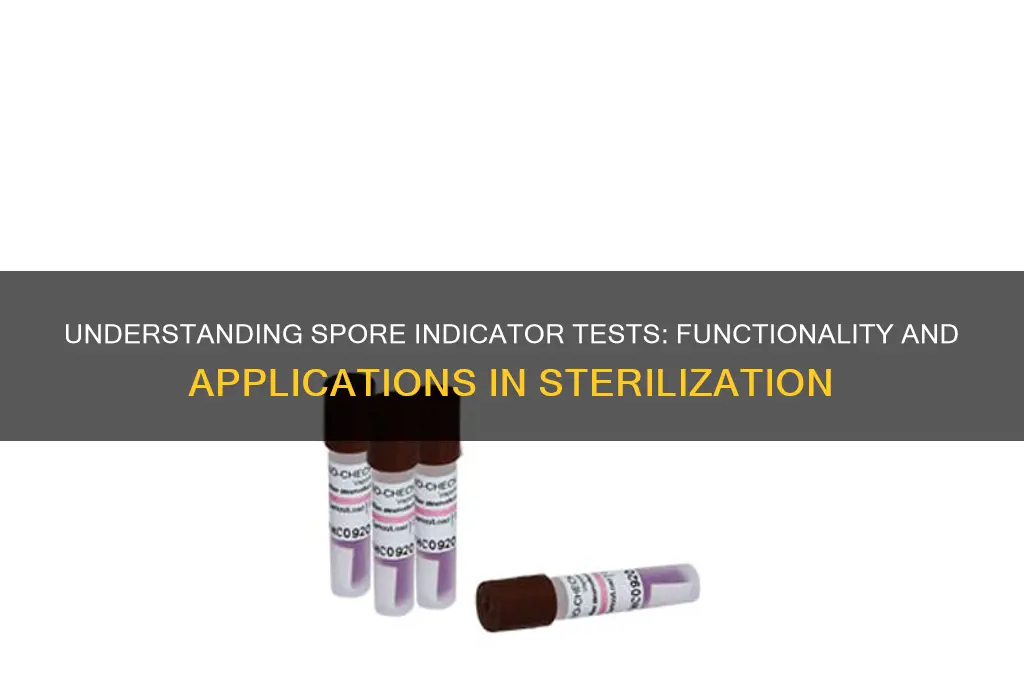
Spore indicator tests are a critical method used in sterilization processes to verify the effectiveness of sterilization equipment, particularly in healthcare, pharmaceutical, and laboratory settings. These tests utilize biological indicators containing highly resistant bacterial spores, such as *Geobacillus stearothermophilus* or *Bacillus atrophaeus*, which are more challenging to kill than most microorganisms. The spores are exposed to the sterilization process, and after completion, the indicator is incubated to determine if any spores survived. If no growth is detected, the sterilization cycle is considered successful; however, if growth occurs, it indicates that the sterilization process was inadequate. This method provides a reliable and direct measure of the sterilizer’s ability to kill microorganisms, ensuring safety and compliance with regulatory standards.
| Characteristics | Values |
|---|---|
| Purpose | To test the effectiveness of sterilization processes by detecting spore survival. |
| Target Organisms | Highly resistant bacterial spores (e.g., Geobacillus stearothermophilus for steam sterilization, Bacillus atrophaeus for dry heat). |
| Indicator Type | Biological indicators (live spores) vs. chemical indicators (color-changing strips). |
| Mechanism | Spores are exposed to the sterilization process; survival indicates process failure. |
| Readout Method | Incubation of spores post-sterilization to check for growth (e.g., turbidity, color change, or fluorescence). |
| Incubation Time | Typically 24–48 hours at 55–60°C (varies by spore species and test system). |
| Sensitivity | Detects as few as 1 surviving spore per test, ensuring high accuracy. |
| Applications | Autoclaves, ethylene oxide (EO) sterilizers, hydrogen peroxide gas plasma, and other sterilization methods. |
| Advantages | Direct measure of sterilization efficacy; more reliable than chemical indicators. |
| Limitations | Requires incubation time; cannot provide immediate results. |
| Standards Compliance | ISO 11138, ISO 14161, and other regulatory guidelines for validation. |
| Storage Requirements | Spores must be stored under controlled conditions (e.g., refrigerated) to maintain viability. |
| Interpretation | Growth = sterilization failure; no growth = process likely successful. |
| Common Formats | Self-contained vials, strips, or ampules with growth media and spores. |
| Validation Frequency | Regular testing (e.g., daily or per cycle) in healthcare and pharmaceutical settings. |
Explore related products
$140.08
What You'll Learn
- Spore Indicator Basics: Understand what spores are and why they're ideal for sterilization process validation
- Indicator Construction: Learn about the materials and design of spore indicator strips
- Sterilization Exposure: How spores are exposed to sterilization processes like steam or gas
- Incubation & Growth: The process of incubating exposed spores to detect surviving microorganisms
- Result Interpretation: Reading and interpreting test results to determine sterilization effectiveness

Spore Indicator Basics: Understand what spores are and why they're ideal for sterilization process validation
Spores, the dormant forms of certain bacteria, are nature's ultimate survivalists. Encased in a tough, protective coat, they can withstand extreme conditions—heat, radiation, and chemicals—that would destroy their active counterparts. This resilience makes them both a challenge and an ideal tool for validating sterilization processes. When exposed to sterilization methods like autoclaving or chemical disinfectants, spores serve as the gold standard for testing efficacy because if they are eliminated, it’s a strong indicator that other, less resilient microorganisms have also been eradicated.
To understand why spores are perfect for this role, consider their biological design. Unlike vegetative bacteria, spores have a significantly reduced metabolic rate and a robust outer layer that resists penetration by sterilants. For instance, *Geobacillus stearothermophilus* spores, commonly used in spore indicator tests, require exposure to 121°C for at least 20 minutes in a steam autoclave to be reliably killed. This high resistance ensures that if the sterilization process fails to eliminate spores, it’s unlikely to be effective against other pathogens, making them a critical benchmark for process validation.
Spore indicator tests are designed to mimic the presence of contaminants in a real-world setting. These tests typically use spore strips or ampules containing a known quantity of spores, often in the range of 10^5 to 10^6 colony-forming units (CFUs). After exposure to the sterilization process, the indicators are incubated under optimal growth conditions (e.g., 55–60°C for *G. stearothermophilus* spores) to determine if any spores survived. If growth is detected, the sterilization cycle is considered a failure, prompting an investigation into the process or equipment.
The choice of spore species in these tests is not arbitrary. *Bacillus atrophaeus* spores, for example, are used for dry heat and ethylene oxide sterilization validation, while *G. stearothermophilus* is preferred for steam and vaporized hydrogen peroxide processes. This specificity ensures that the test accurately reflects the challenges posed by different sterilization methods. For healthcare facilities, using the correct spore species is critical, as regulatory bodies like the FDA and CDC mandate rigorous validation protocols to ensure patient safety.
In practice, spore indicator tests are a cornerstone of quality control in industries ranging from healthcare to pharmaceuticals. They provide a clear, binary result—pass or fail—that leaves no room for ambiguity. For instance, in a hospital setting, daily autoclave testing with spore strips ensures that surgical instruments are safe for use. Similarly, in pharmaceutical manufacturing, spore tests validate that sterile products meet regulatory standards. By leveraging the unique properties of spores, these tests offer a reliable, scientifically grounded method to confirm that sterilization processes are effective, protecting both patients and products from microbial contamination.
Does Crossing Over in Meiosis Occur in Spores? Exploring Genetic Recombination
You may want to see also

Indicator Construction: Learn about the materials and design of spore indicator strips
Spore indicator strips are precision tools, and their effectiveness hinges on meticulous construction. At their core lies a carrier material, typically a strip of filter paper or non-woven fabric, chosen for its ability to absorb and retain spores while allowing for even distribution of sterilant. This base is then inoculated with a specific dosage of highly resistant spores, often ranging from 10^5 to 10^6 spores per strip. The most common spore species used is Geobacillus stearothermophilus, renowned for its resilience to steam sterilization.
Adhesive plays a crucial role, securing the spore inoculum to the carrier material. This adhesive must be sterilization-resistant itself, ensuring it doesn't degrade or interfere with the spore viability during the testing process.
The design of spore indicator strips prioritizes visibility and interpretation. After exposure to the sterilant, the spores undergo a colorimetric change, typically from beige to black, indicating successful spore destruction. This visual transformation is achieved through the incorporation of pH-sensitive dyes within the spore inoculum. These dyes react to the metabolic byproducts produced by surviving spores, providing a clear and unambiguous result.
Control lines, often present on the strip, serve as a reference point, ensuring the test has functioned correctly regardless of the sterilization outcome.
While seemingly simple, the construction of spore indicator strips demands rigorous quality control. The spore dosage must be uniform and accurate, ensuring consistent test results. The carrier material and adhesive must be free from contaminants that could interfere with spore viability or the colorimetric reaction. Each batch of indicators undergoes stringent testing to verify sterility, spore viability, and colorimetric response, guaranteeing their reliability in critical sterilization processes.
Proper handling and storage are equally vital. Spore indicators should be stored in cool, dry conditions to maintain spore viability and prevent premature degradation of the colorimetric components.
In essence, the construction of spore indicator strips is a delicate balance of material science, microbiology, and engineering. Each component, from the carrier material to the colorimetric dye, is carefully selected and integrated to create a reliable tool for verifying sterilization efficacy. Understanding these intricacies highlights the sophistication behind these seemingly simple strips, underscoring their crucial role in ensuring patient safety and product quality.
Can Fungus Spores Survive on Rubber Surfaces? Uncovering the Truth
You may want to see also

Sterilization Exposure: How spores are exposed to sterilization processes like steam or gas
Spores, the resilient survival structures of certain bacteria, are the gold standard for testing sterilization processes. Their ability to withstand extreme conditions makes them ideal challengers for steam, gas, and other sterilization methods. Exposing spores to these processes is a critical step in spore indicator tests, ensuring the effectiveness of sterilization in healthcare, pharmaceuticals, and food production.
Here's a breakdown of how this exposure works:
Direct Immersion: The most common method involves placing spore-impregnated carriers directly into the sterilization chamber. For steam sterilization (autoclaving), this means subjecting the spores to saturated steam at temperatures typically ranging from 121°C to 134°C for specific time intervals, often 15-30 minutes. In gas sterilization, spores are exposed to ethylene oxide gas at controlled concentrations and humidity levels for several hours.
Challenges and Variables: The effectiveness of spore exposure hinges on precise control of parameters. In steam sterilization, factors like temperature, pressure, and exposure time are crucial. Even slight deviations can allow spores to survive. Gas sterilization adds complexity with variables like gas concentration, humidity, and exposure duration. These factors must be meticulously monitored and documented to ensure reliable results.
Post-Exposure Analysis: After exposure, the spores undergo incubation in a nutrient-rich medium. If the sterilization process was successful, the spores will not germinate, indicating effective sterilization. Any visible growth signifies surviving spores, highlighting potential issues with the sterilization process.
Practical Considerations: Choosing the right spore species is vital. Bacillus atrophaeus and Geobacillus stearothermophilus are commonly used due to their resistance to heat and chemicals, respectively. Additionally, proper placement of spore indicators within the sterilization chamber is essential to ensure representative exposure.
This meticulous process of exposing spores to sterilization agents forms the backbone of spore indicator tests, providing a reliable and quantifiable measure of sterilization efficacy. By simulating real-world conditions and analyzing spore survival, these tests safeguard against the presence of harmful microorganisms, ensuring the safety of critical products and processes.
Using Spore Syringes on Agar Dishes: Techniques and Best Practices
You may want to see also
Explore related products

Incubation & Growth: The process of incubating exposed spores to detect surviving microorganisms
Spores, the resilient survival forms of certain bacteria, can withstand extreme conditions, including sterilization processes. Incubating exposed spores is a critical step in spore indicator tests, designed to detect any surviving microorganisms that may pose a risk in healthcare, food production, or pharmaceutical settings. This process involves creating an environment conducive to spore germination and bacterial growth, allowing for the identification of even a single surviving spore.
The Incubation Process: Imagine a petri dish containing a nutrient-rich agar medium, specifically formulated to support bacterial growth. This medium is inoculated with the sample containing potentially exposed spores. The dish is then sealed and placed in an incubator, a controlled environment maintaining optimal temperature and humidity. For most bacterial spores, this means a temperature range of 30-35°C (86-95°F) and high humidity to prevent desiccation. Incubation times vary depending on the target organism, but typically range from 24 to 72 hours.
During incubation, any viable spores will germinate, shedding their protective coats and transforming into actively growing bacteria. These bacteria will then multiply, forming visible colonies on the agar surface. The size, shape, and color of these colonies can provide clues about the type of bacteria present.
Interpreting Results: After the incubation period, the petri dish is examined for colony growth. The presence of colonies indicates that spores survived the sterilization process, highlighting a potential breach in sterilization efficacy. The number and characteristics of colonies provide valuable information. A high number of colonies suggests a significant contamination risk, while a few scattered colonies may indicate a minor issue.
Critical Considerations: It's crucial to maintain strict aseptic technique throughout the incubation process to prevent contamination from external sources. Additionally, using appropriate positive and negative controls is essential for accurate interpretation of results. Positive controls, containing known spore-forming bacteria, confirm the test's sensitivity, while negative controls, devoid of spores, ensure the absence of contamination.
Practical Applications: Incubation and growth are fundamental to various spore indicator tests, including biological indicators used in autoclave validation and spore strip tests for surface disinfection. These tests are vital for ensuring the safety and efficacy of sterilization processes in diverse industries, ultimately protecting public health and product quality. By understanding the intricacies of incubation and growth, we can effectively detect and address potential microbial threats.
Milky Spore's Impact on Fireflies: Uncovering the Truth
You may want to see also

Result Interpretation: Reading and interpreting test results to determine sterilization effectiveness
Interpreting spore indicator test results is a critical step in ensuring sterilization effectiveness, as it directly reflects the ability of the sterilization process to eliminate highly resistant bacterial spores. These tests typically use Geobacillus stearothermophilus spores for steam sterilization (autoclaving) and Bacillus atrophaeus spores for dry heat or ethylene oxide (EtO) sterilization. The process involves exposing a spore strip or vial to the sterilization cycle, followed by incubation to detect spore survival. A color change from purple to yellow in a self-contained biological indicator (BI) or visible growth in a culture medium indicates spore survival, signaling sterilization failure. Conversely, no color change or growth confirms effective sterilization.
To accurately interpret results, follow these steps: first, ensure the BI or spore strip is correctly processed according to manufacturer instructions, including precise incubation times (e.g., 24–48 hours at 55–60°C for Geobacillus stearothermophilus). Second, document the result immediately, noting any anomalies such as partial color change or delayed growth, which may suggest marginal sterilization efficacy. Third, correlate the result with the sterilization cycle parameters (e.g., temperature, pressure, duration) to identify potential deviations. For instance, a failed test in a steam autoclave might indicate insufficient temperature or exposure time, while a failed EtO test could point to inadequate gas concentration or humidity levels.
A comparative analysis of positive and negative results highlights the importance of process validation. A positive result (spore survival) mandates immediate corrective action, such as reprocessing the load, inspecting the sterilizer, and reviewing operator protocols. A negative result (no spore survival) confirms compliance but should not replace routine monitoring. For example, a hospital sterilization unit might use daily BI tests for autoclaves and weekly tests for EtO sterilizers, ensuring consistent performance over time.
Practical tips for result interpretation include maintaining a logbook to track test outcomes, sterilization cycles, and equipment maintenance. Use control spores (positive controls) to validate the test’s accuracy, ensuring the incubation system is functioning correctly. Additionally, train staff to recognize ambiguous results, such as faint color changes, which may require repeat testing or consultation with the manufacturer. By integrating these practices, healthcare and laboratory facilities can uphold sterilization standards, safeguarding patient safety and regulatory compliance.
Are Bacterial Spore Cells Dead During Staining? Unraveling the Mystery
You may want to see also
Frequently asked questions
A spore indicator test is a method used to validate the effectiveness of sterilization processes, particularly in healthcare and laboratory settings. It measures the ability of a sterilization method (e.g., autoclave, chemical sterilant) to kill highly resistant bacterial spores, such as *Geobacillus stearothermophilus* or *Bacillus atrophaeus*, which are more difficult to eliminate than vegetative bacteria.
Spore indicator tests work by exposing a strip or vial containing bacterial spores to the sterilization process. After the cycle, the spores are incubated in a growth medium. If the sterilization was successful, no spores will survive, and no growth will be observed. If spores are detected, the sterilization process is considered ineffective.
There are two main types: biological indicators (BIs) and chemical indicators (CIs). Biological indicators contain live spores and provide a direct measure of sterilization efficacy, making them the gold standard. Chemical indicators change color or appearance in response to specific sterilization conditions but do not confirm spore kill. BIs are used for routine monitoring and validation, while CIs are used for process monitoring and quick checks.








![SHARS .030" Dial Test Indicator .0005" 303-3209 !]](https://m.media-amazon.com/images/I/61Zy1hTLuRL._AC_UY218_.jpg)







![Shars 0.008" Large Face Dial Test Indicator, .0001" Graduation, 1.5" Face Diameter 303-3210 P]](https://m.media-amazon.com/images/I/613RAMhhRSL._AC_UY218_.jpg)