term complications, including bronchiectasis or fungal colonization of the airways. Allergy testing, such as skin prick tests or specific IgE blood tests, can identify sensitivities to common fungal spores like *Cladosporium* or *Aspergillus*. Once diagnosed, immunotherapy, such as subcutaneous or sublingual allergy shots, can desensitize the immune system, reducing symptom severity over time. For acute symptoms, antihistamines, nasal corticosteroids, and bronchodilators are effective in managing inflammation and airway obstruction.
Comparatively, while fungal spore allergies share similarities with other respiratory allergies, their management requires a tailored approach. Unlike pollen, fungal spores thrive in both indoor and outdoor environments, necessitating comprehensive environmental control measures. For instance, while pollen allergies benefit from closing windows during high-count seasons, fungal spore allergies require active measures like dehumidification and ventilation. Additionally, fungal spores can colonize the sinuses, leading to allergic fungal sinusitis, a condition that often requires surgical intervention in addition to antifungal therapy. This highlights the need for a multidisciplinary approach involving allergists, pulmonologists, and otolaryngologists.
In conclusion, fungal spore allergies and respiratory issues in susceptible individuals demand awareness, early intervention, and targeted management. By understanding the specific triggers, implementing environmental controls, and utilizing appropriate medical therapies, individuals can mitigate the impact of these allergens on their health. Whether through simple home modifications or advanced immunotherapy, proactive steps can significantly improve quality of life and prevent long-term complications.
Do Only Select Bacilli Species Produce Spores? Exploring Bacterial Diversity
You may want to see also

Indoor mold exposure linked to chronic health problems
Indoor mold exposure is a silent intruder that can significantly impact human health, often going unnoticed until symptoms become chronic. Mold spores, microscopic and ubiquitous, thrive in damp, humid environments, making indoor spaces like bathrooms, basements, and poorly ventilated areas their ideal breeding grounds. When inhaled, these spores can trigger a cascade of health issues, particularly in individuals with pre-existing conditions or weakened immune systems. For instance, prolonged exposure to mold has been linked to respiratory conditions such as asthma, chronic sinusitis, and bronchitis. Studies show that children and the elderly are especially vulnerable, with prolonged exposure increasing the risk of developing allergies and respiratory infections by up to 30-50%.
Analyzing the mechanisms behind mold-related health problems reveals a complex interplay between fungal spores and the human body. Mold releases mycotoxins, toxic substances that can irritate the lungs, skin, and mucous membranes. Even low-level exposure over time can lead to systemic inflammation, contributing to conditions like chronic fatigue syndrome and fibromyalgia. A 2019 study published in the *Journal of Occupational and Environmental Medicine* found that individuals exposed to indoor mold had a 40% higher likelihood of experiencing persistent headaches and cognitive difficulties. These findings underscore the importance of addressing mold issues promptly, as the cumulative effects of exposure can be insidious and debilitating.
Practical steps to mitigate indoor mold exposure are essential for safeguarding health. Start by controlling indoor humidity levels, ideally keeping them below 50% using dehumidifiers or air conditioners. Regularly inspect areas prone to moisture, such as under sinks, around windows, and in attics, and address leaks or water damage immediately. For visible mold growth covering less than 10 square feet, homeowners can clean it using a solution of one cup of bleach per gallon of water, wearing protective gear like gloves and masks. However, for larger infestations or mold in HVAC systems, professional remediation is recommended to prevent spore dispersal.
Comparing the health impacts of indoor mold exposure to other environmental hazards highlights its unique challenges. Unlike pollutants like lead or asbestos, mold is biological and can grow rapidly under the right conditions, making it difficult to eradicate completely. Additionally, while lead poisoning primarily affects children, mold-related health issues span all age groups, though symptoms may manifest differently. For example, children may experience frequent respiratory infections, while adults might develop persistent skin rashes or joint pain. This broad spectrum of effects necessitates a proactive approach to mold prevention and management.
In conclusion, indoor mold exposure is a significant yet often overlooked contributor to chronic health problems. By understanding the risks, recognizing early signs of mold growth, and taking preventive measures, individuals can reduce their exposure and protect their well-being. Regular maintenance, proper ventilation, and prompt remediation are key strategies in combating this hidden health threat. As awareness grows, so too does the potential to create healthier indoor environments, free from the pervasive influence of fungal spores.
Do Plants Produce Spores Through Meiosis? Unraveling the Process
You may want to see also

Fungal infections from spore inhalation in immunocompromised people
Fungal spores are ubiquitous in the environment, silently drifting through the air we breathe. For most healthy individuals, inhaling these microscopic particles poses little threat, as the immune system efficiently neutralizes them. However, for immunocompromised individuals—those with weakened immune systems due to conditions like HIV/AIDS, cancer treatments, organ transplants, or autoimmune diseases—these spores can become formidable adversaries. Inhalation of fungal spores in this population can lead to severe, often life-threatening infections, such as aspergillosis, cryptococcosis, or pneumocystis pneumonia. Understanding the risks and mechanisms of these infections is critical for prevention and early intervention.
Consider the case of *Aspergillus fumigatus*, a common mold found in soil and decaying organic matter. Its spores are inhaled daily by nearly everyone, yet they rarely cause harm. In immunocompromised individuals, however, these spores can germinate in the lungs, leading to invasive aspergillosis. This infection progresses rapidly, causing symptoms like fever, cough, chest pain, and difficulty breathing. Diagnosis is challenging, often requiring imaging studies or invasive procedures like bronchoscopy. Treatment typically involves antifungal medications such as voriconazole, but success rates are lower in immunocompromised patients due to their reduced ability to mount an immune response. For example, studies show that invasive aspergillosis has a mortality rate of up to 90% in untreated hematopoietic stem cell transplant recipients.
Prevention is paramount for this vulnerable population. Practical steps include minimizing exposure to environments with high fungal spore concentrations, such as construction sites, gardens, or areas with visible mold. Wearing N95 masks in such settings can reduce inhalation risk. Indoor air quality is equally important; using HEPA filters and maintaining low humidity levels (below 50%) can inhibit mold growth. For high-risk individuals, healthcare providers may prescribe prophylactic antifungal medications, such as posaconazole, during periods of severe immunosuppression. Regular monitoring for early signs of infection, including routine chest imaging and serum biomarker tests like galactomannan, can also improve outcomes.
Comparatively, *Pneumocystis jirovecii* pneumonia (PJP) is another spore-related infection that disproportionately affects immunocompromised individuals, particularly those with advanced HIV/AIDS. Unlike molds, *Pneumocystis* is a fungus-like organism that colonizes the lungs asymptomatically in many people. In those with CD4 cell counts below 200 cells/μL, it can cause severe pneumonia, characterized by hypoxia and a non-productive cough. Prophylaxis with medications like trimethoprim-sulfamethoxazole (TMP-SMX) is standard for at-risk patients, reducing PJP incidence by up to 90%. Despite this, breakthrough infections can occur, especially with drug resistance or non-adherence. Early recognition and treatment with high-dose TMP-SMX or alternative agents like pentamidine are essential to prevent respiratory failure.
In conclusion, fungal spores pose a significant but often overlooked threat to immunocompromised individuals. While healthy immune systems effectively combat these invaders, weakened defenses can allow spores to establish devastating infections. Through a combination of environmental precautions, prophylactic measures, and vigilant monitoring, the risk of spore-related fungal infections can be mitigated. For healthcare providers and patients alike, awareness and proactive management are key to safeguarding this vulnerable population.
Can Fern Spores Trigger Allergies? Uncovering the Hidden Culprit
You may want to see also
Explore related products

Toxic spores causing systemic illnesses like aflatoxicosis
Fungal spores, often invisible to the naked eye, can harbor potent toxins capable of triggering systemic illnesses in humans. Among these, aflatoxicosis stands out as a severe condition caused by aflatoxins, metabolites produced by certain strains of *Aspergillus* fungi. These toxins contaminate staple crops like maize, peanuts, and tree nuts, particularly in warm and humid climates where fungal growth thrives. Ingesting even small amounts of aflatoxin-contaminated food can lead to acute or chronic health issues, making it a global health concern, especially in developing regions with limited food safety infrastructure.
Aflatoxins are among the most carcinogenic substances known, with aflatoxin B1 being the most potent. Prolonged exposure, even at low levels, increases the risk of liver cancer, particularly in individuals with hepatitis B or C infections. Acute aflatoxicosis, though rare, can occur after consuming heavily contaminated food, causing symptoms like nausea, abdominal pain, and jaundice. In severe cases, it can lead to liver failure and death within days. Vulnerable populations, including children and those with compromised immune systems, are at higher risk due to their lower body mass and weaker detoxification mechanisms.
Preventing aflatoxicosis requires a multi-faceted approach. Farmers can reduce contamination by properly drying and storing crops, using resistant crop varieties, and implementing good agricultural practices. Consumers should inspect grains and nuts for mold, discard visibly spoiled food, and diversify their diet to minimize repeated exposure from a single source. Regulatory bodies play a critical role by setting and enforcing aflatoxin limits in food (e.g., the FDA’s 20 ppb limit in the U.S.). In regions with high contamination risk, post-harvest interventions like aflatoxin-binding agents or biocontrol products can mitigate toxin levels.
Comparatively, aflatoxicosis highlights the broader issue of mycotoxin-related illnesses, yet it remains distinct due to its severe health outcomes and widespread impact. Unlike other fungal toxins that primarily cause localized reactions, aflatoxins target vital organs, underscoring the need for targeted prevention strategies. While efforts to reduce aflatoxin exposure are advancing, challenges persist, particularly in resource-limited settings. Public awareness, coupled with technological innovations and policy support, is essential to combat this silent yet deadly threat.
Purple Spore Prints: Are Any Poisonous Mushrooms Hiding in This Hue?
You may want to see also

Beneficial fungal spores in probiotics and gut health
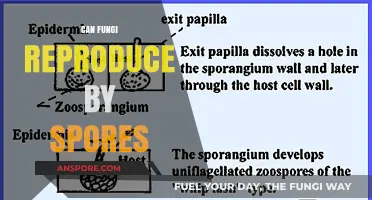
Fungal spores, often associated with allergens or infections, also play a transformative role in gut health when harnessed as probiotics. Unlike bacterial strains, fungal spores—such as those from *Saccharomyces boulardii*—are resilient to stomach acid and antibiotics, ensuring they reach the intestines intact. This unique survival advantage positions them as reliable agents for restoring microbial balance, particularly after antibiotic-induced disruptions or gastrointestinal disorders like diarrhea.
Consider the mechanism: *S. boulardii* spores compete with harmful pathogens for resources, produce enzymes that break down toxins, and stimulate the gut lining to secrete protective mucus. Clinical studies show that a daily dose of 500–1,000 mg (typically 5–10 billion CFUs) can reduce the duration of antibiotic-associated diarrhea by up to 25%. For children over 3 years, a lower dose of 250 mg is recommended, though consultation with a pediatrician is essential. This specificity in action and dosing underscores the precision with which fungal spores can be employed.
However, not all fungal spores are created equal. While *S. boulardii* is widely studied and deemed safe for most age groups, other fungal strains lack sufficient research. For instance, *Aspergillus* or *Candida* spores, though naturally present in the gut, can become opportunistic pathogens in immunocompromised individuals. Thus, selecting spore-based probiotics requires scrutiny—opt for products with transparent sourcing and third-party testing to avoid contamination risks.
Integrating fungal spore probiotics into a routine demands awareness of timing and context. Take them at least 2 hours apart from antibiotics to prevent competition for absorption. Pairing them with prebiotic fibers like inulin or pectin amplifies their efficacy by fueling beneficial microbes. For those with fungal sensitivities or conditions like SIBO (small intestinal bacterial overgrowth), a gradual introduction under medical supervision is critical to avoid adverse reactions.
The takeaway is clear: fungal spores are not a one-size-fits-all solution but a targeted tool for gut health. When chosen wisely and used strategically, they offer a robust complement to traditional probiotics, particularly in challenging microbial landscapes. As research evolves, their role in modulating immunity, metabolism, and even mental health via the gut-brain axis may unveil further applications, solidifying their place in the probiotic arsenal.
Breathing Fungal Spores: Uncovering Potential Health Risks and Concerns
You may want to see also
Frequently asked questions
Yes, fungal spores can cause respiratory issues, especially in individuals with weakened immune systems, asthma, or allergies. Inhaling spores from molds like *Aspergillus* or *Histoplasma* can lead to conditions such as allergic reactions, asthma exacerbations, or fungal infections like aspergillosis or histoplasmosis.
Fungal spores are not harmful to everyone, but certain groups are more vulnerable. These include individuals with compromised immune systems (e.g., HIV/AIDS, cancer patients), chronic lung diseases, allergies, or those undergoing immunosuppressive treatments. Healthy individuals are less likely to experience severe health effects.
Yes, fungal spores in food, particularly from molds like *Aspergillus*, *Penicillium*, or *Fusarium*, can produce toxic compounds called mycotoxins. Ingesting contaminated food can lead to acute or chronic health issues, including gastrointestinal problems, liver damage, or even cancer, depending on the type and amount of mycotoxin consumed.
Exposure to fungal spores can be minimized by maintaining clean and dry indoor environments to prevent mold growth, using air filters or purifiers, avoiding areas with high fungal spore counts (e.g., damp basements), and properly storing food to prevent mold contamination. Wearing masks in dusty or moldy environments can also reduce inhalation risk.